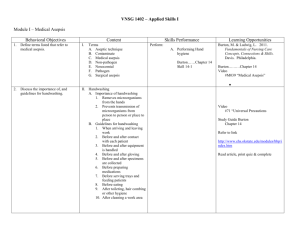
Chap 27: physical assessment Data--Nursing health assessment involves gathering information about the health status of the patient. The nurse then evaluates and synthesizes the information (data). health history is a collection of data that provides a detailed profile of the patient’s health status. Physical assessment is a collection of objective data that provides information about changes in the patient’s body systems. comprehensive health assessment is broad and includes a complete health history and physical assessment. A comprehensive assessment is usually conducted when a patient first enters a health care setting, with information providing a baseline for comparing later assessments. ongoing or partial health assessment, or follow-up assessment, is one that is conducted at regular intervals (e.g., at the beginning of each home health visit or each hospital shift) during care of the patient. This type of assessment concentrates on identified health problems to monitor positive or negative changes and evaluate the effectiveness of interventions. In addition, a brief reassessment of the patient’s body systems and functional abilities is performed to detect any new problems. emergency health assessment is a type of rapid focused assessment conducted when addressing a life-threatening or unstable situation. Assessment of the airway, breathing, and circulation when encountering a patient with traumatic injury as a result of a motor vehicle accident is an example of an emergency assessment. activities of daily living (ADLs) or self-care activities. Eating, bathing, dressing, and toileting are examples of ADLs. instrumental activities of daily living (IADLs) or those activities needed for independent living. Housekeeping, meal preparation, management of finances, and transportation are examples of IADLs. Adventitious breath sounds (extra, abnormal sounds) are not normally heard in the lungs and result from air moving through moisture, mucus, or narrowed airways. Bronchial breath sounds heard over the larynx and trachea are high-pitched, harsh “blowing” sounds, with sound on expiration being longer than inspiration. Bronchovesicular breath sounds are heard over the mainstem bronchus and are moderate blowing sounds, with inspiration equal to expiration. Vesicular breath sounds are soft, low-pitched, whispering sounds, heard over most of the lung fields, with sound on inspiration being longer than expiration. review of systems(ROS)-- The nursing physical assessment involves the examination of all body systems in a systematic manner, commonly using a head-to-toe format; this is called the review of systems (ROS). Four methods are used to collect data during the physical assessment: Inspection: the process of performing deliberate, purposeful observations in a systematic manner. Palpation: use of the sense of touch to assess skin temperature, turgor, texture, and moisture as well as vibrations within the body. Percussion: the act of striking one object against another to produce sound. Auscultation: the act of listening with a stethoscope to sounds produced within the body. Body mass index (BMI) is a ratio of weight to height. BMI is used as an initial assessment of nutritional status and is an indicator of obesity or malnutrition. Waist circumference is the measurement around a patient at the level of the umbilicus and is a good indicator of abdominal fat. Erythema, redness of the skin, is caused by dilation of superficial blood vessels. It is associated with sunburn, inflammation, fever, trauma, and allergic reactions. When assessing for erythema in people with darker skin tones, it is important to assess skin temperature; areas of erythema will feel warm when compared with surrounding skin. Cyanosis is a bluish or grayish discoloration of the skin in response to inadequate oxygenation. Cyanosis is assessed as a blue tinge in patients with lighter skin and as dullness in patients with dark skin tones. Jaundice is a yellow color of the skin resulting from elevated amounts of bilirubin in the blood. It is associated with liver and gallbladder disease, some types of anemia, and excessive hemolysis (breakdown of red blood cells). It usually develops first in the sclera of the eyes and then in the skin and mucous membranes. It is more difficult to observe jaundice on the trunk of the body in patients with darker skin tones, but the sclera, oral mucous membranes, palms, and soles appear yellow to yellow-orange. Pallor, or paleness of the skin, often results from a decrease in the amount of circulating blood or hemoglobin, causing inadequate oxygenation of the body tissues. Depending on severity, pallor may be visible over the entire skin surface or only in the lips, nail beds, mucous membranes, and conjunctiva. Pallor in patients with dark skin tones is seen as an ashen gray or yellow tinge. Ecchymosis is a collection of blood in the subcutaneous tissues, causing purplish discoloration. Petechiae are small hemorrhagic spots caused by capillary bleeding. If they are present, assess their location, color, and size. diaphoresis --An excessive amount of perspiration, such as when the entire skin is moist, is called diaphoresis. Turgor is the fullness or elasticity of the skin. It is usually assessed on the sternum or under the clavicle by lifting a fold of skin with the thumb and first finger (Fig. 27-8 on page 792). Skin turgor is considered normal when the fold returns to its usual shape when released. When the patient is dehydrated, the skin’s elasticity is decreased, and the skin fold returns slowly. Edema is characterized by swelling, with taut and shiny skin over the edematous area. If the area of edema is palpated with the fingers, an indentation (measured in millimeters for depth of the indentation) may remain after the pressure is released; if the indentation is very deep, it is called pitting edema. Edema may be graded (p. 1680). Edema may be the result of overhydration, heart failure, kidney failure, trauma, or peripheral vascular disease. precordium --the portion of the body over the heart and lower thorax, encompassing the aortic, pulmonic, tricuspid, and apical areas, and Erb’s point. chap 25: Asepsis and Infection Control Host--living being where an infectious, parasitic, or pathogenic agent resides and receives sustenance. Antimicrobials--drugs that treat infections by killing or slowing the growth of microbes causing infection …. bacterial infections are treated with drugs called antibiotics. Infection is a disease state that results from the presence of pathogens (disease producing microorganisms) in or on the body. Bacteria, the most significant and most commonly observed infection-causing agents in health care institutions, can be categorized in various ways. They are categorized by shape: spherical (cocci), rod shaped (bacilli), or corkscrew shaped (spirochetes). Most bacteria require oxygen to live and grow and are, therefore, referred to as aerobic. Those that can live without oxygen are anaerobic bacteria. Virus is the smallest of all microorganisms, visible only with an electron microscope. Viruses cause many infections, including the common cold, hepatitis A, B, and C, and human immunodeficiency virus (HIV). Fungi, plantlike organisms (molds and yeasts) that also can cause infection, are present in the air, soil, and water. Some examples of infections caused by fungi include athlete’s foot, ringworm, and yeast infections. Parasites are organisms that live on or in a host and rely on it for nourishment. An organism’s potential to produce disease in a person depends on a variety of factors, including: Number of organisms Virulence of the organism, or its ability to cause disease Competence of the person’s immune system Length and intimacy (extent) of the contact between the person and the microorganism Endemic (occurs with predictability in one specific region or population) can appear in a different geographic location. Pandemics, like COVID-19, are global outbreaks of a novel (new or not previously identified) virus that did not initially not have a known immunization or treatment. The reservoir for growth and multiplication of microorganisms is the natural habitat of the organism. Possible reservoirs that support organisms pathogenic to humans include other people, animals, soil, food, water, milk, and inanimate objects. Direct contact requires close proximity between the susceptible host and an infected person or a carrier, and includes activities such as touching, kissing, and sexual intercourse. Indirect contact involves personal contact with either: (1) a vector, a living creature that transmits an infectious agent to a human, usually an insect; (2) an inanimate object, called a fomite, such as equipment or countertops. Airborne transmission --Microorganisms can also be spread through the airborne route when an infected host coughs, sneezes, or talks, or when the organism becomes attached to dust particles. Another means of transmission is through droplets. Droplet transmission is similar to airborne transmission. However, airborne particles are smaller than 5 μm (micrometer), and droplet particles are greater than 5 μm. Contact tracing-- involves identifying people with an infectious disease and locating individuals and groups with whom they have come into direct contact to interrupt actual or potential transmission of the infectious disease. Antigen --The foreign material is called an antigen. Antibody --the body commonly responds to the antigen by producing an antibody. Asepsis --The practice of asepsis includes all activities to prevent infection or break the chain of infection. The nurse uses aseptic techniques to halt the spread of microorganisms and minimize the threat of infection. There are two asepsis categories: medical asepsis and surgical asepsis. Medical asepsis, or clean technique, involves procedures and practices that reduce the number and transfer of pathogens. Medical asepsis procedures include performing hand hygiene and wearing gloves. Surgical asepsis, or sterile technique, includes practices used to render and keep objects and areas free from microorganisms. Surgical asepsis procedures include inserting an indwelling urinary catheter or inserting an IV catheter. Health care–associated infections (HAIs)--develops as a result of medical care and may occur in many health care settings including hospitals, rehabilitation facilities, outpatient settings, and dialysis centers. The source of an HAI may be either exogenous or endogenous. An infection is referred to as exogenous when the causative organism is acquired from other people. An endogenous infection occurs when the causative organism comes from microbial life harbored in the person. An infection is referred to as iatrogenic when it results from a treatment or diagnostic procedure. Disinfection destroys all pathogenic organisms except spores; Sterilization destroys all microorganisms, including spores/endospores. Personal protective equipment(PPE) includes gloves, gowns, masks, and protective eye gear. To minimize or prevent exposure to infectious material. Isolation--a protective procedure that limits the spread of infectious diseases among hospitalized patients, hospital personnel, and visitors. Bundles are typically three to five evidence-based practices that, when implemented together, improve patient outcomes. Chap 8 Communication Communication is the process of exchanging information and generating and transmitting meanings between two or more people. It is the foundation of society and the most primary aspect of a nurse–patient interaction. Message is the actual communication product from the source. It might be a speech, interview, conversation, chart, gesture, memorandum, or nursing note. Channel of communication is the medium the sender has selected to send the message. The channel might target any of the receiver’s senses. The message can be sent to the receiver through the following channels: Auditory—spoken words and cues Visual—sight, observations, and perception Kinesthetic—touch feedback --Confirmation of the message provides feedback (i.e., evidence) that the receiver has understood the intended message. Noise—factors that distort the quality of a message—can interfere with communication at any point in the process. Verbal communication is an exchange of information using words, including both the spoken and written word. Verbal communication depends on language, or a prescribed way of using words so that people can share information effectively. Language includes a common definition of words and a method of arranging the words in a certain order. Nonverbal communication--The transmission of information without the use of words is termed nonverbal communication. Nonverbal communication includes facial expressions, eye contact, space, time, boundaries, and body movements. Social media are web-based technologies that allow users to create, share, and participate in dialogue in virtual communities and networks. LEVELS OF COMMUNICATION: 1. Intrapersonal communication, or self-talk, is communication within a person. 2. Interpersonal communication occurs between two or more people with a goal to exchange messages. 3. Group Communication Small-group communication occurs when nurses interact with two or more people. Organizational communication occurs when people and groups within an organization communicate to achieve established goals. Group dynamics involve how individual group members relate to one another during the process of working toward group goals. Therapeutic relationship---a caring, exists among people who provide and receive assistance in meeting human needs. Nurse–patient relationship--When a nurse and patient are involved in a caring, therapeutic relationship, known as the nurse–patient relationship, the nurse is the carer and the patient is the person being cared for, in the context of mutual respect and value. Empathy is an objective understanding of the way in which a patient sees their situation, identifying with the way another person feels, putting yourself in another person’s circumstances, imagining what it would be like to share that person’s feelings and communicating this understanding to the patient. Sympathy is the expression of sorrow for someone’s situation, involving compassion and kindness. Rapport, a feeling of mutual trust experienced by people in a satisfactory relationship, facilitates open communication. Semantics--the study of the meaning of words. Assertive behavior is the ability to stand up for yourself and others using open, honest, and direct communication. Aggressive behavior involves asserting one’s rights in a negative manner that violates the rights of others. Aggression can be verbal or physical. Cliché is a stereotyped, trite, or pat answer. Incivility is rude, disruptive, intimidating, and undesirable verbal and nonverbal communication and behaviors directed at another person. Horizontal violence--Anger and aggressive behavior between nurses, or nurse-to-nurse hostility, has been labeled horizontal violence. This negative behavior is also referred to as bullying, lateral violence, and professional incivility. Bullying occurs when a person is subjected to intimidating behaviors that have a negative effect on them; the conduct is persistent and may involve direct physical or verbal behaviors or indirect behaviors. Chapter 05: Culturally Respectful Care Cultural diversity is the coexistence of different ethnic, sex assigned at birth, racial, and socioeconomic groups within one social unit. These groups include, but are not limited to, people of varying religion, language, physical size, sexual orientation, age, disability, occupational status, and geographic location. Cultural respect enables nurses to deliver services that are respectful of and responsive to the health beliefs, practices, and cultural and linguistic needs of diverse patients. Intersectionality refers to the simultaneous experience of categorical and hierarchical classifications including, but not limited to, race, class, gender, sexuality, and nationality. Culture is a shared system of beliefs, values, and behavioral expectations that provides social structure for daily living. Subculture is a large group of people who are members of the larger cultural group but who have certain ethnic, occupational, or physical characteristics that are not common to the larger culture. Cultural assimilation--When a minority group lives within a dominant group, many members may lose the cultural characteristics that once made them different, and they may take on the values of the dominant culture. This process is called cultural assimilation or acculturation. Culture shock--A person may experience culture shock when placed in a different culture they perceive as strange. Culture shock may result in psychological discomfort or disturbances. Ethnicity is a sense of identification with a collective cultural group, largely based on the group members’ common heritage. Stereotyping--When one assumes that all members of a culture, ethnic group, or race act alike. May be positive or negative. Implicit bias--When we hold attitudes toward people or associate stereotypes with them without our conscious knowledge it is called implicit bias. Cultural imposition is the belief that everyone else should conform to your own belief system。 Cultural blindness occurs when one ignores differences and proceeds as though they do not exist. Culture conflict occurs when people become aware of cultural differences, feel threatened, and respond by ridiculing the beliefs and traditions of others to make themselves feel more secure about their own values. Culturally competent care: • Developing self-awareness • Demonstrating knowledge and understanding of a patient’s culture • Accepting and respecting cultural differences • Resisting judgmental attitudes such as “different is not as good” • Accepting responsibility for one’s own cultural competency Linguistic competence refers to the ability of caregivers and organizations to understand and effectively respond to the linguistic needs of patients and their families in a health care encounter. Personal space is the area around a person regarded as part of the person. This area, individualized to each person and to different cultures and ethnic groups, is the area into which others should not intrude during personal interactions. Among the elements of cultural competence are the following: Developing an awareness of your own existence, sensations, thoughts, and environment to prevent them from having an undue influence on those from other backgrounds. Demonstrating knowledge and understanding of the patient’s culture, health-related needs, and culturally specific meanings of health and illness. Accepting and respecting cultural differences in a manner that facilitates the patient’s and family’s abilities to make decisions to meet their needs and beliefs. Not assuming that the health care provider’s beliefs and values are the same as the patient’s. Resisting judgmental attitudes such as “different is not as good”. Being open to and comfortable with cultural encounters. Accepting responsibility for your own education in cultural competence by attending conferences, reading professional literature, and observing cultural practices. Ethnocentrism-- the belief that the ideas, beliefs, and practices of one’s own culture are superior to those of another’s culture. Cultural humility--the recognition of diversity and power imbalances among individuals, groups or communities, with the action of being open, self-aware, egoless, flexible, exuding respect and supportive interactions, focusing on both self and other to formulate a tailored response. Transcultural nursing-- providing culturally respectful care for patients of all ages, as well as families, groups, and communities. A nurse who is culturally respectful has the knowledge and skills to adapt nursing care to cultural similarities and differences.