ST120 Fundamentals of Pathophysiology
advertisement
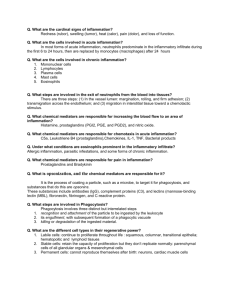
Surgical Pathology Fundamentals Concorde Career College, Portland ST120 Adapted from “Pathology” by Kansas State University Terminology Pathology: The study of the structural and functional changes leading to disease in: • Cell • Tissue • Organs Pathophysiology: Is the abnormal function of organs or systems due to disease Cell structure Terminology Pathology is divided • General • Special or systemic General pathology: Basic reaction of cells and tissue to normal stimuli Specific pathology: Specific response special organs to well defined stimuli Four aspects of disease process 1. 2. 3. 4. Etiology Pathogenesis Morphological changes Clinical significance 1.Etiology A) Determining cause Specifically known to be the soul cause of disease, such as a pathogenic organism, e.g., HIV B) Predisposing causes Leading indirectly to disease such as genetic predisposition 2.Pathogenesis Is the mechanism by which a certain etiological factor causes disease (In Greek: pathos = disease, genesis = development). Some forms of pathogenesis are: Inflammation Malignancy Tissue breakdown 2.Pathogenesis The pathogenesis process leads to the formation of a lesion Lesion is derived from the Latin word "laesio" which means "injury." Lesions are a result of damage to tissues. For example: A cancerous tumor is an example of a lesion The surrounding tissue damaged by a tumor is also termed a lesion. 3.Morphological changes Are the changes that occur in the cell tissue or organ as a result of the pathological process These changes can be Morbid: Macroscopic appearance visible to the naked eye 3.Morphological changes Are the changes that occur in the cell tissue or organ as a result of the pathological process Or Histological: Microscopic appearance only visible under the microscope 4.Clinical significance What impact do these changes have on the patient? Progression of a disease Complete cure Death Complication Additional pathological changes which may occur during or after the course of any disease Pathological investigation During life Surgical biopsy Fine needle aspiration biopsy (FNAB) Cytopathology Molecular techniques After death Autopsy Exposure to stress (irritant) Mild irritant Moderate Severe irritant A) inflammation B) Degeneration Necrosis Necrosis Types of irritants Living irritant: Bacteria Pathogenic fungi Parasite Virus Helminths Non-living irritant: Physical Chemical Trauma, Burns, Radiation Acids, Alkalies Immunological Ag-Ab reaction Hypersensitivity reaction Chemical burns Inflammation It is the response of the living tissue to mild to moderate irritant The response is directed to defend the tissue for foreign irritants and to prevent further damage The aim is to bring more blood to the damaged area by acceleration of the blood stream It is denoted by the suffix “itis” Inflammation Examples of inflammation Tonsillitis Appendicitis Tendonitis ,………etc. Lung? Tonsillitis Inflammation Exudate An exudate is any fluid that filters from the circulatory system into lesions or areas of inflammation Its composition varies but generally includes water and the dissolved solutes of the blood, some or all plasma proteins, white blood cells, platelets and RBC Transudate A fluid that passes through a membrane which filters out much of the protein and cellular elements to yield a watery solution. A transudate is due to increased pressure in the veins and capillaries pressure forcing fluid through the vessel walls or low levels of protein the blood serum The transudated fluid accumulates in tissues outside the blood vessels and can cause edema Types of Exudate 1. Serous exudate is usually seen in mild inflammation, with little protein content; seen in certain disease states like tuberculosis 2. Purulent or suppurative exudate consists of plasma with both active and dead neutrophils, fibrinogen, and necrotic parenchymal cells; referred to as pus. 3. Fibrinous exudate is composed mainly of fibrinogen and fibrin. It is characteristic of rheumatic carditis, but is seen in all severe injuries such as strep throat and bacterial pneumonia 4. Hemorrhagic exudate is seen in injury that causes rupture of blood vessels. 5. Pleural 6. Catarrhal exudate is seen in the nose and throat and is characterized by a high content of mucus. Purulent Exudate Inflammation Effects of inflammation Vascular phenomena 1. 2. 3. 4. Transient vasoconstriction rapidly followed by Vasodilatation Stasis Migration of leucocytes Inflammation Composition and function of inflammatory fluid exudates Fluid exudates Dilution of bacterial toxins fibrin threads : help the movement of leucocytes and limit the spread of infection Also contain antibodies Inflammation Composition and function of inflammatory fluid exudates Cellular part Phagocytosis: engulfing of and destruction of bacteria and necrotic tissue by phagocytes and PNL Inflammation Chemotaxis: the movment of WBCs in the area of inflammation towards the irritant Emigration of leukocytes: the migration of WBC from within the blood vessel towards the inflammation site Diapedesis: the passage and movement of RBCs from within the blood vessel towards the inflamed area Cardinal signs of inflammation Redness (rubor) Hotness (calor) Edema (tumor) swelling due to inflammatory exudate Pain (dolor) due to pressure of edema on nerves and irritation of nerve endings by metabolites Loss of function (functio laesa) this is to make the inflamed part of tissue rest and heal Types of inflammation Acute inflammation Acute non-suppurative inflammation: acute without the formation of pus Acute suppurative inflammation: with pus Localized : Abscess, Furuncle, Carbuncle Diffused : cellulitis, septic meningitis Chronic inflammation Chronic specific : TB Chronic non-specific: follows acute or chronic from the beginning Cells of inflammation Acute inflammation cells: 1- RBC 2- PNL (leukocyte) Eosinophils Basophils Neutrophils Chronic inflammation cells 1- lymphocytes 2- Plasma cells 3- Histocytes 4- fibroblasts Leukocyte review http://en.wikipedia.org/wiki/ White_blood_cell Neutrophil engulfing anthrax bacteria Cells of inflammation Fate of acute inflammation 1- Regression: by resolution, for example when the body (immune system) overcomes bacterial infection 2- Progression: can lead to chronic inflammation and spread; the bacteria overcome the immune system and can spread by: Blood: septicemia, bacteremia, toxemia pyemia Lymphatyic: lymphangitis, lymphadenitis Direct: to other surrounding tissue Type of cells Labile cells: epithelium, haematopoietic (blood) Quiescent (Stable): hepatic, kidney and pancreas Non-dividing (Permanent): nerve cells and skeletal muscle cells Cell development Proliferation: increased number Differentiation: development through stages Healing Tissue repair involves replacement of damaged tissue with new healthy living tissue when resolution cannot occur Types Usually involves two separate but coordinated components A) Regeneration: healing by the same type of tissue cells from surrounding healthy living cells; this occurs following damage to labile cells and stable cells, for example, liver cirrhosis and bone fractures B) Fibrous (scar tissue): healing by granulation tissue (fibroblast with new capillaries formed) which mature into vascular fibrous tissue (scar); this occurs in the healing process of permanent cells and stable cells with extensive damage, for example, myocardial infraction and open wounds Introduction to wound healing Healing is a complex and dynamic process of restoring cellular structures and tissue layers. The adult wound healing process can be divided into 4 distinct phases: Hemostasis phase Inflammatory phase Proliferative phase Remodeling phase Sequence of events in healing Initial phase - Hemostasis Following vasoconstriction, platelets adhere to damaged endothelium and discharge adenosine diphosphate (ADP), promoting thrombocyte clumping, which dams the wound. The inflammatory phase is initiated by the release of numerous cytokines by platelets. Fibrinogen is cleaved into fibrin and the framework for completion of the coagulation process is formed. Fibrin provides the structural support for cellular constituents of inflammation. This process starts immediately after the insult and may continue for a few days. Sequence of events in healing Second phase - Inflammation Within the first 6-8 hours, the next phase of the healing process is underway, with polymorphonuclear leukocytes (PMNs) or PNLs engorging the wound These cells “cleanse” the wound, clearing it of debris. The PMNs attain their maximal numbers in 24-48 hours and commence their departure by hour 72. As the process continues, monocytes also exude from the vessels. These are termed macrophages. The macrophages continue the cleansing process and manufacture various growth factors during days 3-4. Many factors influencing the wound healing process are secreted by macrophages. Sequence of events in healing Third phase – Proliferation This phase consists of different subphases. Fibroplasia Matrix deposition Angiogenesis Reepithelialization During days 5-7, fibroblasts have migrated into the wound, laying down new collagen. The wound is suffused with GAGs and fibronectin that are bonded to a protein core and contribute to matrix deposition. Angiogenesis is the product of parent vessel offshoots. The formation of new vasculature requires extracellular matrix and basement membrane degradation followed by migration, mitosis, and maturation of endothelial cells. Re-epithelization occurs with the migration of cells from the periphery of the wound and adnexal structures. This process commences with the spreading of cells within 24 hours. Division of peripheral cells occurs in hours 48-72, resulting in a thin epithelial cell layer, which bridges the wound. This succession of subphases can last up to 4 weeks in the clean and uncontaminated wound. Sequence of events in healing Fourth phase - Remodeling After the third week, the wound undergoes constant alterations, known as remodeling. This can last for years after the initial injury occurred. Collagen is degraded and deposited in an equilibrium-producing fashion. The collagen deposition in normal wound healing reaches a peak by the third week after the wound is created. Contraction of the wound is an ongoing process resulting in part from the proliferation of the specialized fibroblasts termed myofibroblasts, which resemble contractile smooth muscle cells. Stages of wound healing Resolution/ Remodeling Vessel regression, Collagen remodeling Proliferation Reepithelialization, Angiogenesis, Fibrogenesis, Inflammation PMNs, Macrophages, Lymphocytes Hemostasis Fibrin clot, platelet deposition 1D 3D 1wk Time after injury 6wk 8wk Types of healing Primary vs. secondary healing Complications of the healing process This process can go wrong and produce an increase of fibroblastic proliferation with a resultant hypertrophic scar Further exuberance can result in keloid formation where scar production extends beyond the area of the original insult. Conversely, insufficient healing can result in atrophic scar formation. Hypertrophic scar Keloid Complications of the healing process Weak scar: this may lead to hernia Cicatrisation: contracture of the size of the scar Implantation epidermoid cyst Stump neuroma: following amputation causing a painful coiled mass of nerves Sinus: is a track of septic granulation tissue connecting a cavity to the outside and has one blind end, e.g. pilonidal sinus Fistula: is a tract of septic granulation tissue connecting 2 epithelial surfaces Infection : leading to delayed healing Rarely scars may develop squamous cell carcinoma Ulcers: discontinuity of cover epithelium or muscle membrane Anal fistula Bone Bone is a dynamic tissue Osteoblasts Osteocytes Osteoclasts Osteogenic cells Bone anatomy Diaphysis Metaphysis Epiphysis – Prox/Dist Epiphyseal line Periosteum Compact cortical bone Spongy bone Articular Cartilage Medullary cavity Marrow Nutrient artery The histologic types Compact bone Trabecular bone Lamellar bone Woven bone Callus The matrix of bone Contains inorganic salt Calcium Hydroxyapatite in collagen framework. Osteoblasts - Calcification Mineralization Minerals hardness Collagen fibres Tensile strength. Collagen is necessary for Calcification. Fractures Break in the bone Simple / Compound – infection Single - Horizontal, oblique, spiral, Comminuted – multiple Greenstick – partial children Torus (buckle) – compression of cortex – children Types of fractures Compound fracture Bone remodeling Healing in bone Day 1 - Hematoma formation (fibrin mesh) Day 3 - Inflammation Week 1 - Soft callus – granulation, matrix Week 3-6 - Callus – ossification, woven bone Week 8+ - Re-modeling – absorb/deposit, strengthen, lamellate Healing in bone Healing in bone Healing in bone Healing in bone Healing in bone Callus formation Following mid-shaft humeral fracture Factors affecting healing Systemic & local factors Immobilization Improper reduction – abnormal position Infection: debris & dead tissue in wound Joint involvement Complications Delayed healing Non healing Joint involvement - ankylosis Abnormal position – arthritis Bone necrosis – nutrient artery Avascular necrosis Involucrum formation Pseudarthrosis Involucrum