Medical Surveillance in Occupational Health
advertisement

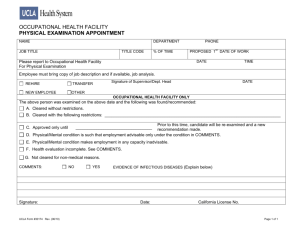
Medical Surveillance JOSEPH J. SCHWERHA MD MPH PROFESSOR OF OCCUPATIONAL AND ENVIRONMENTAL MEDICINE DIRECTOR OF THE OCCUPATIONAL AND ENVIRONMENTAL RESIDENCY PROGRAM GRADUATE SCHOOL OF PUBLIC HEALTH UNIVERSITY OF PITTSBURGH Occupational Health surveillance entails the systematic monitoring of health events and exposures in working populations in order to prevent and control occupational hazards and their associated diseases and injuries. Surveillance derives from the French word surveiller, “to watch over,” which encompasses the twin notions of careful observation and timely intervention. The four essential components of Occupational Health surveillance are: • To gather information on cases of occupational diseases and injuries and on workplace exposures • To distill and analyze data • To disseminate organized data to necessary parties, including workers, unions, employers, governmental agencies, and the public; and • To intervene on the basis of data to alter the factors that produced these health events and hazards Current Occupational Health Surveillance Activities in the U.S.A. • Death Certificates • Hospital Discharge Data • Physicians’ Reports: A sentinel provider is a physician or other health provider (or facility) who, due to their specialty or geographic location, is likely to provide care for workers with occupational disorders. As a part of SENSOR at present, NIOSH provides support to 14 states to develop surveillance systems for 12 occupational conditions, including silicosis, amputations, asthma, burns, cadmium poisoning, carbon monoxide poisoning, carpal tunnel syndrome, childhood injuries, dermatitis, noise-induced hearing loss, pesticide poisoning, and tuberculosis. Surveillance Activities continued • • • • • Laboratory Reports Workers’ Compensation Reports National Surveys Employer Surveillance Programs Occupational Health Clinics Occupational Hazard Surveillance Activities in the United States • OSHA Integrated Management Information System • NIOSH National Hazard Surveys Evaluations for Specific Occupational Exposures and Diseases Assessment The type of occupational health programs needed by any business is directly dependent on the goals, activities, and operations of that organization. Needs Assessment The first stage of medical surveillance is needs assessment. “Do certain workers need special tests?” Assessment of Factors Outside the Workplace * disinfectants * cleaning agents * paint removers * wax strippers * solvents * pesticides * emissions from heating or cooling devices * sunlamps * a wide variety of materials used in painting, ceramics, printmaking, sculpture and casting, welding, stained glass, woodworking, photography, and many forms of commercial art Medical Surveillance 1. Upon initial assignment or institution of medical surveillance: a. General physical examination performed b. Medical history taken, including the following topics: (1) alcohol intake (2) past history of hepatitis (3) work history and past exposure to hepatotoxic agents (4) past history of blood transfusions (5) past history of hospitalizations Medical Surveillance continued c. A serumspecimen obtained, determinations made of: (1) Total bilirubin (2) Alkaline phosphatase (3) Serum glutamate oxalacetic transaminase -SGOT (4) Serum glutamate pyruvic transaminase - SGPT (5) Gamma glutamyl transpeptidase (6) Acute test necessary to maintain an exposure Medical Surveillance continued 2. Examinations provided shall be performed to least a. Every 6 months for certain conditions b. Annually or age related c. Government regulated d. On the physician’s discretion 3. Each employee exposed to an emergency shall be afforded appropriate medical surveillance. Medical Surveillance continued 4. A statement of each employee’s suitability for continued exposure, including use of protective equipment and respirators, shall be obtained from the examining physician promptly after each examination. A copy of the physician’s statement shall be provided each employee. Medical Surveillance continued 5. If any employee’s health would be materially impaired by continuous exposure, each employee shall be withdrawn from possible contact. 6. Laboratory analyses for all biologic specimens included in medical examinations shall be performed in laboratories licensed under 42 CFR Part 74. Medical Surveillance continued OHS’s must have available for staff use, in writing, preferably in a manual, the following desiderata: (1) the type of examination (complete or partial, general or specific) (2) the interval history items to be reviewed (3) the periodicity (4) the organ system or organs to be given special scrutiny (5) the hematologic, urine, biochemical, fecal, radiographic, cytologic, or breath analytic procedures to be completed Medical Surveillance continued (6) acceptable levels for each test result (7) the interval between a test productive of an abnormal leave and the repetition of the test (8) the time of specimen collection (9) the persons to be notified in the event of abnormal findings (10) other actions to be taken Objectives of Occupational Health Services • To protect the health and well-being of workers against the stressors and potential health hazards of the work environment. • To place job applicants or current employees in work commensurate with their physical and emotional capacities, work that can be performed without endangering the worker or fellow employees and without damaging property. • To provide emergency medical care for injured or ill workers and definitive care and rehabilitation for those with workgenerated injuries or illnesses, in keeping with the medical, surgical, or psychotherapeutic expertise of the staff, medical department policy, managerial policy, and the availability of community resources. Objectives of Occupational Health Services continued • To maintain or improve the health of the worker through promotional, educational, counseling, or informational activities, preventive health measures including fitness or wellness programs, and periodic clinical reviews of health status. • To promote improved health among family members. Biological monitoring is the measurement of a chemical, its metabolite, or a nonadverse biochemical effect in a biological specimen for the purpose of assessing exposure. Advantages of Biologic Monitoring 1. It is an attempt to measure the parameter most directly related to potential health effects. Results can aid in formulating a more refined estimate of risk of illness secondary to exposure. 2. Nonoccupational exposures and individual variability are assessed. 3. Multiple exposures and other routes of exposure, such as dermal and ingestion, can be evaluated. Limitations of Biologic Monitoring 1. Effectiveness is dependent on adequate toxicologic data. 2. Test results can be affected by other factors such as alcohol and pregnancy. Cigarette smoking can also interfere with monitoring results. Workers who smoke cigarettes, for example, may have levels of cadmium higher than their nonsmoking counter parts. 3. For some substances, relatively short biologic halflives affect the monitoring. 4. Monitoring is ineffective for surface-acting agents such as sulfur dioxide and ammonia. Variety of Periodic Medical Examinations continued Association of Occupational and Environmental Medicine Clinics (AOEC) found the following three questions essential: 1. Please describe your job 2. Have you ever worked with any health hazard, such as asbestos, chemicals, noise, or repetitive motion? 3. Do you have any health problems that you believe may be related to work? Work and Exposure History • Focus on the job when the patient first began having symptoms • Patient’s job title (or occupation): it is important to know the nature of the job • “Tell me what you do on your job?” • “Is there anything you do now that is different from past jobs where you’ve been an [electrician]?” • Specific exposures: the exposure history requires further study to identify specific constituents of products and exposure levels. • Assessment of relative levels of exposure (i.e., low, medium, high) for specific agents can be valuable Work History • Change in symptoms during the work day. • Change in symptoms over the work week. • Change in symptoms on weekends and on vacations. • Onset of symptoms away from work. • Other experiences with work-related events. Clinical Environmental Medicine Environmental medicine can be considered to be “the study of effects upon human beings of external physical, chemical, and biologic factors in the general environment”. Clinical environmental medicine, then, would be “the study of detectable human disease or adverse health outcomes from exposure to these environmental factors”. The discipline of environmental medicine “combines clinical epidemiologic, and toxicologic approaches. It uniquely seeks to understand external causation and then to adopt policy, engineering, or human factor interventions to prevent or mitigate the caused outcomes”. Principles of Occupational and Environmental Disease • The clinical and pathologic expression of most environmentally caused diseases are indistinguishable from those of nonenvironmental origins. • Many diseases of occupational or environmental cause are multifactorial, with nonenvironmental factors playing a role. • The effects of occupational and environmental exposures occur after a biologically predictable latent interval following exposure. Principles of Occupational and Environmental Disease continued • The dose of an exposure to a noxious agent is a strong predictor of the likelihood and type of effect • People differ substantially in their responses to noxious exposures. The Environmental Evaluation 1. Lack of specificity about the identity of hazards 2. Inadequate information about exposure level 3. Recall biases (greater attention to exposures that were at the time bothersome or otherwise are perceived as being casual) 4. Other biases, e.g., patients fearful of possible job loss may under-report exposures, and litigants may exaggerate the intensities of exposures and their apparent effects The Environmental Evaluation continued This additional information serves several purposes: 1. To learn the true chemical or physical hazards to which the patient has been exposed 2. To establish information about the dose of exposure 3. To corroborate or modify the information that has been obtained directly from the patient. The Environmental Evaluation Issues about confidentiality should always be considered: • Prior medical records • Exposure records from an employer • Health and regulatory agencies • Unions and community groups • Direct site visit Exit Examinations The structure and content of exit examinations most closely mirrors that of the periodic medical examination. Exit examinations tend to be either target-organ or substance specific and frequently are used by employers to document that the employee has suffered no adverse health effects from employment or to establish the extent of any such effects. Record Keeping 1. Medical surveillance a. Establish and maintain a medical record for each employee b. The record shall include: (1) Name, SSN, and description of employee duties (2) Copy of medical examination results (3) Copy of the physician’s written opinion (4) Complaints related to exposure (5) Protective devices worn and length of time worn (6) Copy of the standard and its appendices c. The employer must maintain the record for at least 30-50 yrs Summary of Occupational and Environmental History and Examinations Occupational and environmental histories and examinations serve two main purposes in occupational health practice. The first is to help place and maintain people in work that is commensurate with their physical and mental capabilities. The second usage is to monitor individuals exposed to environmental hazards associated with work-related diseases. To a greater or lesser extent, all occupational and environmental evaluations contain three basic components: the occupational environmental history, the medical history and review of systems, and the physical examination.