Teens Talk Fat Minority Students & their Families Discuss
advertisement

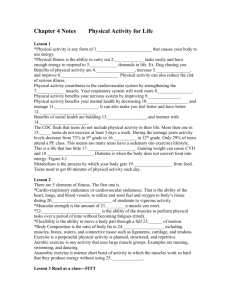
Special Thanks to: Chicago Community Trust & Washington Square Health Foundation for their support and funding. Helping us get one step closer to our goal. WHY TALK FAT? Origins of the Project 1. Growing awareness of obesity as a national problem National Concerns • Doubling of obesity rates • Associated increase of Type 2 Diabetes • Anticipated increase of cardiovascular disease, orthopedic problems, and depression Percent of Teens who fall above the 85th or 95th %ile for BMI 35.00% 30.00% 25.00% 20.00% 15.00% 10.00% 5.00% 0.00% AA boys AA girls 85% Mex. Boys 95% Mex girls ACHN SBHC vs. NHANES, Percent of Teens >95%ile BMI 35 30 25 20 15 NHANES 10 SBHCs 5 0 A.A. boys A.A. girls M.A. boys M.A. girls WHY TALK FAT? Origins of the Project 1. Growing awareness of obesity as a national problem 2. Observation in our own clinics of large numbers of overweight youth 3. Need to address diabetes prevention and diagnosis Where Will Intervention Take Place: School-Based Health Center(SBHC) • Provide ease of access and familiarity to students and families • Students receive comprehensive health care services • Patient population with increased risks for obesity and diabetes (40% of 1st or 2nd degree relatives with diabetes) What is STRIDE? Smart Teens Reducing the Incidence of Type 2 Diabetes, Etc. • SBHC obesity intervention and behavior change program • Context: Enhanced diabetes screening study • Focus: Healthy eating & increase of physical activity • Method: Adult and teen focus groups drawn from 3 urban high schools with SBHC Teens Talk Fat Minority Students & their Families Discuss Experiences and Ideas for Healthy Eating and Physical Activity From the Cook County ACHN N. Fritz, S. Corbin, C.Stahl, N. Mourikes, M. Driscoll Focus Groups • PURPOSE: Use adult and teen opinions to guide development of interventional program to reduce diabetes risks Focus Group Recruitment • FOCUS GROUP Students were recruited via classroom, hallway fliers, patient contact, word of mouth, and referral from providers Parents were recruited via their children, at report card pick-up and clinic registration, and from pre-existing school based parent groups Focus Group • REVIEW Groups were held between November 2001January 2002 1 student and 1 parent group from each of 3 schools Group leader matched by ethnicity Groups of 7-17 participants Groups lasted 1-2 hours Healthy foods served Focus Groups con’t • Focus group questions addressed: Participants’ experience with diet or exercise change Knowledge of community resources for eating and physical activity Participants’ opinions about useful intervention strategies in the SBHCs Focus Group • METHODS: Discussions were audio recorded Tapes reviewed by all investigators independently and themes identified Transcriptions of discussions were also reviewed Analysis: • Particular attention to: Common themes across groups Differences between AA and Latino groups Differences between teens and parents Results: All groups • • • • • 71 participants 19 males, 52 females 36 teens, 35 parents 22 Latinos, 49 African-Americans Most participants were overweight Results: Observations • Many participants expressed a concern for better health and nutrition • All participants were able to list community resources • All participants tried the “healthy” foods that were provided Themes 1. Feeling unable to sustain healthy choices “One of my ex-boyfriends got me one of those things you put your feet on, and I sold it . Then he got me an old stationary bike. . And I sold that too..” “I don’t like walking. I tried sit-ups. I even tried the cha-cha-cha dance….I am just lazy…” “It’s like when you try…OK, you’re trying..” Themes 2. Denial there’s a problem “I don’t want to talk about diabetes – it scares me.” “My doctor tells me to lose weight; But I’m happy with how I am. I don’t want anyone telling me how I should be . .” Themes 3. Knowledge deficits “For a while I tried to stop drinking pop so I switched to juice” “Regular salt is bad for you – you have to buy sea salt from the health food store, it’s better” Themes 4. Expediency of junk food: “If the junk food’s there, you just eat it…” “If you put healthy food in the machines, don’t SAY it’s healthy. . .or people won’t buy it. . .they’ll be afraid it tastes nasty.” Themes 5 Community resources identified and concerns about these resources (healthy eating): “Our neighborhood is ghetto, we don’t sell that stuff. They sell spoiled, rotten meat and stuff.” “Basically, in our neighborhood, you really can’t buy fresh vegetables from there because they are not fresh . . .” Themes 6. Suggestions for programmatic supports: Some sort of group—a support group, cooking group, restaurant field trip group, dance/drama group, etc. Use of school facilities as a resource Very few suggestions regarding provider input Results: Teen Groups • There were a total of 36 teens (9 male, 27 female) • 22 African-American and 14 MexicanAmerican teens • 2/3 of the teens were overweight • Most of the teens had family hx of diabetes, as well as, personal experience with dieting and weight loss Results: Teen Groups con’t • Most teens expressed a concern for their health and nutrition • Most teens did not eat meals provided by the schools’ cafeteria • Most teens were eager to make changes, but also wanted the support needed to make these changes Results: Adult Groups • There were a total of 35 adults (10 male, 25 female) • 10 Mexican-American and 25 AfricanAmerican adults • 2/3 of the adults were overweight • Some of the adults were diabetic, most had family hx of diabetes and had some experience with dieting/weight loss Contrasts: Adults & Teens • Parents were more concerned about safety issues in the community than were teens. • Parents were less likely to try the various healthy snacks provided during the groups. Contrasts: African-Americans & Mexican-Americans • Mexican-American teens expressed more dissatisfaction about their physical appearance than did the African-American teens • Mexican-American parents were more open to changing their eating/cooking habits than the African-American parents • African-American teens but NOT parents were more likely to deny obesity as a problem. Conclusions: Intervention needs to • Address psychological barrier of hopelessness • Build interpersonal support groups • Address school environmental issues: lunch, vending machines, PE classes, after school opportunities • Education is important but insufficient • Support development of change agents among youth, parents, and staff