幻灯片 1
advertisement

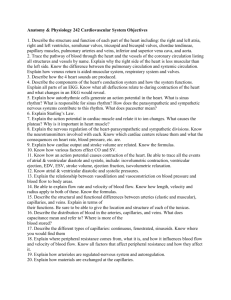
Cardiac Pump OBJECTIVES • Describe how the heart enable it to pump blood through the systemic and pulmonary circulations. • Discuss the pressure changes in the heart chambers and great vessels during a complete cardiac cycle. • List the factors that determine cardiac contractile force. • Explain how electrical excitation of the heart is coupled to its contractions. The Structures of the Heart is Designed for Optimal Function Several important morphological and functional differences exist between myocardial and skeletal muscle cells • A striking difference is that cardiac muscle appears to be a syncytium (a functional syncytium, not a true anatomical syncytium ) • with branching and interconnecting fibers, whereas skeletal muscle cells do not interconnect. Cardiac muscle functions as a syncytium because a wave of depolarization, followed by contractions of the atria and ventricles (an all-or-none response), occurs when a uprathreshold stimulus is applied. As the wave of excitation approaches the end of a cardiac cell, the spread of excitation to the next cell depends on the electrical conductance of the boundary between the two cells. Gap junctions (nexuses) with high conductance are present in the intercalated disks between adjacent cells. cardiac impulse from one cell to the next, are made up of connexons, • cardiac muscle is richly endowed with mitochondria (sarcosomes) which contain the respiratory enzymes necessary for oxidative phosphorylation. • To provide adequate O2 and substrate for its metabolic machinery, the myocardium is also endowed with a rich capillary supply, about one capillary per fiber. The cardiac chambers consist of two atria, two ventricles, and four valves The cardiac valves consist of thin flaps of tough, flexible, endothelium-covered fibrous tissue firmly attached at the base to the fibrous valve rings. Movements of the valve leaflets are essentially passive, and the orientation of the cardiac valves is responsible for the unidirectional flow of blood through the heart. Cardiac valves are interposed between atria and ventricle • Atrioventricular valves . The tricuspid valve lies between the right atrium and right ventricle and is made up of three cusps, The mitral valve lies between the left atrium and left ventricular and has two cusps. • Semilunar valves The valves between the right ventricle and pulmonary artery and between the left ventricle and aorta consist of three cuplike cusps attached to the valve rings. At the end of the reduced ejection phase of ventricular systole, blood flow reverses briefly toward the ventricles. This flow reversal snaps the cusps together and prevents regurgitation of blood into the ventricles. The pericardium is an epithelialized fibrous sac that invests the heart The pericardium consists of a visceral layer that is adherent to the epicardium and a parietal layer separated from the visceral layer by a thin layer of fluid. The fluid layer provides lubrication for the continuous movement of the enclosed heart. The pericardium is nor very distensible and thus strongly resists a large, rapid increase in cardiac size. Therefore the pericardium helps prevent sudden over distention of the heart chambers. The Cardiac Cycle is the Sequential Contraction and Relaxation of Atria and Ventricles Ventricular systole is initiated by Ventricular excitation (1) lsovolumic contraction • The interval between the start of ventricular systole and the opening of the semilunar valves is called isovolumic contraction because ventricular volume is constant during this brief period. • Ventricular pressure rises abruptly (2) Ejection rapid ejection: The rapid-ejection phase is characterized by the sharp rise in ventricular and aortic pressures that terminates at the peak ventricular and aortic pressures, an abrupt decrease in ventricular volume, and a large aortic blood flow. reduced ejection: During the reduced ejection period, runoff of blood from the aorta to the periphery exceeds ventricular output, so aortic and ventricular pressures decline. Throughout ventricular systole the blood returning to the atria progressively increases atrial pressure. At the end of ejection a volume of blood approximately equal to that ejected during systole remains in the ventricular cavities. This residual volume is fairly constant in normal hearts. However, it is smaller ? when heart rate increases or when outflow resistance is reduced, Ventricular filling occurs during diastole (1) Isovolumic relaxation The period between closure of the semilunar valves and opening of the AV valves is called isovolumic relaxation. It is characterized by a precipitous fall in ventricular pressure without a change in ventricular volume. (2) Rapid filling phase Ventricular filling occurs immediately after the AV valves open. The blood that had returned to the atria during the previous ventricular systole is abruptly released into the relaxing ventricles. The atrial and ventricular pressures decrease despite the increase in ventricular volume (3) Diastasis (slow filling) During diastasis, blood returning from the periphery flows into the right ventricle, and blood from the puhnunary circulation flows into the left ventricle. This small, slow addition to ventricular filling is indicated by gradual increases in atrial, ventricular, and venous pressures and in ventricular volume. (4) Atrial systole The onset of atrial systole occurs soon after the beginning of the P wave of the electrocardiogram. The transfer of blood from atrium to ventricle. A Graph of the Cardiac Pressure-Volume Relationship Reveals the Sequence of Dynamic Changers During Single Cardiac Cycle The two major heart sounds are produced mainly by closure of the cardiac valves Four sounds are usually produced by the heart, but only two are ordinarily audible through a stethoscope. With electronic amplification the heart sounds, even the less intense sounds, can be detected and recorded graphically as a phonocardiogram. The first heart sound is initiated at the onset of ventricular systole and consists of a series of vibrations of mixed, unrelated low frequencies (a noise). It is the loudest and longest of the heart sounds. The second heart sound, which occurs with closure of the semilunar valves , is composed of higher-frequency vibrations (higher pitch), is of shorter duration and lower intensity, and has a more snapping quality than the first heart sound. The third heart sound is usually not audible, but it is sometimes heard in children with thin chest walls or in patients with left ventricular failure. A fourth, or atrial sound, consisting of a few Iow-frequency oscillations, is occasionally heard in healthy individuals. The length-force relationship of myocardial fibers determines myocardial contraction Skeletal muscle and cardiac muscle show similar length-force relationships. The developed force is maximal when cardiac muscle begins contracting at resting sarcomere lengths of 2.0 to 2.4 m. 0.35 1.5µm 0.65 Z 0.35 M 0.65 0.20 sarcomere At such lengths, overlap of the thick and thin filaments is optimal, and the number of cross bridge attachments is maximal Z Developed force (the force attained during contraction) may be expressed as ventricular relationship of force-length or systolic pressure, pressure- initial volume. Myocardial resting fiber length This is known as the Frankmay be expressed as endStarling relationship, named after diastolic ventricular volume. the scientists who first described it. The pressure-volume curve in diastole is flat at low volumes. Thus, large increases in volume can be accommodated with only small increases in pressure; that is, the ventricle is compliant. Nevertheless, the systolic pressure is considerable at the lower filling pressures. The ventricle becomes much less The normal heart operates compliant with greater filling, only on the ascending portion however, as evidenced by the sharp rise of the diastolic curve at of the Frank-Starling curve (upper curve). large intraventricular volumes. Excitation-contraction coupling is mediated by Ca 2+ • The heart requires optimum concentrations of Na+, K+ and Ca++ to function normally. ? • Ca++ is also essential for cardiac contraction. Removal of Ca++ from the extracellular fluid decreases contractile force and eventually causes arrest in diastole. • Conversely, an increase in the extracellular Ca++ concentration enhances contractile force, but very high Ca++ concentrations induce cardiac arrest in systole (rigor). Preload and afterload are determinants of cardiac performance Preload and afteload in a papillary muscle A, Resting stage in the intact heart just before opening of the AV valves. B, Preload in the intact heart at the end of ventricular filling. C, Supported preload plus afterload in the intact heart just before opening of the aortic valve. D, Lifting preload plus afterload in the intact heart: ventricuiar ejection with decreased ventricular volume. AL, Afterload; PL, preload; PL and AL, total load. The preload can be increased by greater filling of the left ventricle during diastole. At lower end-diastolic volumes, increments in filling pressure during diastole elicit a greater systolic pressure during the subsequent contraction. Systolic pressure increases until a maximum systolic pressure is reached at the optimum preload. If diastolic filling continues beyond this point, no further increase in developed pressure occurs. At very high filling pressures, peak pressure development in systole is reduced. optimum preload At a constant preload, a higher systolic pressure can be reached during ventricular contractions by raising the afterload (increasing aortic pressure). Increments in afterload produce progressively higher peak systolic pressures. If the afterload continues to increase, it becomes so great that the ventricle can no longer generate enough force to open the aortic valve At this point, ventricular systole is totally isometric there is no ejection of blood and thus no change in the volume of the ventricle during systole. Force and velocity are functions of the intracellular concentration of free Ca++. When velocity is constant, force equals the afterload during contraction of the muscle. Force and velocity are inversely related. Preloads and afterloads depend on certain characteristics of the vascular system and the behavior of the heart. In heart failure the preload can be substantially increased ; In essential hypertension the high peripheral resistance augments the afterload Contractility Contractility represents the performance of the heart at a given preload and afterload at constant heart rate. Contractility can be augmented by certain medications, such as norepinephrine or digitalis, and by an increase in contraction frequency (tachycardia). The increase in contractility (positive inotropic effect) produced by any of these interventions is reflected by increments in developed force and velocity of contraction. • A hypodynamic heart is characterized by an elevated enddiastolic pressure, a slowly rising ventricular pressure, and a somewhat reduced ejection phase (curve C). A hyperdynamic heart (such as a heart stimulated by norepinephrine) shows a reduced end-diastolic pressure, a fastrising ventricular pressure, and a brief ejection phase (curve B). The slope of the ascending limb of the ventricular pressure curve indicates the maximum rate of force development by the ventricle (maximum rate of change in pressure with time, maximum dP/dt, the slope provides an index of the initial contraction velocity and hence contractility.