Histology of urinary system 2010
advertisement

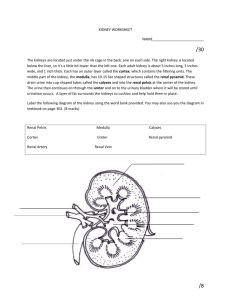
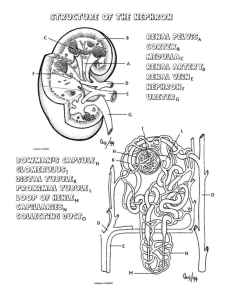
HISTOLOGY OF THE URINARY SYSTEM Prof. Dr. Fauziah Othman Department of Human Anatomy Faculty of Medicine and Health Sciences Universiti Putra Malaysia Kidney * Parts of nephron and structures Juxtaglomerular apparatus Functional aspects Blood circulation Ureter and urinary bladder • General features Urinary epithelium Urethra * Structure of male and female urethra Kidney Main organ of the excretory system Kidney is built of billions of little tubes called the nephrons. At the beginning of each nephron, a web of capillaries releases much water and other molecules into the nephron. The urine is collected in the urinary bladder and, when it fills up, it is excreted via urethra into the outside environment. Kidney's Internal Structure Cortex -- the outer part of the kidney; Medulla -- the inner portion of the kidney; Pyramids -- the triangular-shaped divisions of the medulla of the kidney; Papilla -- narrow, innermost tip of the pyramid; Pelvis -- the kidney or renal pelvis is an extension of the upper end of the ureter (the tube that drains urine into the bladder); Calyx -- each calyx is a division of the renal pelvis; opening into each calyx is the papilla of a pyramid. basic structural and functional unit of the kidney. Its chief function is to regulate the concentration of water and soluble substances like sodium salts by filtering the blood, reabsorbing what is needed and excreting the rest as urine. A nephron eliminates wastes from the body, regulates blood volume and blood pressure, controls levels of electrolytes and metabolites, and regulates blood pH. Its functions are vital to life and are regulated by the endocrine system by hormones such as antidiuretic hormone, aldosterone, and parathyroid hormone. microscopic units of a kidney, have 2 main parts, 1. 2. renal corpuscle (Bowman's capsule with glomerulus) renal tubule. RENAL CORPUSCLE glomeruli surrounded by Bowman's capsules. Bowman's capsule -- the cup-shaped top of a nephron. It is the sack-like Bowmans's capsule that surrounds the glomerulus. Glomerulus -- a network of blood capillaries tucked into Bowman's capsule. Juxtaglomerular apparatus The juxtaglomerular apparatus is a microscopic structure in the kidney, which regulates the function of each nephron. There are three cellular components of the apparatus which are the; 1. 2. 3. macula densa, extraglomerular mesangial cells, juxtaglomerular cells (also known as granular cells). RENAL TUBULE Proximal convoluted tubule -- the first segment of a renal tubule, called proximal because it lies nearest the tubule's origin from Bowman's capsule, and convoluted because it has several bends in it. Loop of Henle -- the extension of the proximal tubule; observe that the loop of Henle consists of a straight descending (directed downward) limb, a loop, and a straight ascending limb (directed upwards). Cont. Distal convoluted tubule -- the part of the tubule distal to the ascending limb of Henle. It is the extension of the ascending limb of Henle. Collecting tubule -- a straight (not convoluted) part of a renal tubule; distal tubules of several nephrons join to form a single collecting tubule Histology Bowman's capsule Cells of the outer or parietal layer of Bowman's capsule form a simple squamous epithelium. Cells of the inner layer, podocytes in the visceral layer, are extremely complex in shape. Small foot-like processes, pedicles, of their cytoplasm form a fenestrated epithelium around the fenestrated capillaries of the glomerulus. The openings between the pedicles are called filtration slits. They are spanned by a thin membrane, the filtration slit membrane. Between the podocytes and the endothelial cells of the capillaries a comparatively thick basal lamina, which can be subdivided into an outer lamina externa, a middle lamina densa and an inner lamina interna. The basal lamina and the slit membranes form the glomerular filtration barrier, which prevents some large molecules from entering the capsular space between the outer and inner epithelial layers of Bowman's capsule. Mesangial cells in the glomerulus form the connective tissue that gives structural support to podocytes and vessels. Histo: proximal tubule walls - low columnar epithelium. The eosinophilic cells of the epithelium have a wide brush border and are active in endocytosis. Histo of Loop of Henle It is 'U' shaped and has descending and ascending segments. Thin descending segment has flattened epithelium( squamous). It is permeable to water but not solutes. Histo: Distal convoluted tubule straight part of the DCT is formed by the low cuboidal cells without a brush border. The diameter of the tubule gradually expands to about 35 microns. convoluted part and comes in contact with the Glomerulus forming the Macula Densa. Nephron structure characteristic Renal corpusle Capillary ball covered by podocyte & surrounded by simple squamous epithelial capsule, capsular space. Proximal convulated Lined with simple cubodial epithelium & prominent brush border Loop of Henle Tubule that form a loop, there are thick & thin ascending & desecnding portion; the most distal part of the loop often extends into the medulla. Thick limb are lined with simple squamous/ cuboidal epithelium Thin limb are lined with simple squamous epithelium Distal convulated Lined with simple cuboidal with only sparse brush border; cytoplasm of cells tend to be paler than that of proximal convulated Ureter The wall of the ureter is made 3 layers. From inside outwards they are : 1. Mucosa- which is made up of epithelium & lamina propria 2. Muscular coat – made of smooth muscles 3. Fibrosa – made of fibrous connective tissue Mucosa- is thrown into folds and thus gives the appearance of star shaped lumen. 1. Transitional epithelium. 3-5 layers thickness. 2. Lamina propria- dense, irregular layer of fibroelastic connective tissue The epithelium is separated from the lamina propria by a basal lamina. Muscular layer – Upper 2/3 of the ureter is made of two layers of smooth muscle cells. Inner longitudinal and outer circular layer( in contrast to the wall of GIT which has inner circular & outer longitudinal !). Lower 1/3 of the ureter has a third outer layer of longitudinal muscles( inner longitudinal, middle circular, outer loingitudinal ). Fibrous coat – is made up of fibrous connective tissue The urethra: Female: relatively short, exits just anterior to the vagina Male: longer, divided into three sections the prostatic, membranous and spongy urethra. The prostatic urethra is enclosed in the prostate gland. The membranous urethra is a short section that penetrates the urogenital diaphragm. The spongy urethra or penile urethra extends from the membranous urethra to the external urethral orifice (meatus). Histology: In both male and females the urethra starts out as transitional cell but quickly becomes stratified squamous in the female. The male urethra is more variable but ends up stratified squamous as well. Histology of the bladder mucosa of transitional epithelium, Submucosa, and thick muscular layer know as the detrusor muscle Clinical correlates Urinary incontinence Childbirth and other events can injure the scaffolding that helps support the bladder in women. Pelvic floor muscles, the vagina, and ligaments support your bladder. Overactive bladder Specifically, the symptoms of overactive bladder include urinary frequency—bothersome urination eight or more times a day or two or more times at night urinary urgency—the sudden, strong need to urinate immediately urge incontinence—leakage or gushing of urine that follows a sudden, strong urge nocturia—awaking at night to urinate