File
advertisement

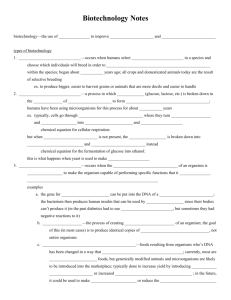
ARJUNKUMAR PJ MSc MLT 1yr IDENTIFICATION OF GRAM POSITIVE AND GRAM NEGATIVE BACTERIA Clinical sample - sample from sterile site -??? Inoculation into culture media Incubation overnight --??? Temp colonies on solid media Take a part of the colony –inoculate into peptone water –incubate 37c – 4-6h Uniform turbidity- Staphylococci Surface pellicle-Pseudomonas aeruginosa Granular turbidity- Streptococci Solid medium: Gram staining Gram positive & Gram negative bacteria Gram positive cocci ---gram positive bacilli Gram negative cocci ---gram negative bacilli Gram positive bacilli- Clostridium Corynebacterium Bacillus spp Gram positive cocci Staphylococci Streptococci Pneumococci Staphylococci- pigmentation Catalase Mannitol fermentation Coagulase test Streptococci Hemolysis on blood agar VIRIDANS STREPTOCOCCI STREPTOCOCCUS PYOGENES ENTEROCOCCI Pneumococci Capsular swelling Bile solubility test Inulin fermentation Optochin sensitivity testing Gram negative cocci- bean shaped intracellular Chocolate agar in candle jar-oxidase positive Gonococci, meningococci Summary Figure (Identification Scheme) Note: S. viridans is Is alpha hemolytic and negative for all the tests below below GRAM POSITIVE COCCI Catalase - + Staphylococcus(Clusters) Streptococcus(pairs & chains) Coagulase + S. aureus hemolytic mannitol yellow - S. epidermidis nonhemolytic (usually) mannitol white Hemolysis BETA: Bacitracin S.pyogenes (group A) + CAMP/ Hippurate + S. agalactiae (group B) ALPHA: Optochin /Bile Solubility + S. pneumoniae GAMMA: Bile Esculin + 6.5% NaCl Enterococcus + Bile Esculin + 6.5% NaCl Group D* Non-Enterococcus Group D* - (*can also be alpha hemolytic) Gram negative bacilli Family Enterobacteriaceae LF Escherichia coli, klebsiella NLF Salmonella, Shigella, Proteus Oxidase , catalase, H2S, Urease, sugar fermentation test IMViC reaction Testing for indole production is important in the identification of Enterobacteria. Most strains of E. coli, P. vulgaris, Povidencia species break down the amino acid tryptophan with release of indole. Principle: The test organism is cultured in a medium which contains tryptophan. Indole production is detected by Kovac’s or Ehrlich reagent which contains 4(p)dimethylaminobenzaldehyde. This reacts with the indole to produce a red colored compound. Media used: Peptone water or Tryptone water. Method: The media is inoculated with the test organism, indole paper strip is placed in the neck of the tube. Incubate the tube at 37°C overnight. Examine for indole production by looking for color change in the filter paper. Yellow to pink Indole production can also be done by adding Kovac’s reagent to the culture and observing for the appearance of a red color of the surface layer within 10 mins. Controls: Positive indole control: E. coli. Negative indole control: Klebsiella pneumoniae, Enterobacter aerogenes. Controls: Positive indole control: E. coli. Negative indole control: Klebsiella pneumoniae, Enterobacter aerogenes. Principle: this test detects the production of sufficient acid during fermentation of glucose by bacteria and sustained maintenance of a pH below 4.5. Procedure: the test organism is inoculated in glucose phosphate broth and inoculated at 37°C for 2-5 days. Then add five drops of 0.04% solution of methyl red, mix well and read the results immediately. Interpretation: Positive: Red colour Negative : Yellow color These tubes show the results of a typical methyl red test. Tube A. Methyl red negative Tube B. Methyl red postive Positive control: E. coli, Listeria monocytogenes Negative control: Klebsiella, Enterobacter spp. Principle: This test depends on the production of acetyl methyl carbinol (acetoin) from pyruvic acid in the media. In the presence of alkali and atmospheric oxygen, acetoin is oxidized to diacetyl which reacts with α-naphthol to give a red color. Method: Test organism is inoculated in glucose- phosphate broth and incubated at 37°C for 48 hrs. Then add 1 ml of 40% KOH and 3 ml of α-naphthol in absolute alcohol. Interpretation: Positive: Pink color within 2-5 minutes deepening to crimson color in 30 minutes. Negative: Colorless for 30 mins These tubes show the results of a typical Voges-Proskauer test. Tube A. Voges-Proskauer positive Tube B. Voges-Proskauer negative Positive control: Klebsiella sp., Enterobacter sp., Staphylococcus. Negative control: E. coli, Micrococcus. Principle: It is the ability of an organism to utilize citrate as the sole source of carbon for its growth., with resulting alkalinity. Procedure: Solid Simmon’s citrate media is used. A bacterial colony is picked up by a straight wire and inoculated into the media. Incubated at 37°C for overnight. Interpretation: Positive: Growth with an intense blue color on the slant. Negative: No growth with any change in color (green). Positive control: Klebsiella sp., Salmonella sp. except Salmonella typhi, Citrobacter sp., Negative control: E. coli, Salmonella typhi. Principle: To determine the ability of an organism to produce an enzyme urease which splits urea to ammonia. Ammonia makes the medium alkaline and thus phenol red indicator changes to pink/ red in color. Method: The test is done in Christensen’s urease medium. The test organism is inoculated on the entire slope of medium and incubated at 37°C. it is examined after 4 hours and after overnight incubation. Interpretation: Positive – pink color Negative- pale yellow. Positive controls: Klebsiella sp., Proteus sp., Helicobacter pylori. Negative control: E. coli, Yersinia pestis. Principle: To determine the presence of an enzyme cytochrome oxidase which catalyses the oxidation of reduced cytochrome by molecular oxygen. Method: Freshly prepared solution of 1 % tetra – methyl paraphenylene diamine dihydrochloride (oxidase reagent) is used. A filter paper strip, soaked in the oxidase reagent, is smeared with test organism. In a positive oxidase reaction the smeared area turns deep purple within 10 seconds. Interpretation: Positive: deep purple within 10 secs. Negative: – No color change Positive control: Pseudomonas sp., Vibrio sp., Alcaligenes sp. Negative control: All members of Enterobacteriaceae. Principle: certain bacteria have an enzyme catalase which acts on hydrogen peroxide to relase oxygen. Method: pick up a few colonies of test bacteria with platinum loop from a nutrient agar plate and mix it with a drop of H2O2 (10 volumes) on a clean glass slide. Interpretation: Positive test: Immediate bubbling easily observed Negative test: No bubbling Positive control: Staphylococcus, Micrococcus, all members of Enterobacteriaceae except Shigella dysentriae. Negative control: Shigella dysenteriae typeI, Streptococcus, Clostridium. Principle: To determine the ability of an organism to ferment a specific carbohydrate (sugar) incorporated in a medium producing acid or acid with gas. Method: Test organism is inoculated in a sugar medium and inoculated at 37°C for 18-24 hrs. glucose, lactose, sucrose and mannitol are widely used sugars. Sugar media contain 1% sugar. Indicator used is Andrade’s indicator Interpretation: Positive: pinkish –red color (acidic) Negative: Yellow to colorless (alkaline) Gas production can be seen as bubbles in Durham’s tube Examples of fermentation bacteria: Glucose fermenters: All members of the Enterobacteriaceae Glucose and lactose fermenters: E. coli, Klebsiella sp. Glucose and mannitol fermenter: Salmonella sp. Beta-hemolytic Streptococcus are spherical bacteria that produce hemolysins capable of completely lysing (bursting open) red blood cells. When grown on sheep blood agar, colonies of betahemolytic Streptococcus are encircled by visible areas of clearing where beta hemolysis has occurred. Beta-hemolytic streptococci may be pathogens or nonpathogens. Group A Streptococcus (Streptococcus pyogenes) causes "strep throat". Strep throat may lead to delayed sequelae such as rheumatic fever, glomerulonephritis, and/or scarlet fever. The bacitracin susceptibility test is used to distinguish Group A streptococci, which cause ninety percent of acute streptococcal infections in humans, from other streptococci. When grown on blood agar, Group A streptococci are sensitive to (killed by) the antibiotic bacitracin . A sterile disk impregnated with bacitracin is placed on the first sector of an isolation plate before incubation. A zone of inhibition (area with no growth) will be seen around the disk after incubation if the organism is a Group A beta-hemolytic Streptoccus. Other beta-hemolytic streptococci are resistant to (not killed by) bacitracin. Their colonies will thus grow right up to the disk of bacitracin. Chocolate Agar plate Group A Streptococcus and Group C Streptococcus with bacitracin disks Coagulase is an enzyme that catalyzes the formation of a fibrin clot in plasma. The presence of coagulase can be detected by heavily inoculating the test organism into rabbit plasma and incubating the mixture for 4 to 24 hours. Any degree of clotting during this time, from a loose clot suspended in the plasma to a solid, immovable clot is a positive result. Staphylococcus aureus produces coagulase Staphylococcus epidermidis does not. 1. Negative Coagulase Test 2. Positive Coagulase Test Triple Sugar Iron Agar (TSI) Are used to determine if bacteria can ferment glucose and/or lactose and if they can produce hydrogen sulfide or other gases. (If an organism can ferment glucose, it is "glucose positive". If it ferments lactose, it is "lactose positive".) In addition, TSI detects the ability to ferment sucrose. These characteristics help distinguish various Enterobacteriacae, including Salmonella and Shigella, which are intestinal pathogens. TSI contains three sugars: glucose, lactose and sucrose. Lactose and sucrose occur in 10 times the concentration of glucose (1.0% versus 0.1%). Ferrous sulfate, phenol red (a pH indicator that is yellow below pH 6.8 and red above it), and nutrient agar are also present. The tube is inoculated by stabbing into the agar butt (bottom of the tube) with an inoculating wire and then streaking the slant in a wavy pattern. Results are read at 18 to 24 hours of incubation. Reading the Results A yellow slant on TSI indicates the organism ferments sucrose and/or lactose. On KIA a yellow slant indicates the organism ferments lactose. (Because KIA does not contain sucrose, sucrose fermentation is not detected with KIA tests.) Other results are the same for TSI and KIA. A yellow butt shows that the organism fermented glucose. Black preciptate in the butt indicates hydrogen sulfide production. Production of gases other than hydrogen sufide is indicated either by cracks or bubbles in the media or the media being pushed away from the bottom of the tube. Understanding the Results If an organism ferments glucose only, the entire tube turns yellow due to the effect of the acid produced on phenol red. Because there is a minimal amount of glucose present in the tube, the organism quickly exhausts it and begins oxidizing amino acids for energy. Ammonia is thus produced and the pH rises. Within 24 hours the phenol red indicator reverts to its original red color on the slant. Because TSI/KIA media is poured as a deep slant, the butt has limited oxygen and bacteria are unable to oxidize amino acids there. The butt thus remains yellow. If an organism can ferment lactose and/or sucrose, the butt and slant will turn yellow (as they do from glucose fermentation). However, they remain yellow for at least 48 hours because of the high level of acid products produced from the abundant sugar(s). KIA resembles TSI in all respects except that KIA contains two sugars (lactose and glucose) while TSI contain three sugars (lactose, glucose and sucrose). Like TSI media, KIA contains 10 times as much lactose as glucose. Thus KIA tests for an organism's ability to ferment glucose or lactose but not sucrose. If the gas being produced is hydrogen sulfide (H2S), it reacts with the ferrous sulfate and precipitates out as a black precipitate (ferric sulfide) in the butt. Organisms producing large amounts of hydrogen sulfide (e.g. Salmonella and Proteus) may produce so much black precipitate that it masks the yellow (acid) color of the butt It is a differential indicator medium used for the differentiation of lactose fermenters from non lactose fermenters It consists of 2% peptone, lactose, neutral red indicator and sodium taurocholate. It is used to distinguish lactose fermenting from Non – lactose fermenting bacteria.