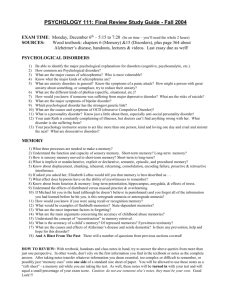
Psychological Disorders

Historical Roots
In the ancient world, psychopathology was thought to be caused by demons and spirits that had taken possession of the person’s mind and body.
Part of daily life in ancient worlds was spent doing rituals aimed at outwitting or placating these supernatural beings.
Hippocrates
In 400 B.C. the Greek physician Hippocrates took the first step toward a scientific view of mental illness when he said that abnormal behavior had physical causes.
He taught his disciples to interpret the symptoms of psychopathology as an imbalance among our body fluids called “humors.”
Humors
Blood
Choler (yellow bile)
Melancholer (black bile)
Phlegm
Origins
Heart
Liver
Spleen
Brain
Temperament
Sanguine (cheerful)
Choleric (angry)
Melancholy (depressed)
Phlegmatic (sluggish)
Early Theories
Music or singing was often used to chase away spirits.
In some cases
trephening was used:
Cutting a hole in the head of the afflicted to let out the evil spirit.
Salem Witch Trials
As a result of erroneous thinking, thousands of mentally disturbed people were executed.
In Salem Massachusetts, was one example of the problems with this type of thinking.
A modern analysis of the Salem witch trials has concluded that the girls were probably suffering from poisoning by a fungus growing on rye grain-the same fungus that produces the hallucinogenic drug LSD.
Psychopathology
What was formerly known as mental illness or mental disorder is now often referred to as psychopathology.
Some feel “mental illness” puts the basis for the illness on biology, even though psychologists have shown that environment is often the cause of the disorder.
Psychopathology is any pattern of emotions, behavior, or thoughts inappropriate to the situation and leading to personal distress or the inability to achieve important goals.
Stereotypes & Stigma
Psychological disorders are incurable
People with psychological disorders are dangerous
People with psychological disorders behave bizarrely & are very different from “normal” people
What effect do these have on the likelihood of someone truly suffering seeking help?
Psychological Disorders/Abnormal Psych
Psychological Disorders
At various moments, all of us feel, think or act the way disturbed people do much of the time. We, too, get anxious, depressed, withdrawn, suspicious, or deluded, just less intensely and more briefly.
Some 450 million people world wide suffer psychological disorders.
No culture known to man is without some form of psychological disorders.
Prevalence of Psychopathology
In America, mental illness is far more common than most people realize.
Over 15% of the population currently suffers from diagnosable mental health problems.
Another study found that during any given year, the behaviors of over 56 million Americans meet the criteria for a diagnosable psychological disorder (Carson et al.
1996).
Over the lifespan, as many as 32% of Americans suffer from some psychological disorder (Regier et al., 1988).
What is Psychological Disorder?
How do we discern what is normal and abnormal?
What about a soldier who risks his life in war? A grief stricken mother who cannot return to her normal routines three months after losing her son?
Psychological disorders are persistently harmful thoughts, feelings and actions.
When behavior is deviant, distressful and dysfunctional, psychologists label it a disorder.
3 Classical Symptoms of
Severe Mental Illness
The more extreme a disorder is, the more easily it is detected. When trying to diagnose a patient, doctors look for three classic symptoms of sever psychopathology:
Hallucinations-false sensory experiences.
Delusions-extreme disorders that involve persistent false beliefs.
Affect (emotion)-characteristically depressed, anxious, manic, or no emotional response.
Psychological Disorders as a Continuum
No Disorder Mild Disorder
Moderate
Disorder
Severe
Disorder
Absence of signs of psychological disorder
Few signs of distress or other indicators of psychological disorder
Indicators of disorders are more pronounced and occur more frequently
Clear signs of psychological disorder, which dominate the person’s life
Absence of behavioral problems
Few behavior problems; responses usually appropriate to the situation
More distinct behavior is often inappropriate to the situation
Severe and frequent behavior problems; behavior is usually inappropriate to the situation
No problems with interpersonal relationships
Few difficulties with relationships
More frequent difficulties with relationships
Many poor relationships or lack of relationships
Disorders are exaggerations of normal behavior and responses.
The Medical Model
In the late 18 th century, the “disease view” reemerged.
The result was the medical model, a view that mental disorders are diseases of the mind that, like ordinary physical diseases, have objective causes and require specific treatment.
**
Problems with the Medical Model
Despite its success, modern psychologists find fault with relying solely on the medical model.
They suggest that treating the disorder as a
“disease” leads to a doctor-knows-best approach in which the therapist takes all the responsibility for diagnosing and correcting the problem.
In this model, the patient becomes a passive recipient of medication and advice.
Perspectives and
Disorders
Psychological School/Perspective
Psychoanalytic/Psychodynamic
Humanistic
Cause of the Disorder
Internal, unconscious drives
Failure to strive to one’s potential or being out of touch with one’s feelings.
Behavioral
Cognitive
Sociocultural
Biomedical/Neuroscience
Reinforcement history, the environment.
Irrational, dysfunctional thoughts or ways of thinking.
Dysfunctional Society
Organic problems, biochemical imbalances, genetic predispositions.
Social-Cognitive-Behavioral Approach
As psychology has evolved, theories which were originally at odds, have now been combined to offer more thorough explanations, for example, cognitive psychology and behaviorism.
Cognitive psychology looks inward, emphasizing mental processes. Behaviorism looks outward and emphasizes the influences of the environment.
Psychologist from these perspectives see these two as complementary, and add that cognitions and behavior usually happen in social context, requiring social
perspective.
Combining Perspectives
The behavioral perspective tells us that abnormal behaviors can be acquired in the same fashion as healthy behaviors-- through behavioral learning.
The cognitive perspective suggests that we must consider how people think about themselves and their relations with other people.
Social-cognitive-behavioral approach, then, is an alternative to the medical model combining all three of psychology’s major perspectives.
The Bio-psycho-social Model of
Mental Disorder
Modern bio-psychology assumes that some mental disturbances involve the brain or nervous system in some way.
Subtle changes in the brain’s tissue or its chemical messengers- the neurotransmitters- can profoundly alter thoughts and behaviors.
Genetic factors, brain injury, infection, and learning are some of the factors that can tip the balance towards psychopathology.
Sociocultural
(Roles, expectations, definition of normality and disorder)
Biological
(Evolution, individual genes, brain structures and chemistry)
Psychological
(Stress, trauma, learned helplessness, mood-related perceptions and memories)
In short, biological, socio-cultural and psychological factors contribute to psychological disorders
A Short History of the DSM
The DSM-1 (1952), 106 disorders across several major categories, reflecting a psychodynamic perspective on etiology
DSM II (1968), 182 disorders, similar framework as DSM-1; like
DSM-1, it lacked specification of specific symptoms of many disorders; distinguished among disorders at broader levels of neurosis, psychosis, and personality disturbance
DSM-III (1980) and DSM-III-R (1987), which focused on standardization of diagnostic categories by linking them to specific criteria or symptom clusters, expressed in colloquial language; included 265 diagnoses in DSM-III and 292 in DSM-III-R, which changed some of the diagnostic criteria
DSM-IV (1994) and DSM-IV-TR (2000), 297 disorders, relatively minor changes
Major Changes
Change
Elimination of multi-axial system a
Comment
Clinicians wanted simplified, diagnosisbased system; distinctions between Axis I and Axis II disorders were never clearly justified; clinicians can still specify external stressors; new assessment measures will be introduced
Establishes 20 diagnostic classes or categories of mental disorders
Categories based on groupings of disorders sharing similar characteristics; some categories represent spectrums of related disorders
Introduction of new diagnostic category of
Neurodevelopmental Disorders to include
Autism Spectrum Disorder and ADHD and other disorders reflecting abnormal brain development
Increasing emphases on neurobiological bases of mental disorders and the developing understanding that abnormal brain development underlies many types of disorders
Major Changes
Change
Introduces more dimensionality (severity ratings) but does not restructure personality disorders as some had proposed
Comment
Major changes in personality disorders held over until next revision, the DSM 5.1 (or maybe 5.2)
Roman numerals dropped: DSM-5, not
DSM-V
Removes obsessive-compulsive disorder from category of Anxiety Disorders and places it in new category of Obsessive-
Compulsive and Related Disorders
Allows for easier nomenclature for midcourse revisions, 5.1, 5.2, etc.
Recognizes a spectrum of obsessivecompulsive type disorders, including body dysmorphic disorder; however, anxiety remains the core feature of OCD, so questions remain about separating it from anxiety disorders
Major Changes
Change
Provides a means of rating severity of symptoms, such as for ASD
Comment
Encourages clinicians to recognize the dimensionality of disorders
Greater emphasis on comorbidity; e.g., use of anxiety ratings in diagnosing depressive and bipolar disorders
Provides more explicit recognition of comorbidity in having clinicians rate level of anxiety in mood disorders
Change
Major Changes
Comment
Elimination of term “somatoform disorders” (now Somatic Symptom and
Related Disorders)
Eliminates a term few people understood
(somatoform disorders) and now emphasizes the psychological reactions to physical symptoms, not whether they are medically based
Reorganization of mood disorders into two separate diagnostic categories of
Depressive Disorders and Bipolar and
Related Disorders
No major changes anticipated, but no clear basis for eliminating umbrella construct of mood disorders
Change
Major Changes
Comment
Hypochondriasis dropped as distinct disorder Eliminates the pejorative term
“hypochondriasis”; people formerly diagnosed with hypochondriasis may now be diagnosed with Somatic Symptom Disorder if their physical symptoms are significant or with Illness Anxiety Disorder if their symptoms are minor or mild
Factitious Disorder moved to Somatic
Symptom and Related Disorders
Associated with other somatic symptom disorders, but is distinguished by intentional fabrication of symptoms for no apparent gain other than assuming medical patient role
Diagnostic Categories
Diagnostic Category Examples of Specific Disorders
Neurodevelopmental Disorders Autism Spectrum Disorder
Specific Learning Disorder
Communication Disorders
ADHD, Motor Disorders, etc.
Schizophrenia Spectrum and Other
Psychotic Disorders
Bipolar and Related Disorders
Depressive Disorders
Schizophrenia
Schizophreniform Disorder
Schizoaffective Disorder
Delusional Disorder
Schizotypal Personality Disorder
Bipolar I Disorder, Bipolar II Disorder
Cyclothymic Disorder
Disruptive Mood Dysregulation Disorder
Major Depressive Disorder
Persistent Depressive Disorder
Premenstrual Dysphoric Disorder
Diagnostic Categories
Diagnostic Category Examples of Specific Disorders
Anxiety Disorders
Obsessive-Compulsive and Related
Disorders
Trauma and Stressor Related Disorders
Specific Phobia
Social Anxiety Disorder (Social Phobia)
Panic Disorder
Agoraphobia
Generalized Anxiety Disorder
Separation Anxiety Disorder
Selective Mutism
Obsessive-Compulsive Disorder
Body Dysmorphic Disorder
Hoarding Disorder
Hair-Pulling Disorder (Trichotillomania)
Excoriation (Skin-Picking) Disorder
Adjustment Disorders
Acute Stress Disorder
Posttraumatic Stress Disorder
Reactive Attachment Disorder
Disinhibited Social Engagement Disorder
Diagnostic Categories
Diagnostic Category
Dissociative Disorders
Somatic Symptom and Related
Disorders
Feeding and Eating Disorders
Elimination Disorders
Examples of Specific Disorders
Dissociative Identity Disorder
Dissociative Amnesia
Depersonalization/Derealization Disorder
Somatic Symptom Disorder
Illness Anxiety Disorder
Conversion Disorder (Functional Neurological
Symptom Disorder)
Factitious Disorder
Anorexia Nervosa
Bulimia Nervosa
Binge Eating Disorder
Pica, Rumination Disorder
Avoidant/Restrictive Food Intake Disorder
Enuresis
Encopresis
Sexual Dysfunctions
Diagnostic Categories
Diagnostic Category
Sleep-Wake Disorders
Examples of Specific Disorders
Insomnia Disorder
Hypersomnolence Disorder
Narcolepsy
Breathing-Related Sleep Disorders
Circadian Rhythm Sleep-Wake Disorders
Parasomnias: Sleepwalking, Sleep Terrors,
Nightmare Disorder, Rapid Eye Movement Sleep
Behavior Disorder
Restless Legs Syndrome
Delayed Ejaculation
Erectile Disorder
Female Orgasmic Disorder
Female Sexual Interest/Arousal Disorder
Genito-Pelvic Pain/Penetration Disorder
Male Hypoactive Sexual Desire Disorder
Premature (Early) Ejaculation
Diagnostic Categories
Diagnostic Category
Gender Dysphoria
Disruptive, Impulse-Control, and
Conduct Disorders
Substance-Related and Addictive
Disorders
Neurocognitive Disorders
Examples of Specific Disorder
Gender Dysphoria
Oppositional Defiant Disorder
Intermittent Explosive Disorder
Conduct Disorder
Antisocial Personality Disorder
Pyromania
Kleptomania
Substance Use Disorders
Substance-Induced Disorders
Gambling Disorder
Delirium
Major & Mild Neurocognitive Disorders
Diagnostic Categories
Diagnostic Category
Personality Disorders
Examples of Specific Disorders
Paranoid Personality Disorder
Schizoid Personality Disorder
Schizotypal Personality Disorder
Antisocial Personality Disorder
Borderline Personality Disorder
Histrionic Personality Disorder
Narcissistic Personality Disorder
Avoidant Personality Disorder
Dependent Personality Disorder
Obsessive-Compulsive Personality Disorder
Indicators of Abnormality
While psychologists look for the three classical symptoms, not all disorders have such sever symptoms.
A few others are:
Distress: Does the individual show unusual or prolonged levels of anxiety?
Maladaptiveness: Does the person act in ways that make others fearful?
Irrationality: Does the person act or talk in ways that are irrational or incomprehensible to others?
Unpredictability: Does the individual behave erratically and inconsistently at different times?
Unconventional/undesirable behavior: Does the person act in ways that are statistically rare and violate social norms?
Anxiety Disorders are psychological disorders characterized by distressing, persistent anxiety or maladaptive behaviors that reduce anxiety
We all experience anxiety at one point and time in our lives, however it is not intense and not persistent
Anxiety disorders are the most common mental
illness in the U.S., affecting 40 million adults in the United States age 18 and older (18% of U.S. population).
Symptoms:
Often jittery
Agitated
Sleep deprived
Difficulty concentrating
Depressed Mood
Apprehension may leak out through
Furrowed brows
Twitching eyelids
Trembling
Perspiration
Fidgeting
Generalized Anxiety Disorder
An anxiety disorder in which a person is continually tense, apprehensive, and in a state of autonomic nervous system arousal
GAD affects 6.8 million adults, or 3.1% of the
U.S. population.
Women are twice as likely to be affected as men.
Anxiety Disorders :
Generalized Anxiety Disorder:
High level of “free-floating” anxiety not tied to specific threat; pervasive & persistent stimulation of ANS
• Must last at least 6 months for diagnosis
Brood over relatively minor issues
However, as time passes emotions tend to mellow and by age 50, generalized anxiety disorder becomes rare
More common in females
Psychological Disorders/Abnormal Psych
Anxiety Disorders
Specific phobias focus on one thing
People tend to avoid that situation or particular thing
Social Phobias is basically shyness taken to the extreme
Intense fear of being scrutinized by others, avoid potentially embarrassing social situations, or will sweat, tremble, or have diarrhea when doing so
15 million, 6.8%
Equally common among men and women, typically beginning around age 13.
Agoraphobia
Fear or avoidance of situations in which escape might be difficult or help unavailable when panic strikes
Phobias
Anxiety disorder marked by a persistent, irrational fear and avoidance of a specific object or situation
19 million, 8.7%
Women are twice as likely to be affected as men.
Typically begins in childhood; the median age of onset is 7.
Anxiety Disorders
Phobic Disorder:
Anxiety now has a specific focus: persistent, irrational fear of something presenting no real danger
Beyond simple phobias – maladaptive, disruptive to everyday life (e.g., various social phobias, often w/ physical symptoms
Remember conditioning!
Psychological Disorders/Abnormal Psych
Causes of Phobias
Genetics
– Martin Seligman used photos of flowers and snakes to test this theory
Specific events
– Specific events can trigger a phobia
Phobias are likely linked to the amygdala, the part of the brain that controls aggression and fear
Anxiety Disorders
Common and uncommon fears
Panic Disorder
An anxiety disorder marked by unpredictable minutes-long episodes of intense dread in which a person experiences terror and accompanying chest pain, chocking, or other frightening sensations
6 million, 2.7%
Women are twice as likely to be affected as men.
Very high comorbidity rate with major depression.
Recurring attacks of overwhelming anxiety, sudden & relatively brief
May be mistaken for heart attack
Often linked to agoraphobia; may “fear the fear itself”
Onset late adolescence, early adulthood; may be rooted in limbic system
Psychological Disorders/Abnormal Psych
Understanding Anxiety Disorders
Learning perspective
Fear conditioning: researchers have demonstrated ability to condition fear in rats
Two specific learning processes contribute to anxiety
Stimulus generalization
Reinforcement
Observational Learning
Biological Perspective
Natural Selection: fear threats face by ancestors
Genetics: researchers are examining neurotransmitters that influence an anxiety gene
The Brain: Anxiety disorders are manifested biologically as an overarousal of brain areas involved in impulse control and habitual behaviors
Obsessive-Compulsive Disorder
An anxiety disorder characterized by unwanted repetitive thoughts (obsessions) and/or actions
(compulsions)
Crosses the line from normality to disorder when they persistently interfere with everyday living and cause the person distress
2-3% cross the line during their teens or early twenties
Obsessive thoughts and compulsive behavior become so ritualistic that effective functioning become impossible
Anxiety Disorders
Acute Stress Disorder
The person experienced or witnessed trauma
with an event where there was the threat of or actual death or serious injury.
The event may also have involved a threat to the person's or another person's physical well-being.
The person responded to the event with
strong feelings of fear, helplessness, or horror.
Acute Stress Disorder
The person experiences at least three of the following dissociative symptoms during or after the traumatic event:
Feeling numb or detached or having difficulties experiencing emotions.
Feeling dazed or not entirely being aware of surroundings.
Derealization , or feeling as though people, places, and things are not real.
Depersonalization , or feeling separated and detached from oneself.
Dissociative amnesia, or being unable to recall important parts of the traumatic event.
Acute Stress Disorder
Studies of motor vehicle accident (MVA) survivors have found rates of ASD ranging from approximately 13% to 21%
A study of survivors of a typhoon revealed an ASD rate of 7%
While a study of survivors of an industrial accident revealed a rate of 6%
A rate of 19% was found in survivors of violent assault
While a rate of 13% was found in a mixed group consisting of survivors of assaults, burns, and industrial accidents.
A study of victims of robbery and assault found that 25% met criteria for ASD.
While a study of victims of a mass shooting found that 33% met criteria.
Acute Stress Disorder
ASD and PTSD differ in two fundamental ways:
The first difference is that the diagnosis of ASD can be given only within the first month following a traumatic event. If posttraumatic symptoms were to persist beyond a month, the clinician would assess for the presence of PTSD.
The ASD diagnosis would no longer apply.
ASD also differs from PTSD in that it includes a greater emphasis on dissociative symptoms.
Trauma & Stressor Disorder
Post-Traumatic Stress Disorder (PTSD):
Delayed (“post”) stress (“stress”) reaction to uncontrollable danger (“traumatic”)
Haunting memories that constantly intrude on thoughts; nightmares; social withdrawal; depression
Symptoms may last years
Often seen in war veterans, victims of violent crime, etc.
Psychological Disorders/Abnormal Psych
Post-Traumatic Stress Disorder (PTSD
7.7 million, 3.5%
Women are more likely to be affected than men.
Rape is the most likely trigger of PTSD: 65% of men and 45.9% of women who are raped will develop the disorder.
Childhood sexual abuse is a strong predictor of lifetime likelihood for developing PTSD.
Post-Traumatic Stress Disorder
PTSD
Cause: experiencing / witnessing a traumatic event
(fear, helplessness, horror)
Nightmares, flashbacks, social withdrawal, insomnia
Combat veterans, disaster or accident survivors, sexual assault victims, 2/3 of prostitutes
Basic trust erodes, sense of hopelessness
15% of Vietnam vets (45% for heavy combat)
1 in 6 Iraqi combat infantry veterans
Shell Shock
Precursor to PTSD?
Trauma & Stressor Disorder
Etiology of Anxiety Disorders:
Biological
• Concordance rates show some genetic basis
• Hypersensitivity to internal signs of anxiety
• GABA synapses affected by anti-anxiety meds (Valium,
Xanax, Prozac) that suppress the CNS
Conditioning/Learning
• Phobias & preparedness
• Observational learning
Cognitive factors: misinterpretation, inappropriate focus etc.
Stress-related factors: duh
Psychological Disorders/Abnormal Psych
Reactive Attachment Disorder
Reactive attachment disorder is a rare but serious condition in which an infant or young child doesn't establish healthy attachments with parents or caregivers.
Reactive attachment disorder may develop if the child's basic needs for comfort, affection and nurturing aren't met and loving, caring, stable attachments with others are not established.
Withdrawal, fear, sadness or irritability that is not readily explained
Sad and listless appearance
Not seeking comfort or showing no response when comfort is given
Failure to smile
Watching others closely but not engaging in social interaction
Failing to ask for support or assistance
Failure to reach out when picked up
No interest in playing peekaboo or other interactive games
Major Depression
Major depression is a form of depression that does not alternate with mania
(happiness).
It is normal to become depressed after a sad or unfortunate event but if a person remains depressed weeks or months after that event, it may be classified as major depression.
Major depression does not give way to manic episodes.
Major Depression
By many accounts, depression is under diagnosed and under treated.
Lifetime Risk of a
Depressive Episode lasting a Year or More
Globally speaking, studies indicate that depression is the single most prevalent disability.
While some differences may be a result of reporting, other factors seem to be at work too:
Taiwan/Korea = low divorce rate
Lebanon = war in Middle East
Taiwan
Korea
Puerto Rico
U.S.
Germany
Canada
New Zealand
France
Lebanon
1.5%
2.9%
4.3%
5.2%
9.2%
9.6%
11.6%
16.4%
19%
Depression
Mood Disorders-
Depression
Canadian depression rates
Causes of Depression
Some causes of major depression involve genetic predisposition. Severe bouts of depression often run in families-this indicates a biological basis.
Further indication of a biological basis for depression are that drugs that affect the brains levels of certain neurotransmitters can be very effective.
However, biology alone cannot account for everything.
Cognitive Explanations
Probably because of low self-esteem, depressionprone people are more likely to perpetuate the depression cycle by attributing negative events to their own personal flaws or external conditions they feel helpless to change.
Martin Seligman calls this learned helplessness.
Locus of control-internal vs. external
Cognitive-Behavioral Cycle of Depression
Fred decides to be more sociable, but when he asks Teresa for a date she already has plans.
Fred concludes that he is not very interesting or attractive and that people don’t like him.
Negative
Event
Low Self-Esteem and Negative
Interpretations
Because of Fred’s negative behaviors, people avoid himreinforcing his symptoms.
Social Rejection and Loneliness
Depression
Fred feels completely alone and unhappy
Negative
Behaviors
Fred avoids people, skips school and neglects personal hygiene
The Cognitive Approach
The cognitive approach to depression points out that negative thinking styles are learned and modifiable.
*Think classical and operant conditioning.
Beck’s Basics
Aaron Beck suggests that depression is a result of negative thinking which he called ‘cognitive errors’ (errors in logic)
Beck identified three negative thoughts that seemed to be really automatic and occurred without delay in depressed patients.
The “Cognitive Triad:”
Self
External World
Future
Beck believes that faulty thinking leads to depression. The question remains though, which came first, the depression or the faulty thoughts.
Increasing Rates of Depression
Rates of depression have increased 10-20 times what they were 50 years ago.
The average age of people experiencing depression has gone down.
Martin Seligman identifies 3 causes of this trend:
1.
Out-of-control individualism/self-centeredness-focuses on individual successes and failures rather than group accomplishments.
Increasing Rates of Depression
2.
The self-esteem movement- teaching a generation of children they should feel good about themselves, irrespective of their efforts and achievements.
3.
A culture of victimology- reflexively pointing the finger of blame at someone or something else.
Types of Dissociative
Disorders
Four Major Types:
– Dissociative amnesia
– Dissociative identity disorder
– Dissociative fugue
– Depersonalization Disorder
Types of Dissociative Disorders
Psychogenic Amnesia : Amnesia with no physiological basis
biologically induced amnesia = organic amnesia )
Fugue = Psychogenic Amnesia + unfamiliar environment (fugue = flight / loss of identity and flee)
Signs and Symptoms
Memory loss (amnesia) of certain time periods, events and people
Mental health problems, including depression and anxiety
A sense of being detached from yourself
(depersonalization)
A perception of the people and things around you as distorted and unreal
(derealization)
A blurred sense of identity
Causes
Abuse
– Physical
– Sexual
– Emotional
Frightening home life
It is rare for adults to develop a dissociative disorder
Types of Dissociative Disorders
Dissociative Identity Disorder (DID)
AKA Multiple Personality Disorder
Usually from traumatic event / overwhelming stress (high % report child abuse) often at young age (3-5 years)
Self-protection / coping mechanism
Distinctive identities for different events
(toddler to adult)
Norm- 3-6 identities (2 to qualify)
Almost entirely confined to N. America
Very controversial as medical diagnosis
Dissociative Disorders
Depersonalization Disorder:
• Feeling that you aren’t “real”
• Sense of detachment from your own body, feeling as if you’re losing grip on reality, living in a dream
• Only a disorder if recurring
(est. 70% experience at some point)
Psychological Disorders/Abnormal Psych
Somatoform Disorders
“soma” = body
Psychological problem manifested in a physiological symptom (IOW: physical problem without a physical cause)
Common among those claiming disability
Two major disorders :
hypochondriasis : imagined or exaggerated illnesses (no medical cause)
Conversion disorder : involves motor or sensory problems with no biological explanation / cause
Conversion blindness, conversion paralysis
Explaining Somatoform
Psychoanalytic
Outward manifestations of unconscious conflict
Behaviorists
Reinforcement for behavior (can’t work or sympathy / attention)
Clinical Distinction…
Somatoform patient: unconscious of psychological causes (does not seek to maintain role of patient)
Factitious patient: Consciously creating the symptoms, …prolonging role of patient
Somatoform Disorders
Body Dysmorphic Disorder:
• Characterized by excessive concern with bodily appearance
• Concern their nose is too big, hair too thin, over/underweight to the point of maladaptive behavior & personal distress
• Some become “plastic surgery addicts”
Psychological Disorders/Abnormal Psych
Somatoform Disorders
Etiology of Somatoform Disorders:
• Personality o Histrionic personality – attention?
o Neuroticism
• Cognitive factors o Misinterpret minor issues o Faulty stds of “good health”
• “Sick Role” o Like a defense mechanism – don’t have to deal w/ other problems
Psychological Disorders/Abnormal Psych
Bipolar & Related
Manic Episode
a mood disorder marked by a hyperactive, wildly optimistic state
Bipolar Disorder
a mood disorder in which the person alternates between the hopelessness and lethargy of depression and the overexcited state of mania
formerly called manic-depressive disorder
Schizophrenia
Disordered / distorted thinking
Breakdown in selective attention (Can’t filter out information)
►
Disturbed perceptions
Delusions: beliefs that have no basis in reality
►
Delusions of persecution = paranoia
►
Delusions of grandeur = greatness
Hallucinations: Perceptions in the absence of sensory stimulation
►
Inappropriate actions / emotions
Things to consider…
►
Most severe of psych disorders
►
Usually starts in late teens / early twenties
►
1 out of every 100 people have
Schizophrenia
Types of Schizophrenia
Disorganized Schizophrenia
Paranoid Schizophrenia
Catatonic Schizophrenia
Undifferentiated Schizophrenia
Acute vs. Chronic Schizophrenia
What’s the difference?
Acute: Abrupt display of symptoms- can be short duration and never return or become longterm issue
Chronic: Long-term struggle with Schizophrenia
Disorganized Schizophrenia
►
Odd use of language (Word Salad = fragmented speech
Neologisms: made up words
Clang associations: string together nonsense words that rhyme
►
Inappropriate effect:
Laugh in sorrowful setting
Flat effect: no emotional response at all
Paranoid Schizophrenia
►
Delusions of persecution
►
“out to get me”
Catatonic Schizophrenia
►
Engage in odd movements
►
Remain motionless for hours (odd positions
/ poses / Waxy flexibility
► parrot-like repeating of speech, movement
Undifferentiated Schizophrenia
►
Disordered thinking, but no symptoms of other types of Schizophrenia
Explaining Schizophrenia
►
Biological
Dopamine hypothesis
►
Excessive levels = Schizophrenia (average 6x normal levels)
Enlarged brain ventricles
Genetic predispositions
Abnormality of 5 th chromosome
►
Social-Cognitive
Double binds: contradictory messages = distorted ways of thinking
Schizophrenic DisordeRs
Is a change in order for the DSM-V?:
Eliminate subcategories in favor of:
Positive: behavioral excesses (hallucinations, delusions, bizarre behavior)
Negative: behavioral deficits (poverty of speech, withdrawal, flat affect, apathy)
Psychological Disorders/Abnormal Psych
Schizophrenic DisordeRs
Etiology of Schizophrenic Disorders:
Typically emerges in late adolescence; more significant in males
Biological factors:
• Genetics
• Excess dopamine
• Structural abnormalities in brain
• Problems during prenatal neural development (viral infections?)
• Stress may be an important trigger
Psychological Disorders/Abnormal Psych
Schizophrenic DisordeRs
Psychological Disorders/Abnormal Psych
Schizophrenia
Personality Disorders
Enduring, maladaptive behavior that negatively affects one’s ability to function.
Usually less serious than other disorders.
Nurture based
Personality Disorder
Antisocial disorder ( most serious )
No regard for others’ feelings / world as hostile / look out for oneself / absence of conscience
No fear, no shame
serial criminals, serial killers (worst case)
Electric shock: no increased anxiety in anticipation
Causes: Both Biological and Psychological
• Nurture influential: hero or villain …
More Personality Disorders
Borderline Personality
Disorder of emotions (intense instability) self-mutilation
Severe anxiety, depression
Dependant personality disorder
Overly dependant on attention, help from others
Paranoid Personality Disorder
Feel persecuted, very distrustful
Narcissistic Disorder
Self-love, grandiose self-importance, entitlement, failed relationships, “”narcissistic paradox”
Histrionic Disorder : (center of attention)
Overly dramatic behavior
Obsessive-Compulsive Disorder
Overly concerned with thoughts and behaviors