Musculoskeletal Tissue
advertisement

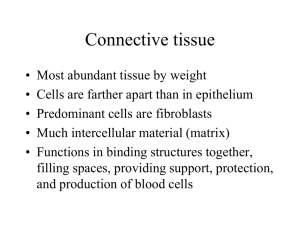
Chapter 1 Musculoskeletal Tissue Tissues of the body Epithelial Nervous Connective Muscle Epithelial tissue Two forms – Membranous Forms such structures as the outer layer of the skin, the inner lining of the body cavities and lumina, and the covering of visceral organs – Glandular Specialized tissue that forms the secretory portion of glands Nervous tissue Helps coordinate movements via a complex motor control system of prestructured motor programs and a distributed network of reflex pathways mediated throughout the CNS Connective tissue Found throughout the body Divided into subtypes according to the matrix that binds the cells Includes bone, cartilage, tendons, ligaments, and blood tissue Muscle tissue Responsible for the movement of materials through the body, the movement of one part of the body with respect to another, and locomotion Three types: – Smooth – Cardiac – Skeletal Connective Tissue The primary types of connective tissue cells are: – Macrophages, which function as phagocytes to clean up debris – Mast cells, which release chemicals associated with inflammation – Fibroblasts, which are the principal cells of connective tissue Connective Tissue Proper 1. 2. 3. 4. 5. 6. Loose connective tissue Dense regular connective tissue Dense irregular connective tissue Elastic connective tissue Reticular connective tissue Adipose connective tissue Cartilage and bone tissue 1. 2. 3. Hyaline cartilage Fibrocartilage Elastic cartilage Collagen and Elastin Collagen and elastin are vital constituents of the musculoskeletal system Collagen – Maintains the structural integrity of various tissues – Provides tensile strength to tissues Elastin – Provides the tissues in which it is situated with elastic properties Collagen and Elastin Collagenous and elastic fibers are sparse and irregularly arranged in loose connective tissue, but are tightly packed in dense connective tissue – Fascia is an example of loose connective tissue – Tendons and ligaments are examples of dense regular connective tissue Tendons Cordlike structures that function to attach muscle to bone and to transmit the forces generated by muscles to bone in order to achieve movement or stability of the body in space Tendons The fascicles of tendons are held together by loose connective tissue called endotenon – Endotenon contains blood vessels, lymphatics and nerves, and permits longitudinal movements of individual fascicles when tensile forces are applied to the structure The connective tissue surrounding groups of fascicles and/or the entire structure is called the epitenon Myotendinous junction (MTJ). The site where the muscle and tendon meet Very vulnerable to tensile failure, especially biceps and triceps brachii, the rotator cuff muscles, the flexor pollicis longus, the peroneus longus, the medial head of the gastrocnemius, the rectus femoris, the adductor longus, the iliopsoas, the pectoralis major, the semimembranosus, and the whole hamstrings group Skeletal ligaments Skeletal ligaments are fibrous bands of dense connective tissue that connect bones across joints – Contribute to the stability of joint function by preventing excessive motion – Act as guides to direct motion – Provide proprioceptive information for joint function Ligament pathology Ligament injuries are graded according to severity – First-degree (mild) – Second-degree (moderate) – Third degree (complete) Ligament pathology First-degree sprain – Minimal loss of structural integrity – Little or no swelling – Minimal bruising – Minimal functional loss – Early return to training Ligament pathology Second-degree sprain – Significant structural weakening – Some abnormal motion – More bruising and swelling – Tendency for recurrence – Need protection from risk of further injury – May need modified immobilization Ligament pathology Third-degree sprain – Loss of structural integrity – Marked abnormal motion – Significant bruising – Needs prolonged protection – Surgery may be considered – Permanent functional instability a possibility Bone A highly-vascular form of connective tissue Composed of collagen, calcium phosphate, water, amorphous proteins, and cells The collagen of bone is produced in the same manner as that of ligament and tendon, but by a different cell, the osteoblast Bone There are 206 bones in the human skeleton – 177 of these bones are involved in voluntary movement – 29 of these bones are immobile Bone The function of bone is to: – Provide support – Enhance leverage – Protect vital structures – Provide attachments for both tendons and ligaments – Store minerals, particularly calcium. Two Components of the Skeleton Axial Skeleton Skull Spinal Column Sternum Ribs Appendicular Skeleton Upper Extremity Lower Extremity Major Bone Types 1. 2. 3. 4. Long Short Flat Irregular Long Bones Characteristics – Possess a cylindrical shaft and medullary canal – Relatively broad ends – Thick walled shaft Long Bones of Skeleton Upper Extremity 1. Clavicle 2. Humerus 3. Ulna 4. Radius 5. Metacarpals 6. Phalanges Lower Extremity 1. Femur 2. Tibia 3. Fibula 4. Metatarsals 5. Phalanges Short Bones Relatively short, compact and solid structures Short Bones of Skeleton Upper Extremity Carpals (wrist) Lower Extremity Tarsals (ankle) Flat Bones Examples: Sternum Scapulae Ribs Pelvic bones Patellas Irregular Bones Examples: Bones of Spinal Column – The 24 vertebrae – Sacrum – Coccyx Characteristics of Bone Epiphyses – – Each bone has two epiphysis, which are layers of cartilage at the ends of the bones The presence of an epiphysis indicates incomplete bone growth Articulation – – Connection point of bones (joint) Type of articulation helps determine the type and amount of motion possible Pathology of bone Osteoporosis – Maybe primary or secondary Osteomalacia – Characterized by incomplete mineralization of normal osteoid tissue Osteomyelitis – An acute or chronic inflammatory process of the bone and its marrow secondary to infection Paget’s disease (osteitis deformans) – An osteometabolic disorder Cartilage Tissue Cartilage tissue consists of cartilage cells called chondrocytes – Chondrocytes are specialized cells that are responsible for the development of cartilage, and the maintenance of the extracellular matrix Cartilage tissue exists in three forms: – Hyaline – Elastic – Fibrocartilage Hyaline cartilage Covers the ends of long bones and, along with the synovial fluid that bathes it, provides a smooth and almost frictionless articulating surface The most abundant cartilage within the body Elastic cartilage A very specialized connective tissue, primarily found in locations such as the outer ear, and portions of the larynx Fibrocartilage Fibrocartilage functions as a shock absorber in both weight bearing, and non-weight bearing joints Examples include the symphysis pubis, the intervertebral disc, and the menisci of the knee Pathology of cartilage Osteoarthritis – Can be primary or secondary Osteochondritis dissecans – And osteochondral fracture Joints Joints are regions where bones are capped and surrounded by connective tissues that hold the bones together and determine the type and degree of movement between them Joints may be classified as diarthrosis, which permit free bone movement and synarthrosis, in which very limited or no motion occurs Joint Classifications Synarthrodial (immovable) Amphiarthrodial (slightly movable) – Syndesmosis – Synchondrosis Diarthrodial (freely movable) Diarthrosis This type of joint generally unites long bones and has great mobility. Examples include but are not limited to the hip, knee and shoulder and elbow joints Diarthrodial Joint Characteristics 1. 2. 3. 4. 5. Articular cavity present Joint encased within ligamentous capsule Capsule lined with synovial membrane Secretion of synovial fluid, which lubricates the joint Smooth articular surfaces, which are covered with cartilage Diarthrodial Joint Classifications 1. 2. 3. 4. 5. 6. Ball and socket (spheroidal; enthrodial) Hinge (ginglymoid) Pivot (trochoid) Condyloid (ellipsoidal) Irregular (arthrodial: plane) Sellar (saddle) Ball-and-Socket Joint Surface: – Spherical head fits into – Cup cavity of other bone Motion: Triaxial – Flexion/Extension – Abduction/Adduction – Circumduction Example: – Hip – Shoulder Hinge (ginglymus) Joint Surface: – 1 surface spool-like – 1 surface is concave and fits over spool Motion: Uniaxial – Concave surface glides partially around the spool-like process Example: humero-ulnar joint Pivot (trochoid) Joint Surface – Peg-like pivot Motion: Uniaxial – Rotation only Example: – Atlanto-axial – Radioulnar Condyloid Joint Surface: – Oval or egg-shaped convex surface – Fits into a reciprocally shaped concave surface Motion: Biaxial – Forward/backward – Side to Side Example: – wrist Irregular Joint Surface – Irregularly shaped, – usually flat or slightly curved. Motion: – Gliding (non-axial) Examples: some intercarpal joints Saddle Joint Surface: – Ends of both bones are convex – Like western saddle Motion: biaxial – Flexion/Extension – Abduction/Adduction Example: – Carpometacarpal joint of thumb Diarthrodial Joint Classifications and Axes Number of Axes Classificatio n 0 1 Nonaxial Uniaxial Irregular Hinge/ Pivot 2 Biaxial 3 Triaxial Condyloid / Saddle Ball & Socket Synovial joints The bones that articulate in a synovial joint are capped with a smooth layer of hyaline cartilage called articular cartilage. Synarthrosis There are three major types of synarthroses based on the type of tissue uniting the bone surfaces: – Synostosis joints: united by bone tissue. Examples include sutures and gomphoses – Synchondrosis joints: joined by either hyaline or fibrocartilage. Examples include the epiphyseal plates of growing bones and the articulations between the first rib and the sternum – Syndesmosis joints: joined together by an interosseous membrane. Examples include joints such as the symphysis pubis Synarthrodial Joint Characteristics Surface: – Bones are united by fibrous tissue continuous with periosteum Motion: – None permitted Example: – Sutures of the Skull Amphiarthrodial Syndesmosis Joint Characteristics Surface: – Ligamentous connection between bones Motion: – Minimal movement between bones Examples: – Inferior tibiofibular joint Amphiarthrodial Synchondrosis Joint Characteristics Surface: – Motion: – bones are united by fibrocartilage Bend &Twist Example: – Articulations between bodies of vertebrae Symphysis pubis Costochondral joints of the ribs w/ sternum Bursa Flattened sac-like structures Closely associated with some synovial joints Produce small amounts of fluid allowing for smooth and almost frictionless motion between contiguous muscles, tendons, bones, ligaments, and skin Skeletal Muscle A single muscle cell is called a muscle fiber or myofiber – Individual muscle fibers are wrapped in a connective tissue envelope called endomysium – Bundles of myofibers which form a whole muscle (fasiciculus) are encased in the perimysium. The perimysium is continuous with the deep fascia – Groups of fasiciculus are surrounded by a connective sheath called the epimysium Machinery of movement Each myofibril contains many fibers called myofilaments, which run parallel to the myofibril axis – The myofilaments are comprised of two protein filaments: actin (thin) and myosin (thick) – The A bands are composed of myosin filaments, while the I bands are composed of actin filaments Machinery of movement The actin filaments of the I band overlap into the A band, giving the edges of the A band a darker appearance than the central region (H band), which only contains myosin At the center of each I band is a thin dark Z line. A sarcomere represents the distance between each Z line Machinery of movement When a muscle contracts isotonically: – The distance between the Z lines decreases – The I band and H bands disappear – The width of the A band remains unchanged This shortening of the sarcomeres is not produced by a shortening of the actin and myosin filaments, but by a sliding of actin filaments over the actin filaments, which pulls the Z lines together Machinery of movement Cross-bridges – Structures that serve to connect the actin and myosin filaments – The myosin filaments contain two flexible hingelike regions, which allow the cross-bridges to attach and detach from the actin filament – During contraction, the cross-bridges attach and undergo power strokes, which provide the contractile force – During relaxation, the cross-bridges detach Machinery of movement The regulation of cross-bridge attachment and detachment is a function of two proteins found in the actin filaments: tropomyosin and troponin – Tropomyosin attaches directly to the actin filament – Troponin attaches to the tropomyosin, rather than directly to the actin filament For contraction to take place, the tropomyosin must be moved The energy for movement The energy required to power muscular activity is derived from the hydrolysis of ATP to ADP and inorganic phosphate. The energy for movement Three major energy systems: – Phosphagen system (anaerobic) – Glycolysis system (anaerobic) – Oxidative system (aerobic) Neuromuscular Junction Each muscle fiber is innervated by a somatic motor neuron One neuron and the muscle fibers it innervates constitute a motor unit, or functional unit of the muscle Each motor neuron branches as it enters the muscle to innervate a number of muscle fibers The area of contact between a nerve and a muscle fiber is known as the motor endplate, or neuromuscular junction Muscle contraction Release of a chemical acetycholine from the axon terminals at the neuromuscular junctions Electrical activation of the skeletal muscle fibers Release of Ca2+ from the terminal cisternae The released Ca2+ diffuses into the sarcomeres, binds to troponin, displaces the tropomyosin, and allows the actin to bind with the myosin crossbridges At the end of the contraction, the sarcoplasmic reticulum actively accumulates Ca2 which requires the degradation of adenosine triphosphate (ATP) to adenosine diphosphate. (ADP) Muscle Fiber Types Four different types of muscle fibers have been recognized within skeletal muscle: – Type I (slow twitch red oxidative) – Type IIa (fast twitch red oxidative) – Type IIb (fast twitch white glycolytic) – Type IIc (fast twitch intermediate) Slow twitch Fibers Slow twitch fibers are richly endowed with mitochondria and have a high capacity for oxygen uptake – Suitable for activities of long duration or endurance, including posture Fast Twitch Fibers Fast twitch fibers can be separated into those that have a high complement of mitochondria (Type IIa), those that are mitochondria poor (Type IIb) and those that display a mixture of characteristics (Type IIc) – Fast twitch fibers are suited to quick, explosive actions, including such activities as sprinting Pathology of muscle Muscle strains may be classified according to their severity: – Mild (first degree): involves a tear of a few muscle fibers with minus swelling and discomfort – Moderate (second degree): involves greater damage to the muscle and clear loss of strength – Severe (third degree): involves a tear extending across the whole muscle belly Pathology of muscle Myositis ossificans: is an aberrant reparative process that causes benign heterotopic ossification in soft tissue