21 Blood - Orange Coast College
advertisement

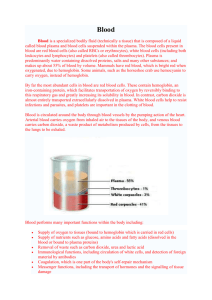
Human Anatomy, First Edition McKinley & O'Loughlin Chapter 21: Blood 1 Blood Considered a connective tissue: contains Cells a liquid ground substance (called plasma) dissolved protein fibers. About four times more viscous (or thicker) than water. Temperature of blood is about 1°C higher than measured body temperature. 21-2 Blood Whole blood can be separated: Liquid component cellular components machine called a centrifuge. blood is withdrawn from a vein and collected in a centrifuge tube tube is placed into the centrifuge, which then spins it in a circular motion for several minutes rotational movement separates the blood into liquid and cellular components 21-3 4 Components of Blood Erythrocytes (or red blood cells) Buffy coat form the lower layer of the centrifuged blood typically make up about 44% of a blood sample makes up the middle layer thin, slightly gray-white layer composed of cells called leukocytes (or white blood cells) and cell fragments called platelets forms less than 1% of a blood sample Plasma straw-colored liquid that rises to the top generally makes up about 55% of blood 21-5 Components of Blood Erythrocytes and the components of the buffy coat are called the formed elements. not “cells,” merely fragments broken off from a larger cell Formed elements and the liquid plasma compose whole blood. 21-6 7 Functions of Blood – Transportation Transports numerous elements and compounds throughout the body. erythrocytes carry oxygen from the lungs to body cells and then transport carbon dioxide from the cells back to the lungs for expulsion from the body blood plasma transports nutrients that have been absorbed from the GI tract hormones secreted by the endocrine organs to their target cells plasma carries waste products from the cells to organs such as the kidneys, where these waste products are removed 21-8 Functions of Blood – Regulation of Body Temp. Regulates body temperature. plasma absorbs and distributes heat throughout the body for cooling the blood vessels in the dermis dilate and dissipate the excess heat through the integument when the body needs to conserve heat, the dermal blood vessels constrict, and the warm blood is shunted to deeper blood vessels in the body 21-9 Functions of Blood – Regulation of pH Levels pH is a measure of how alkaline or acidic a fluid is. Neutral pH is measured at exactly 7. Acidic fluids (e.g., orange juice) are between 0 and 7. Alkaline fluids (e.g., milk) are between 7 and 14. Blood plasma contains compounds and ions that may be distributed to the fluid among tissues (interstitial fluid) to help maintain normal tissue pH. Blood plasma pH is continuously regulated at a value of 7.4 the pH level required for normal cellular functioning. 21-10 Functions of Blood – Maintenance of Fluid Levels Maintains normal fluid levels in the cardiovascular system. Prevents fluid loss. Constant exchange of fluid between the blood plasma and the interstitial fluid. If too much fluid is absorbed in the blood, high blood pressure results. If too much fluid escapes the bloodstream and enters the tissues, blood pressure drops to unhealthy low levels, and the tissues swell with excess fluid. 21-11 Functions of Blood – Maintenance of Fluid Levels To maintain balance of fluid exchange between the blood and the interstitial fluid, blood contains compounds (such as salts and some proteins) to prevent excess fluid loss in the plasma. 21-12 Functions of Blood – Protection Leukocytes (white blood cells) help guard against infection by mounting an immune response if a pathogen or an antigen is found. Plasma transports antibodies, which are molecules that can immobilize antigens until a leukocyte can completely kill or remove the antigen. Platelets and blood proteins protect the body against blood loss by forming blood clots on damaged vessels. 21-13 Components of Plasma Complex mixture of water, proteins, and other solutes. When the proteins are moved from plasma, the remaining fluid is termed serum. Water makes up about 92% of plasma’s total volume. water facilitates the transport of materials in the plasma 21-14 Plasma Proteins The next most abundant materials in plasma are the plasma proteins. Make up about 7% of the plasma. 6 and 8 grams of protein in a volume of 100 milliliters of blood (referred to as g/dl) The plasma proteins include: albumins globulins fibrinogen regulatory proteins 21-15 Plasma Proteins – Albumins Smallest and most abundant of the plasma proteins. make up approximately 58% of total plasma proteins Regulate water movement between the blood and interstitial fluid. Albumins act as transport proteins that carry ions, hormones, and some lipids in the blood. 21-16 Plasma Proteins – Globulins Second largest group of plasma proteins, forming about 37% of all plasma proteins. Smaller alpha-globulins and the larger beta-globulins primarily bind, support, and protect certain waterinsoluble or hydrophobic molecules, hormones, and ions. Gamma-globulins: Also called immunoglobulins or antibodies. Produced by some of our defense cells to protect the body against pathogens that may cause disease. 21-17 Plasma Proteins – Fibrinogen Makes up about 4% of all plasma proteins. Responsible for blood clot formation. Following trauma to the walls of blood vessels, fibrinogen is converted into long, insoluble strands of fibrin, which is the essence of a blood clot. 21-18 Plasma Proteins – Regulatory Proteins Form a very minor class of plasma proteins. <1% of total plasma proteins Include enzymes to accelerate chemical reactions in the blood and hormones being transported throughout the body to target cells. 21-19 Solutes Plasma is an extracellular fluid (ECF). it includes all body fluids that are not found inside cells Plasma is somewhat like interstitial fluid, in that both have similar concentrations of nutrients, waste products, and electrolytes Concentration of dissolved oxygen is higher in plasma than in interstitial fluid, because the cells take up and use the oxygen from the interstitial fluid during energy production. 21-20 Solutes Difference in concentration ensures that oxygen will continue to diffuse from the blood into the tissues. Difference in concentration ensures that carbon dioxide will readily diffuse from the interstitial fluid into the blood, where it will be carried to the lungs and discharged from the body. 21-21 Formed Elements in the Blood Erythrocytes Leukocytes make up more than 99% of formed elements primary function is to transport respiratory gases in the blood make up less than .01% of formed elements contribute to defending the body against pathogens Platelets make up less than 1% of formed elements and help with blood clotting 21-22 Hematocrit Percentage of erythrocytes in the blood. Values vary slightly and are dependent on age and sex. Adult males range between 42% and 56% . Females range from 38% to 46%. Childrens’ hematocrit ranges also vary and differ from adult values. Altitude can affect the hematocrit. body compensates by making more erythrocytes more erythrocytes in the blood can carry more oxygen to the tissues 21-23 24 Erythrocytes Mature erythrocytes lack nuclei. Transport oxygen and carbon dioxide to and from the tissues and the lungs. Lack of nuclei enables them to carry respiratory gases more efficiently. 21-25 26 Hemoglobin in Erythrocytes Every erythrocyte is filled with approximately 280 million molecules of a red-pigmented protein called hemoglobin. Transports oxygen and carbon dioxide, and is responsible for the characteristic bright red color of arterial blood. Hemoglobin that contains no oxygen has a deep red color that is perceived as blue because the blood within these veins is observed through the layers of the skin and the subcutaneous tissue. 21-27 Hemoglobin in Erythrocytes Each hemoglobin molecule consists of four protein building blocks, called globins. All globin chains contain a nonprotein (or heme) group: Alpha (a) chains Beta (b) chains. ring shaped an iron (Fe) ion in its center. Oxygen binds to these iron ions for transport in the blood. Each hemoglobin molecule: four iron ions is capable of binding four molecules of oxygen. 21-28 Hemoglobin in Erythrocytes Oxygen binding is fairly weak Oxygen binds to the hemoglobin ensures rapid attachment and detachment of oxygen with hemoglobin. when the erythrocytes pass through the blood vessels of the lungs. It leaves the hemoglobin when the erythrocytes pass through the blood vessels of body tissues. 21-29 30 Erythrocyte Life Cycle No organelles, therefore can not sustain itself. Finite life span of about 120 days. Daily: Are phagocytized by liver and spleen. About 1% of oldest RBCs are removed By macrophages Some components saved, some discarded 21-31 32 Erythrocyte Life Cycle Some components saved, some discarded Heme group: Converted to biliverdin (green pigment) Then converted to bilirubin In bile, produced by liver Bile enters the digestive tract Helps emulsify fat Bilirubin modified and removed via urine and feces Iron: Transported by transferrin to liver Transferred to ferritin for storage Ferritin can be transported to red bone marrow 21-33 Blood Types Determined by membrane proteins in the RBC cell membrane. Called surface antigens (agglutinogens). Most common group: ABO blood group Two antigens: A and B ABO blood types: Type A: have the A surface antigen Type B: have the B surface antigen Type AB: have both the A and the B surface antigens Type O: have neither the A or the B surface antigen. 21-34 35 Blood Types Antibodies (agglutinins) to the surface antigens are in the plasma ABO group has anti-A antibodies and anti-B antibodies Type Type Type Type A: have anti-B B: have anti-A AB: has neither anti-A or anti-B O: has both anti-A and anti- B 21-36 Antibodies An antibody interacts with a specific antigen. The ABO blood group has both anti-A and anti-B antibodies that react with the surface antigen A and the surface antigen B, respectively. The antibodies in your blood plasma do not recognize the surface antigens on your erythrocytes. 21-37 38 39 Blood Types Rh blood type Based on another surface antigen Called either Rh or D Rh positive (Rh+): has the antigen Rh negative (Rh-): does not have the antigen 21-40 Blood Types Rh blood type Antibody only present with exposure to Rh+ blood (the antigen) Only people with Rh- blood can have the antibody Erthryroblastosis fetalis: Rh+ antibodies in plasma of an Rh- mother can cross the placenta RhoGAM: prevent antibody development 21-41 Leukocytes Leukocytes help initiate an immune response and defend the body against invading pathogens. Leukocytes are true “cells” in that they contain a nucleus and cellular organelles. Leukocytes also differ from erythrocytes in that they are about 1.5 to 3 times larger, and they do not contain hemoglobin. 21-42 21-43 Leukocytes The five types of leukocytes are divided into two distinguishable classes—granulocytes and agranulocytes—based upon the presence or absence of visible organelles termed specific granules. 21-44 Leukocytes – Granulocytes Neutrophil Eosinophils have reddish, or pink-orange granules in their cytoplasm. 60–70% of the total number of leukocytes constitute about 2–4% of the total number of leukocytes nucleus usually has two lobes, which are connected by a thin strand Basophils are 1.5 times larger than erythrocytes least numerous of the granulocytes constitute about 0.5–1% of the total number of leukocytes always exhibit a bilobed nucleus and abundant blue-violet granules in the cytoplasm 21-45 21-46 Leukocytes – Agranulocytes Agranulocytes are leukocytes that have such small granules in their cytoplasm that they are frequently overlooked upon casual observation—hence the name agranulocyte. Agranulocytes include both lymphocytes and monocytes. 21-47 21-48 Leukocytes – Agranulocytes Lymphocytes T-lymphocytes (T-cells) B-lymphocytes (B-cells) manage and direct an immune response some directly attack foreign cells and virusinfected cells stimulated to become plasma cells and produce antibodies Natural killer cells (NK cells) attack abnormal and infected tissue cells 21-49 21-50 Leukocytes – Agranulocytes Monocytes Up to three times the diameter of an erythrocyte. Constitute about 3–8% of all leukocytes. Nucleus is kidney-shaped or U-shaped. Macrophages phagocytize bacteria, cell fragments, dead cells, and debris. 21-51 Platelets Irregular, membrane-enclosed cellular fragments about 2 micrometers in diameter (less than onefourth the size of an erythrocyte). In stained preparations, they exhibit a dark central region. Sometimes called thrombocytes. Continually produced in the red bone marrow by cells called megakaryocytes. 21-52 21-53 Platelets Severe trauma to a blood vessel causes the blood to coagulate, or clot. Components in the plasma produce a web of fibrin that traps erythrocytes and platelets in the web to halt blood flow. 21-54 Hemopoiesis Also called hematopoiesis Production of the formed elements of blood Occurs in red bone marrow 21-55 Hemopoiesis Begins with hemopoietc stem cells Called Hemocytoblast Pluripotent cells Produce two cell lines Myloid line Everything but lymphocytes Lymphoid line lymphocytes 21-56 21-57 Hemopoiesis Influenced by a number of hormones and growth factors Colony-stimulating factors: Multi-CSF: RBCs,granulocytes,monocytes, platelets GM-CSF: granulocytes, monocytes From myloid stem cell From progenitor cell G-CSF: granulocytes From myeloblast cells 21-58 Hemopoiesis Colony-stimulating factors: contined M-CSF: monocytes From monoblasts Thrombopoietin: megakaryocytes and platelets Erythropoietin: hormone from the kidney, RBC’s 21-59 Hemopoiesis Erythropoiesis: from progenitor cell Reticulocyte: loses all organelles Thrombopoiesis Leukopoiesis Granulocyte maturation: from myeloblast Monocyte maturation: from monoblast Lymphocyte maturation: from lymphoid stem cell B-lymphoblast T-lymphoblast 21-60 21-61