"We Can Do Better Together" - Partnerships for Low
advertisement

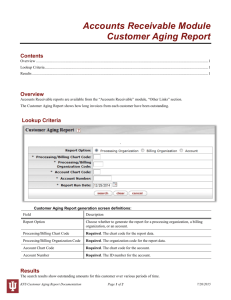
“We Can Do Better Together” Partnerships for Low-Income Health, Housing, and Social Support Services: Livable Communities for All Ages Fellowship Project Conducted in Partnership with: Department of Health & Human Services, Administration for Community Living, Health Resources and Services Administration, and Department of Housing and Urban Development Lori Simon-Rusinowitz, MPH, PhD 2014-15 Health and Aging Policy Fellow University of Maryland School of Public Health September 10, 2015 Health, Housing, and Social Support Services 1 Project Mentors and Planning Team Members: • HHS Administration for Community Living: Bob Hornyak, Elena Fazio, Lan Marshall • HHS Health Resources and Services Administration: Suma Nair, Jacqueline Rodrigue, Kent Forde, Shafa Al-Showk • Department of Housing and Urban Development Jennifer Ho, Ron Ashford, Leigh van Rij Health, Housing, and Social Support Services 2 Agenda • • • • Background Information Project Goals and Approach Webinar Description Comprehensive Agenda to Encourage more Successful Partnerships • References Health, Housing, and Social Support Services 3 Why Increased Interest in “Livable Communities” Now? • U.S. Trends in Aging Demographic and economic imperatives. Increased recognition about the importance of and demands on family caregivers, the backbone of our long-term services and supports (LTSS) system. Health, Housing, and Social Support Services 4 U.S. Trends in Aging • In 2013 there were 44.7 million Americans age 65 and older representing 14.1% of the U.S. population. By 2040, the number of older Americans is expected to grow to 82.3 million or about 21.7% of the U.S. population (Administration on Aging, 2014). • An estimated 70% of people who turn 65 will require long-term services and supports (LTSS) in their lives (e.g., personal care, medication management, care coordination, household tasks, transportation, etc.) (DHHS 2015). • • Source: www.census.gov/population/www/projections/summarytables.html Source: http://longtermcare.gov/the-basics/who-needs-care/ Health, Housing, and Social Support Services 5 U.S. Trends in Aging • In 2013, about 40 million family caregivers in the U.S. provided an estimated 37 billion hours of care to an adult with limitations in daily activities. The estimated economic value of their unpaid contributions was approximately $470 billion in 2013, up from an estimated $450 billion in 2009 (Reinhard et al. 2015). • Older adults prefer to receive LTSS in their own home and community, as opposed to institutional settings (e.g., nursing homes). – 88% prefer to remain in their current residence for as long as possible (Keenan 2010) – 92% prefer to remain in their local community for as long as possible (Keenan 2010) • • Source: http://assets.aarp.org/rgcenter/general/home-community-services-10.pdf Source: http://www.aarp.org/content/dam/aarp/ppi/2015/valuing-the-invaluable-2015-update-new.pdf Health, Housing, and Social Support Services 6 What is a “Livable Community”? • Multiple terms: Housing Plus Services, Livable Community, Livable Communities for All Ages, Communities for a Lifetime, Age-Friendly Community, Dementia Friendly Community World Health Organization (WHO, 2007) framework for a broad set of services that supports people aging in their own community rather than an institutional setting. Health, Housing, and Social Support Services 7 World Health Organization Framework (WHO, 2007) Transportation Outdoor Spaces & Buildings Community Support & Health Services Housing Age-friendly city Communication & Information Social Participation Respect & Social Inclusion Civic Participation & Employment World Health Organization (Ed.). (2007). Global age-friendly cities: A guide. World Health Organization. Retrieved from http://whqlibdoc.who.int/publications/2007/9789241547307_eng.pdf?ua=1 Health, Housing, and Social Support Services 8 Why Increased Interest in “Livable Communities” Now? Health Care Reform is Changing the Policy Landscape • Affordable Care Act policies and incentives (i.e. value-based payment and population health) are changing health care providers’ priorities and behavior. • To achieve the “triple aim” of better care for individuals, better care for populations, and lower per capita costs, providers need to keep people healthy and out of hospitals (IHI, 2015). • Health care providers can benefit from partnerships with affordable housing and social support programs to help meet these goals (LeadingAge, 2014). • • Institute for Healthcare Improvement (IHI). IHI Triple Aim Initiative. http://www.ihi.org/engage/initiatives/tripleaim/pages/default.aspx . Accessed August 29, 2015. LeadingAge Center for Housing Plus Services (2014) Housing and Health Care : Partners in Healthy Aging. http://www.leadingage.org/housinghealth/ Accessed August 29, 2015. Health, Housing, and Social Support Services 9 Benefits of Affordable Housing, Social Support, and Health Care Partnerships • Health care and affordable housing partnerships can offer residents: – easy access to health care services and programs (important for high service users), – health education programs and follow up care in a cost-effective setting, – health care providers who have an improved understanding of social factors effecting health conditions, – a service coordinator who knows residents and can follow up when needed. • LeadingAge Center for Housing Plus Services (2014) Housing and Health Care : Partners in Healthy Aging. http://www.leadingage.org/housinghealth/ Accessed August 29, 2015. Health, Housing, and Social Support Services 10 Partnerships for Low-Income Health, Housing, and Social Support Services Can Increase Access to Health Care • Housing Plus Services can help address the following health care challenges: - avoid unnecessary hospital re-admissions, address medication complications, manage chronic health, conduct patient education and encourage patient engagement, address social determinants of health, address “super utilizers,” and link older residents to social support services via local Aging & Disability Resource Centers and Area Agencies on Aging (e.g., case management, personal care, transportation, homemaker services). LeadingAge Center for Housing Plus Services (2014) Housing and Health Care : Partners in Healthy Aging. http://www.leadingage.org/housinghealth/ Accessed August 29, 2015. Health, Housing, and Social Support Services 11 Health and Housing Partnership: Public Housing Primary Care Program • HRSA operates Federally Qualified Health Centers (FQHC), the primary care, safety net health system for low income, vulnerable populations. • These health centers offer comprehensive primary care for all ages. • HRSA funds approximately 80 Public Housing Primary Care Centers that are either located in a public housing building or within one mile. • This program serves about 22 million patients; however, only 7% are over 65 years old (about 1.5 million patients). • FQHC Opportunity: Health centers can expand their capacity to serve the growing elderly population. • US HHS Heath Resources and Services Administration, Bureau of Primary Care, Public Housing and Primary Care Health Centers. http://bphc.hrsa.gov/qualityimprovement/supportnetworks/specialpopulations/. Accessed August 29, 2015. Health, Housing, and Social Support Services 12 Social Service Community Partnerships: “No Wrong Door” Approach to Services • ACL Goal: A LTSS system that is consumer-driven and cost-effective. • Steps: – – – – • Outreach and coordination with referral community services Person-centered counseling (focus on the person’s goals) Streamline eligibility to public programs State agency support: must include governor, Medicaid agency, consumers, key stakeholders in service design and oversight Administration for Community Living (2015), Center for Integrated Programs, Office of Consumer Access and Self-Determination, Aging & Disability Resources Centers, Program, No Wrong Door System, http://www.acl.gov/Programs/CIP/OCASD/ADRC/index.aspx. Accessed August 29, 2015. Health, Housing, and Social Support Services 13 “No Wrong Door” System Organizations 14 Health, Housing, and Social Support Services 14 Why Focus on Interagency Partnerships? • A Government Accountability Office Report (May 2015), entitled, Older Adults. Federal Strategy Needed to Help Ensure Efficient and Effective Delivery of Home and CommunityBased Services (HCBS), calls for the Administration for Community Living to lead collaborations between: – Departments of Housing and Urban Development, – Transportation, – and Agriculture, – as well as the Centers for Medicare and Medicaid Services, to meet the growing needs of elders for social support services. • With limited resources and growing needs, partnerships can leverage existing programs to better serve this population. • This report focused on non-medical services; it did not address primary care offered by FQHCs. However, social support services are essential to the successful outcomes of primary health services. • Federal interagency partnerships require time and attention. Each agency has its own priorities, and culture. Successful partnerships bridge these differences. Health, Housing, and Social Support Services 15 Agenda • • • • Background Information Project Goals and Approach Webinar Description Comprehensive Agenda to Encourage More Successful Partnerships • References Health, Housing, and Social Support Services 16 Project Goals: Obtain Maximum Program Benefits for Consumers via Interagency Partnerships, Encourage More Partnerships Social Support Services Housing Services Health, Housing, and Social Support Services Health Services 17 Project Approach • Identify existing health, housing, and social support partnerships, and program characteristics that make them successful or create barriers to success. • Highlight exemplary programs in a webinar designed to teach us about successful partnerships. Invite policymakers, providers, researchers, and others. • Identify ways to share lessons from the “early innovators” with the wider health, housing, and social support communities. • Develop a comprehensive agenda to encourage more successful partnerships. Health, Housing, and Social Support Services 18 Key Project Steps • Propose project to leaders in each agency, and obtain their support. • Agency leaders identify interagency team members. • Review literature and conduct background discussions with health, housing, and social support stakeholders to inform the webinar. • Identify successful partnerships to highlight. • Identify appropriate webinar audience members. • Conduct webinar with audience polling questions. • Develop a comprehensive agenda with recommendations. Health, Housing, and Social Support Services 19 National Initiatives Indicate Growing Interest in Livable Communities • AARP Livability Index (2015) • National Association of Area Agencies on Aging (2015). “Making Your Community Livable for All Ages” • Grantmakers in Aging: Improving America for All Ages (2013) • AARP’s network of age-friendly communities (2012) • LeadingAge “Housing Plus Services” Center, Learning Collaborative (2012) Health, Housing, and Social Support Services 20 National Initiatives Indicate Growing Interest in Livable Communities • National Center for Health in Public Housing: 2015 national symposium includes a plenary session and workshops on healthy aging in public housing. • Association of State and Territorial Health Officers, 2015 Annual Meeting showcases effective healthy aging programs, Association has a position statement on healthy aging in community settings. • Altarum Institute (2015) “MediCaring Communities,” financing model for community support services. • US HHS Assistant Secretary for Planning and Evaluation (2014a), evaluation of Support And Services at Home (SASH), a Vermont statewide housing, health, and social support program. Health, Housing, and Social Support Services 21 Current Literature Indicates Growing Interest in Livable Communities • Public Policy and Aging Report (2015). Making a home in the city: The age-friendly community movement. • The Gerontologist (2015): Toward the 2015 White House Conference on Aging: Creating an aging policy vision for the decade ahead, addresses “age-friendly communities.” • LeadingAge (2014): Combined HUD and Medicare database documents higher health costs among HUD-assisted elders. • Generations (2013-14): issue on “age-friendly communities.” • Journal of Aging and Social Policy (2014), two-volume issue on “age-friendly communities.” Health, Housing, and Social Support Services 22 Agenda • • • • Background Information Project Goals and Approach Webinar Description Comprehensive Agenda to Encourage More Successful Partnerships • References Health, Housing, and Social Support Services 23 Webinar Description • • • • Webinar Overview and Introductions We Need to Learn From You: Audience Polling Question What Does Research Tell Us About “Housing Plus Services”? Learning from Partnerships in Vermont, California, and Hawaii • We Need to Learn From You: Audience Polling Questions • Audience Discussion Health, Housing, and Social Support Services 24 Webinar Audience Members • Planning team members invited key stakeholders from their own health, housing, and social service networks. • We aimed for 50 key stakeholders. • Over 100 people registered for the seminar, and included people from: - eight federal agencies or offices, - national associations/technical assistance providers. - direct service providers, - foundations, and - researchers. Health, Housing, and Social Support Services 25 Bob Hornyak Director, Office of Performance and Evaluation and Lori Gerhard Director, Office of Integrated Programs HHS ACL Health, Housing, and Social Support Services 26 Suma Nair Director of the Office of Quality Improvement Health Resources and Services Administration’s Bureau of Primary Health Care Health, Housing, and Social Support Services 27 Jennifer Ho Senior Advisor on Housing and Services U.S. Department of Housing and Urban Development Health, Housing, and Social Support Services 28 Robyn Stone Executive Director, Center for Applied Research, LeadingAge Health, Housing, and Social Support Services 29 Building the Evidence Base for Affordable Senior Housing + Services Robyn I. Stone, DrPH Executive Director, Center for Applied Research, LeadingAge July 29, 2015 Health, Housing, and Social Support Services 30 “A Picture of Housing & Health” Researchers compared Medicare and Medicaid cost and utilization for HUD-assisted Medicare beneficiaries and unassisted beneficiaries in the community. They found that HUD residents: – included a much larger percentage of people who are dually eligible for Medicare and Medicaid than people who do not receive HUD assistance, and – have more serious health conditions, use more Medicare and Medicaid services, and have greater health care costs than those outside of HUD assisted programs. Stone, R., (2015). Building the evidence base for affordable senior housing + services. Presented during the webinar, entitled Partnerships for Health, Housing, and Social Support Services: Livable Communities for All Ages, July 29. Health, Housing, and Social Support Services 31 How Housing and Services Matter Two data sources help illustrate outcomes: – Researchers surveyed 2,017 HUD properties in the HUD/Medicare-Medicaid data set, and reviewed services available and health outcomes. – They also studied three “housing plus services” programs: • Vermont: Support And Services at Home (SASH) • Pittsburgh, PA: Staying at Home Program • Harrisburg, PA: Presbyterian Senior Living & PinnacleHealth Partnership Health, Housing, and Social Support Services 32 How Housing and Services Matter Sample Findings Indicate Positive Outcomes: HUD/CMS Survey: The availability of HUD building services were associated with several positive resident health outcomes. Support And Services at Home (SASH): Early findings over two years indicated that growth in annual total Medicare expenditures was $1,756 - $2,197 lower for SASH participants in well-established panels than for two comparison groups. Staying at Home: Participants were less likely to visit the ER, have unscheduled hospital stays, report negative health conditions, and move to a nursing home. Presbyterian Senior Living & PinnacleHealth: Over a two-year period, partnership participants had fewer ER visits and inpatient visits. Health, Housing, and Social Support Services 33 Molly Dugan Director Support And Services at Home (SASH), Vermont Health, Housing, and Social Support Services 34 The Intersection of Health & Housing • SASH – Statewide, part of Vermont’s Health Care Reform Initiative • Housing as a platform for health care • 65 partner agencies part of SASH Collaboratives • Available in all types of HUD housing Health, Housing, and Social Support Services 35 The SASH Model Focuses on Three Components of Care Management • Conducts wellness assessment • Convenes SASH team • Understands participants needs and preferences • Coordinates individual/community healthy living plans Care Coordination • Develops healthy living plan • Coaches SASH Participants • Provides reminders and in person check ins • Organizes presentations and evidence based programs Self Management • Coordinates with discharge staff, family and neighbors • Personal visit to review discharge instructions • Helps ensure a safe home transition Transitional Care Health, Housing, and Social Support Services 36 Primary Challenges • • • • • • Sustainable funding source Lack of administrative funding Keeping housing at the “table.” Information sharing – IT systems, HIPAA Capacity for mental/behavioral health services Multiple funding sources=multiple applications, reports, outcomes, etc. Health, Housing, and Social Support Services 37 Success Drivers • Housing sector included in statewide health care reform discussions/initiative • Population-based approach with focus on social determinants of health • Medicare Demonstration funds allow flexible spending to match need – capitated model • SASH designed with participants not for them • Real-time data and ability to regularly share outcomes • Statewide platform to build upon Health, Housing, and Social Support Services 38 Marty Lynch CEO and Brenda Goldstein Psychosocial Services Director LifeLong Medical Care, California Health, Housing, and Social Support Services Services located in Oakland, Berkeley, West Contra Costa County 48,000 patients served annually 12 Primary Care Clinics, Urgent Care, Adult Day Health, Supportive Housing, School-Based Clinics, Dental Special history with elders and care for complex adult populations including disabled and homeless Health, Housing, and Social Support Services 40 City/County Government Behavioral Health Housing Departments Public Health Hospitals Managed Care Plans Center for Independent Living Health Care for the Homeless Housing Developers Community Based Organizations Health, Housing, and Social Support Services 41 California has decentralized health care delivery systems – delegated from state to local managed care plans Housing availability and cost Fee for service billing and unaligned financial incentives Health, Housing, and Social Support Services 42 Funding case management by non-licensed providers Fragmented & diagnosis driven funding Blended funding = multiple reporting/documentation requirements Productivity concerns – longer appointments needed for complex populations which include family members, support teams etc. Need to demonstrate cost savings Health, Housing, and Social Support Services 43 Unlinked, multiple IT systems creates challenges Identifying target populations Tracking patient utilization Assessing outcomes across the system of care Staff recruitment/retention Aging homeless population – needs exceed access to in home services or appropriate institutional based care Health, Housing, and Social Support Services 44 Medicaid eligibility expansion Improved coverage of mental health services Integration of primary/behavioral health care Managed care plans focus on high cost members Recognition of impact of social determinants of health (especially housing) Increased need for medical respite care given focus on reducing hospitalizations Health, Housing, and Social Support Services 45 Merlita Compton Director, Elder Services And Laura Taylor Grant Writer Kokua Kalihi Valley, Hawaii Health, Housing, and Social Support Services 46 Addressing the social determinants of health among the multi-ethnic elders of Kalihi. July 29, 2015 Merlita Compton Laura Taylor Health, Housing, and Social Support Services 47 Patient Demographics, 2014 8% 10.5% of KKV’s patients are 65 or older 1% 0-100% of poverty level 35% 91% 30% 101-200% of poverty level over 200% of poverty level 25% 20% 15% 17% 5% 18% 10% Medicaid/Quest Private Insurance 5% 0% Uninsured 60% Medicare 30% of KKV’s patients live in public housing Health, Housing, and Social Support Services 48 Elder Care Program History # of clients 734 800 600 400 200 0 12 24 45 80 1999 2001 2002 2003 Elder Services Established with Case Management Health Maintenance, Senior Volunteers Caregiver Support & Transportation Health, Housing, and Social Support Services 120 2005 539 571 2011 2013 226 2007 MD, BH, nutrition ed, eligibility services Dental & CDSMP 2014 Personal Care, Gardening MD clinic expands 49 Key Partnerships Hawaii Department of Health, Executive Office on Aging Honolulu C&C, Elderly Affairs Division (Area Agency on Aging) Public Housing communities University of Hawai‘i Law School School of Medicine Dept of Public Health… eval School of Nursing Office of Public Health Studies Health, Housing, and Social Support Services 50 KKV Elder Care Goals Assist Kalihi’s kupuna to maintain: Highest level of physical/mental abilities Highest quality of life Save medical costs Prevent or delay institutionalization Reduce premature death Improve quality of life Reduce the risk of falling Improve health Promote mental well-being Delay onset of disability Empower elders to live independently and remain in their community Health, Housing, and Social Support Services Nana Perpetua Amian, 101 years old 51 Funding partnerships, challenges in a changing landscape City 22% Private 12% 66% KKV Elder Care Funding Sources Health, Housing, and Social Support Services 52 Agenda • • • • Background Information Project Goals and Approach Webinar Description Comprehensive Agenda to Encourage More Successful Partnerships • References Health, Housing, and Social Support Services 53 Comprehensive Agenda: Process • Establish an ongoing interagency workgroup that leaders from each agency can support with adequate time and resources. • Include Department of Transportation and CMS team members as transportation and financing are key components of livable communities for all ages. • Develop intentional steps to create an interagency workgroup. Each agency needs to understand each others’ mission, priorities, and culture. • Build on existing knowledge – research, evidence-based interventions, best practices, and discussions with key stakeholders. Health, Housing, and Social Support Services 54 Comprehensive Agenda: Content • Address workforce issues, including shortages among direct care workers, geriatricians, and other providers. • Work with the newly funded HRSA Geriatrics Workforce Enhancement Program (GWEP) to address workforce issues (e.g., develop guidelines to expand FQHCs’ capacity to serve elders and adults with disabilities). • Develop guidelines to address issues such as: – hiring and retaining geriatricians and other geriatric providers, – training for primary care providers who see elders and adults with disabilities, – developing approaches to address multiple chronic conditions, and – providing adequate time for complex consumers. Health, Housing, and Social Support Services 55 Comprehensive Agenda: Content (continued) • Address the need for oral health services, physical therapy, occupational therapy, and other services that support the chronic care needs of elders and adults with disabilities. • Incorporate technology that can help support consumers, direct care workers, and family caregivers. Technology would need to include financing and training. • Build on quality indicators/benchmarks for each service area (health, housing, social support services), and benchmarks for integrated services (e.g., continuity of services, communication among providers, level of consumer-direction infused into services). • Facilitate states’ efforts to offer individual budget community-based service programs if they choose to do so. This evidence-based consumer-directed option offers maximum flexibility to consumers and their families in purchasing services and hiring direct care workers. Health, Housing, and Social Support Services 56 Comprehensive Agenda: Research • Develop an ongoing literature review from health, housing, and social support partnerships (including seminal work informing current literature). Update the literature review regularly to include evolving literature. • Identify gaps in knowledge related to a low-income, diverse older populations and adults with disabilities. • Develop a research agenda, including suggested questions to address in a demonstration and evaluation of evidence-based “housing plus services” programs (e.g., implementation with diverse populations and in diverse geographic areas). • Develop and test messages designed to encourage partnerships among health, housing, and social support services (e.g., we can do better by working together; the outcome is worth the effort). Health, Housing, and Social Support Services 57 Comprehensive Agenda: Policy and Implementation Challenges • Lack of targeted, sustainable funding for health, housing, and social support partnerships (e.g., funding for administrative functions). • Need for streamlined funding sources to address duplication from multiple funders (e.g., multiple applications and reports). • Data sharing barriers due to privacy concerns/HIPAA and information technology incompatibilities. • Barriers to funding diverse types of case managers, including those who may be competent but unlicensed. Health, Housing, and Social Support Services 58 References • • • • • • • • • • • • • • AARP (2015) Livability Index. http://livabilityindex.aarp.org/ Accessed August 29, 2015. AARP (2012). AARP’s network of age-friendly communities. Washington, DC. Retrieved on August 20, 2012 from http://www.aarpinternational.org/File%20Library/Resources/AARPNetworkofAgeFriendlyCommunitiesBooklet.pdf Administration for Community Living (2015), Center for Integrated Programs, Office of Consumer Access and Self-Determination, Aging & Disability Resources Centers, Program, No Wrong Door System, http://www.acl.gov/Programs/CIP/OCASD/ADRC/index.aspx. Accessed August 29, 2015. Administration on Aging (2014). A Profile of Older Americans. http://www.aoa.acl.gov/Aging_Statistics/Profile/index.aspx Accessed August 29, 2015. Castle, N., & Resnick, N. (2014). Service-enriched housing: The staying at home program. Journal of Applied Gerontology, 0733464814540049. Altarum Institute (2015) Center for Elder Care and Advanced Illness. MediCaring communities. A call to action: Making it safe to grow old. http://altarum.org/sites/default/files/uploaded-related-files/MedicaringCommunities_042815.pdf Accessed August 29, 2015. Association of State and Territorial Health Officers, Health aging and public health position statement. http://www.astho.org/Policyand-Position-Statements/Healthy-Aging-and-Public-Health-Position-Statement/ Ellenbecker, C. H., Byrne, K., O’Brien, E., and Rogosta, C. (2002). Nursing Clinics in Elder Housing: Providing Access and Improving Health Care Outcomes. Journal of Community Health Nursing, 19: 7–15. Generations, Vol. 37, No. 4. Winter 2013–2014. Aging in Community. Golant, S. M., Pynoos, J., Cicero, C., Lawler, K., Berger, C., & Blechman, A. D. (2012). Livable and Sustainable Communities. Public Policy and Aging Report, 19(1). Golant, S. M., Parsons, P., & Boling, P. A. (2010). Assessing the quality of care found in affordable clustered housing-care arrangements: Key to informing public policy. Cityscape, 5-28. Grantmakers in Aging (2013). Age-friendly communities. The movement to create great places to grow up and grow old in America. Retrieved on April 12, 2014 from http://www.giaging.org/documents/130402_GIA_AFC_Primer.pdf Institute for Healthcare Improvement (IHI). IHI Triple Aim Initiative. http://www.ihi.org/engage/initiatives/tripleaim/pages/default.aspx . Accessed August 29, 2015. Journal of Aging & Social Policy (2014). Special Issue: Age-friendly cities and communities around the world. Vol. 26, Issue 1-2. Health, Housing, and Social Support Services 59 References • • • • • • • • • • • Keenan, T. A. Home and community preferences of the 45+ population. (Washington, D.C.: AARP, 2010), 4. Available at: http://assets.aarp.org/rgcenter/general/home-community-services-10.pdf LeadingAge Center for Housing Plus Services (2014). Study documents higher health costs among HUD-assisted seniors. http://www.leadingage.org/Study_Documents_Higher_Health_Costs_Among_HUD_Assisted_Seniors.aspx Accessed August 29, 2015. LeadingAge Center for Housing Plus Services (2014) Housing and Health Care : Partners in Healthy Aging. http://www.leadingage.org/housinghealth/. Accessed August 29, 2015. LeadingAge Center for Housing Plus Services (2012). Why housing plus services. Retrieved on March 23, 2014 from http://www.leadingage.org/Housing_Plus_Services_Rationale.aspx Mollica, R., and Morris, M. 2005. Massachusetts Supportive Housing Program. New Brunswick, NJ: Rutgers Center for State Health Policy. National Association of Area Agencies on Aging, “Making your community livable for all ages: What’s working!” (2015). http://www.n4a.org/files/n4aMakingYourCommunityLivable1.pdf National Center for Health in Public Housing (2015), Health Center and Public Housing National Symposium, http://www.nchph.org/wp-content/uploads/2015/07/2015-Health-Center-and-Public-Housing-Plenary-Descriptions.pdf Public Policy and Aging Report (2015). Making a home in the city: The age-friendly community movement. Vol. 25 (1) Winter. Rabins, P. V., Black, B.S., Roca, R., German, P.S., McGuire, M., Robbins, B., Rye, R., and Brant, L. (2000). Effectiveness of a nursebased outreach program for identifying and treating psychiatric Illness in the elderly. Journal of the American Medical Association, 283: 2802–2809. Reinhard, S., Feinberg, L. F., Choula, R., and Houser, A. (2015). Valuing the invaluable: 2015 update. AARP Public Policy Institute, Washington, D.C. Source: http://www.aarp.org/content/dam/aarp/ppi/2015/valuing-the-invaluable-2015-update-new.pdf Robbins, B., Rye, R., German, P.S., Tlasek-Wolfson, M., Penrod, J., Rabins, P. V., Black, B.S.. (2000). The Psychogeriatric Assessment and Treatment in City Housing (PATCH) Program for elders with mental illness in public housing: Getting through the crack in the door. Archives of Psychiatric Nursing, 14: 163–172. Health, Housing, and Social Support Services 60 References • • • • • • • • • • Siu, C. (2009). Impacts of nutrition and human services interventions on the health of elderly and disabled persons in public housing. Washington, DC: Congressional Hunger Center. The Gerontologist (2015). Toward the 2015 White House Conference on Aging: Creating an aging policy vision for the decade ahead. Vol. 55(2), 179-182. U.S. Census Bureau. (2010). U.S. Population Projections. Available at: www.census.gov/population/www/projections/summarytables.html U.S. Census Bureau. (2013). American Community Survey. Retrieved from http://www.census.gov/acs/www/ U.S. Department of Health and Human Services (2014). Picture of housing and health: Medicare and Medicaid use among older adults in HUD-assisted housing. Available at: http://aspe.hhs.gov/basic-report/picture-housing-and-health-medicare-andmedicaid-use-among-older-adults-hud-assisted-housing U.S. Department of Health and Human Services (2014a). Support And Services at Home (SASH) evaluation: first annual report. Retrieved from http://aspe.hhs.gov/daltcp/reports/2014/sash1.pdf U.S. Department of Health and Human Services. (2015). Who needs care? Available at: http://longtermcare.gov/the-basics/who-needs-care/ US Department of Health and Human Services, Heath Resources and Services Administration, Bureau of Primary Care, Public Housing and Primary Care Health Centers. http://bphc.hrsa.gov/qualityimprovement/supportnetworks/specialpopulations/ Accessed August 29, 2015. U.S. Government Accountability Office. (2015). Older adults: Federal strategy needed to help ensure efficient and effective delivery of home and community-based services and supports. Available at: http://www.gao.gov/products/GAO-15-190 World Health Organization (WHO) (2007). Global age-friendly cities: A guide. Geneva, Switzerland. Retrieved August 16, 2012 from http://whqlibdoc.who.int/publications/2007/9789241547307_eng.pdf Health, Housing, and Social Support Services 61 For additional information about today’s webinar, please contact: Lori Simon-Rusinowitz email: lasr@umd.edu Health, Housing, and Social Support Services 62