Treatment
advertisement
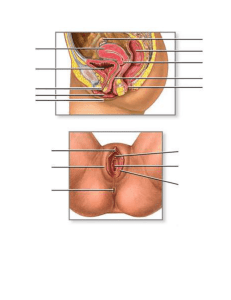
Chapter 16 The reproductive system Physiologic Concepts Spermatogenesis Spermatogenesis (the formation of sperm) begins during puberty and continues throughout the lifetime of a male. Spermatogenesis requires approximately 2 months. From each primary spermatocyte, four viable sperm are produced. Spermatogenesis occurs in the seminiferous tubule under the control of two pituitary hormones: ◦ follicle-stimulating hormone (FSH) and ◦ luteinizing hormone (LH) and the sex hormones, primarily testosterone. Testes Follicle-Stimulating Hormone ◦ FSH is a hormone released from the anterior pituitary in response to gonadotropin-releasing hormone (GnRH) . ◦ The final effect of FSH is to cause proliferation and differentiation of the immature sperm. Luteinizing Hormone ◦ LH is the 2nd hormone released in response to stimulation by GnRH. ◦ LH stimulates the synthesis of the steroid hormone testosterone. Stimuli Controlling GnRH Release GnRH is released in small pulses throughout the day, resulting in relatively constant daily levels. Increases or decreases in GnRH release may occur seasonally and with different physical and psychological conditions such as anxiety or depression. Changes in the secretion of GnRH may affect sperm formation by affecting LH and FSH and may alter libido. The Menstrual Cycle It is the cyclic maturation and release of an ovum. It involves the growth of a follicle, ovulation of the ovum, and characteristic changes in the endometrial lining of the uterus. Ovulation On approximately day 12 of the menstrual cycle, there is a dramatic rise (6- to 10-fold) in the release of LH from the anterior pituitary. This rise is called a preovulatory LH surge. FSH increases to a lesser degree. Rising LH levels initiate a profound, final growth of the follicle, and then rupture, releasing the ovum into the abdominal cavity. Phases of Menstrual cycle Hormonal changes during menstrual cycle. Female Secondary Sexual Characteristics They are under the control of estrogen and to a lesser extent progesterone. The female secondary sexual characteristics include: ◦ Fully developed breasts. ◦ The female pattern distribution of pubic hair. ◦ Bone growth and closure of the epiphyseal plates. Puberty Puberty is the beginning of sexual maturation. Puberty typically occurs at a younger age in girls (8 and 14) than boys (10 and 16) years of age. The menstrual cycle is the peak of puberty in girls. In boys, puberty culminates in the ability to ejaculate mature sperm. Menopause Menopause is as a lack of menstrual cycles for the previous 12 months. It occurs in a woman when her ovaries no longer respond to LH and FSH with estrogen and progesterone production, and no longer release an ovum Pathophysiologic Concepts Infertility Infertility is the inability or reduced ability to produce offspring. Infertility in a couple may result from female factors (40 to 50%), male factors (30 to 40%), or both (20%). Infertility may occur from the start of the relationship (primary infertility) or after the couple has already produced one or more offspring (secondary infertility). Female Factors Female factors include: problems with follicular growth, anovulation (failure to ovulate), or ovulatory irregularities. Optimal fertility in women lasts to about 30 years of age and then begins to fall sharply with increasing frequency as a woman ages. Blockage of the fallopian tubes following pelvic infection or the presence of uterine abnormalities that prevent implantation may be involved. Immune responses may destroy the implanted embryo if the woman is either hyperimmune to the embryo or fails to develop tolerance to it. Miscarriages later in gestation may occur if the placenta is poorly placed or poorly perfused with blood, or if the cervix cannot support the weight of a growing fetus. Treatment of female infertility Treatment is specific to the cause. Drugs to induce ovulation or superovulation may be administered. Harvesting of eggs from the woman for in vitro fertilization (outside of the body) may be attempted. Eggs fertilized outside the body may be implanted into the fallopian tube or uterus. Male Factors Male factors may include defects in spermatogenesis that result in: ◦ deformed sperm or ◦ sperm too few in number to allow for successful penetration of the ovum. Sperm motility (movement) may be impaired as well. Male Factors Causes: Infection and scarring of the testicles, epididymis, vas deferens, or urethra. Systemic infections, such as mumps, may cause swelling of the testicles and destruction of the seminiferous tubules. Obstruction of the blood vessels supplying the testes can cause hypoxia and a failure of the sperm to develop or survive. Autoantibodies produced against sperm may reduce sperm number and quality. Exposure of the testicles to high temperature may reduce spermatogenesis. Treatment of male factor infertility Treatment is specific to the cause. For example, for a man with a low sperm count, sperm may be obtained and then introduced artificially into his female partner after techniques to increase the concentration of the highest-quality sperm have been performed. This process is called artificial insemination. Pathophysiologic Concepts Gynecomastia Gynecomastia is the enlargement of breast tissue in males. It can result from excess production of estrogen in the male or the liver's inability to break down normal male estrogen secretions. It is frequently seen during early puberty in some males and may be a normal development or may be related to excess body weight or a hormonal imbalance. Pathophysiologic Dysmenorrhea Is painful menstruation that occurs without evidence of pelvic infection or disease. It is usually caused by excessive release of a specific prostaglandin (F2 alpha ), from the uterine endometrial cells. Which stimulates myometrial smooth muscle contraction and uterine blood vessel constriction. It worsens the uterine hypoxia normally associated with menstruation significant pain. NSAIDs (inhibit prostaglandin production) can effectively reduce cramping. Prostaglandin inhibitors should be used at the first sign of pain or at the first sign of menstrual flow. Because forceful menstrual cramping may contribute to the development of endometriosis (painful growth of uterine tissue outside of the uterus), Complaints of dysmenorrhea should always be taken seriously, and attempts should be made to reduce its incidence. Pathophysiologic Amenorrhea Is the absence of a menstrual cycle. It is considered: ◦ primary if a woman has never had a menstrual cycle or ◦ secondary if she has had menstrual cycles in the past, but no longer. Amenorrhea exists naturally before puberty (primary amenorrhea) and after menopause (secondary amenorrhea). It also occurs during pregnancy, for a few to several weeks after delivery of an infant, and may occur during lactation. Emotional disturbances and physical stress may also cause amenorrhea. Endocrine disorders, affecting ovaries, pituitary, thyroid, or adrenal glands, can cause amenorrhea, both primary and secondary. Conditions of Disease or Injury Cryptorchidism It is the failure of one or both testicles to descend into the scrotum of a male infant. Cryptorchidism is present at birth and is especially common in premature infants. Mostly the testes will descend on their own within the first year of birth. If not, the testes will remain at a higher temperature which may affect sperm quantity and quality, leading to infertility later in life. However, male sexual function and secondary sexual characteristics are normal. Cryptorchidism Clinical Manifestations One or both testes will not be palpable in the scrotum at birth. Diagnostic Tools Physical examination is used to diagnose the condition. Ultrasound or other imaging techniques may be used. Complications Infertility in the adult may result if descent does not occur. Increased risk of testicular cancer exists in individuals with cryptorchidism, even after surgical repair. Cryptorchidism Treatment Most cases of cryptorchidism will reverse spontaneously within 1 year. If not occur, treatment with hCG may stimulate descent. If hormonal therapy is ineffective, surgery is required. Surgery should be performed by 2 years of age. Varicocele An abnormal dilation of a vein in the spermatic cord. A sudden occurrence of a varicocele in older men may indicate an advanced renal tumor. Clinical Manifestations It may be asymptomatic or associated with a slight feeling of discomfort and testicular heaviness. Tortuous, dilated veins may be palpable. Diagnostic Tools Physical examination is used to diagnose the condition. Ultrasound may be used. Complications Poor blood flow to the testes may cause infertility. Treatment A support garment for the testicles is worn to relieve discomfort. To maintain fertility, surgical ligation of the vein may be performed. Hydrocele Is the collection of a plasma filtrate in the scrotum, outside the testes, that results in scrotal swelling and therefore testicular ischemia. A hydrocele may be: ◦ ◦ ◦ ◦ a congenital problem or Acquired; trauma to the genitals. A testicular tumor may cause formation of a hydrocele. Idiopathic development may also occur. Clinical Manifestations A hydrocele may be asymptomatic or associated with palpable or visible swelling and discomfort. Diagnostic Tools Physical examination, augmented by US. Visual inspection using a light focused on the testicle may be able to identify fluid. Treatment Identification of the cause and drainage of the fluid. Pelvic Inflammatory Disease PID is the infectious inflammation of any of the organs of the upper genital tract in women, including: uterus, fallopian tubes (salpingitis), or ovaries (oophoritis). The infectious agent is usually bacterial and is often acquired during sexual intercourse. A variety of MOs may include N. gonorrhoeae, C. trachomatis, and Escherichia coli. In severe cases, the entire peritoneal cavity may be affected. Clinical Manifestations Although occasionally a woman will be asymptomatic, she usually presents with a high fever and severe bilateral abdominal pain. Bleeding between periods may occur. Abdominal pain worsens with intercourse and physical activity. Pelvic Inflammatory Disease Diagnostic Tools Palpating or moving the cervix during an internal pelvic examination is very painful. Purulent discharge at the external os may be apparent on inspection. Culture of the cervical discharge may indicate the infecting microorganism. WBCs and ESR are usually elevated. Visualization of the inflamed pelvis by laparoscopy, the insertion of a fiberoptic probe, can be used to confirm the diagnosis of PID. Pelvic Inflammatory Disease Complications PID may lead to scarring and adhesions of the uterus or fallopian tubes, predisposing a woman to infertility; risk of a subsequent ectopic pregnancy. In an ectopic pregnancy, the embryo implants and grows at a site other than the uterus, usually the fallopian tube. Rupture of the fallopian tube may occur, leading to internal hemorrhage and maternal death. Approximately 5% to 10% of women with PID die, usually from septic shock. Pelvic Inflammatory Diseases Treatment AB therapy at home or in the hospital is required. Avoidance of sexual intercourse until the inflammation has subsided will allow healing to occur and will reduce the risk of repeated infection. Education on the use of barrier methods of contraception (condom, diaphragm with foam or jelly) to prevent future occurrences of sexually transmitted disease is important. Birth control pills may reduce PID by increasing the production of cervical mucus, but do not replace the need for a condom. The sexual partner(s) of an affected woman should be evaluated for infection and, if necessary, treated with antibiotics. Appendicitis must be ruled out as the cause of abdominal pain. Endometriosis Endometriosis is the presence of uterine endometrial cells outside the uterus, anywhere in the pelvic or abdominal region. The endometrial cells respond to estrogen and progesterone with proliferation, secretion, and bleeding during the menstrual cycle. This can cause inflammation and severe pain. The inflammation may lead to scarring of pelvic or abdominal organs and infertility Clinical Manifestations Menstrual cramping and pain, ranging from mild to severe, before and/or during menstruation is the most common symptom of endometriosis. Changes in bowel movements (diarrhea or constipation) may occur around the time of menstruation. Pain with intercourse (dyspareunia) or during defecation (if rectal tissue is involved). The pain is usually worse during menstruation, but in severe cases pain may be constant. Endometriosis Diagnostic Tools Visualization of the peritoneal cavity using laparoscopic techniques can diagnose endometriosis and assign a stage to the disease. Complications Infertility is a common (30% to 40%) complication of endometriosis. Endometriosis may cause infertility by causing scarring and obstruction of the fallopian tubes or by initiating a maintained state of inflammation. Hormonal disturbances may occur. Emotional distress, family and marital problems, especially if infertility is a concern. Cancer of the Female Reproductive Tract Cancer of the female reproductive tract may develop in the vagina, uterus, or ovaries. Vaginal Cancer usually occurring in women older than 60 years of age. ◦ The vaginal squamous cells are most often involved. ◦ Frequently, the cancer is a secondary metastasis. ◦ Uterine Cancer Uterine cancer includes cancer of the cervix and endometrium. Cervical cancer is often a result of STD of the cervix caused by certain strains of the human papillomavirus (HPV). Cervical cancer is most common in women who have had multiple sexual partners. The premalignant changes(dysplasia), can be identified and staged during cytologic studies of a cervical smear Cancer of the Female Reproductive Tract Uterine endometrial cancer is the most common female reproductive cancer and is usually an adenocarcinoma (from the epithelial cells). Endometrial cancer is related to lifetime exposure to estrogen and typically presents in postmenopausal women. Ovarian Cancer Although relatively rare, ovarian cancer causes death more often than any other female reproductive cancer. Clinical Manifestations be asymptomatic or associated with bleeding, discharge, or pain. Cervical cancer may be asymptomatic or associated with bleeding after intercourse or spotting between menstrual periods. A vaginal discharge with odor may be present. Endometrial cancer may be asymptomatic or associated with abnormal bleeding. Ovarian cancer is usually asymptomatic until the disease is advanced. Late symptoms include abdominal swelling and pain. Gastrointestinal obstruction may cause vomiting, constipation, or small-volume diarrhea. Vaginal cancer may Diagnostic Tools The Pap smear Direct cytologic sampling of the vagina and endometrium Ovarian cancer can be identified by use of MRI or vaginal ultrasound. The ovaries may be palpable. . Increased level of an ovarian tumor cell antigen, CA125, in a symptomatic woman or a woman with a family history of ovarian or breast cancer can be an early indication of disease. Complications Death may occur with any of the reproductive cancers. Survival rates are highest (75 to 95%) with endometrial cancer and lowest (25 to 30%) with ovarian cancer. Early detection can improve survival rate significantly, especially for cervical cancer, which has a survival rate near 100% if identified while still in situ (before it has spread).