Clinical Conference
advertisement

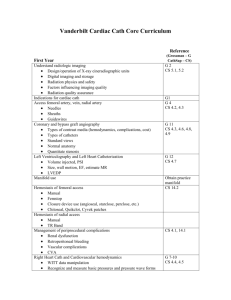
Clinical Conference HPI • 74 y/o female with hx of: – diastolic dysfunction – COPD – Lt ICA aneurysm – presents to the ER 3 MONTHS AGO with chest pain – CHEST PAIN: • Left sided • started at rest • 7/10 • throbbing, intermittent and non-radiating • No alleviating or exacerbating factors • Some shortness of breath which was relieved with her home O2. • No associated palpitations, diaphoresis, nausea. Other History PMH: • Diastolic dysfunction • Left ICA Aneurysm • COPD • HTN • Glaucoma • s/p abd hysterectomy ~2000 Social Hx: • quit tobacco many years ago • denied EtOH and drugs FH: • Denies family history of DM, HTN, CAD. Meds • • • • • • • • • Asa 325mg Po Qday Digoxin 125mg Po Qod Isosorbide Dinitrate 40mg Tid Lisinopril 40mg Po Qday Metoprolol 200mg Po Qday Simvastatin 20mg Po Qday Hydralazine 100mg Po Tid Lansoprazole 30mg Po Qday Lasix 20mg Po Bid Physical Exam • • • • Vitals: T: 36.6, BP:156/104, HR: 75, RR: 18, SaO2: 96% on 2L Gen: alert and oriented X3, no acute distress Heent: op clear, poor dentition, eomi, right eyelid slightly edematous Cardiovascular: – – – – – – – Non-displaced non-sustained PMI ; no thrills or heave Nl carotid upstroke and volume; no bruits RR, No S3 or S4 II/VI holosytolic murmur at LLSB; no friction rub. JVP 7; no HJR Warm LE, no edema. Nl radial, femoral, DP and PT pulses. • Pulm: clear bilaterally without crackles • Abd: soft, non-tender, normoactive bowel sounds, no ascites; no organomegaly. Pertinent Labs Na: 139 K: 3.9 BUN:20 Creat: 0.9 CK: 125 CKMb: 1.3 Trop: <0.05 Lipids: TC 169 Trig 110 HDL 41 LDL 106 EKG 11/06 Old EKG 7/05 ECHO 7/06 ECHO TWO-DIMENSIONAL STUDY • Global left ventricular function is normal. • Left ventricular wall thickness is moderately increased. • The aortic valve is mildly sclerotic but opens well. DOPPLER EVALUATION • Mild tricuspid regurgitation. • The pulmonary artery systolic pressure is 31mmHg. • Left ventricular inflow pattern reflects diastolic dysfunction. Pulmonary vein flow is normal. CONCLUSION • Normal left ventricular size and systolic function (function has very significantly improved from study of 7/5/05). • Diastolic dysfunction. Stress Dipyridamole Gated SPECT Myocardial Perfusion Study • Ischemic changes in the apical and inferior walls w/ apical thinning • SSS 11 • EF 45% Cath Cath LHC 11/06: • LEFT MAIN: Angiographically normal. • LEFT ANTERIOR DESCENDING: Mild diffuse disease; 30% mid. • LEFT CIRCUMFLEX CORONARY ARTERY: Mild diffuse disease; segments appears slightly diffusely aneurysmal. • RIGHT CORONARY ARTERY: Slow flow through right coronary artery; is dominant, tortuous right coronary artery; diffusely aneurysmal. • PLAN: medical management – Started statin. – Up-titrated nitrates. – F/U as outpt….. 3 months later….. Presents to ER w/ c/p story and physical exam almost identical to that in Nov 06….however….. EKG EKG from 11/06 EXAM Unchanged from previous, specifically: no rales no s3, no change in the prior murmur no le edema carotid exam w/ continued nl upstroke and volume. C/P resolved w/ IV BB and nitrates… Pertinent Labs • • • • CK: 214 CKMB: 14.1 Trop: 4.89 BNP: 316 (prior BNP was 112) • • Na: 146 / Cl: 106 / BUN: 17 K: 4.1 / HCO3: 27 / Creat: 1.3 • 9.5>13.2<167 Follow-up Labs • • • Troponin: 4.89 -> 6.36 CKMB: 14.1 -> 13.5 CK: 214 -> 250 Cath Cath 3/07 • • • • • • • diffusely ectatic/aneurysmal coronaries TIMI2 flow in the left system TIMI1 flow in the right system saddle proximal LAD/DIAG filling defect with extension of the defect into the DIAG1 mid LCX - 50% ostial RCA - 50% severely depressed LVEF globally, diffuse moderate-severe HK with somewhat worse anterolateral wall, EF 30-35%, trivial MR, no LV-AO gradient at time of pullback Now What??? Pt started on Reopro overnight and repeat cath the next morning…. Cath 3/23/07 No significant change in thrombus burden…pt underwent thrombectomy and anticoagulation w/ heparin initiated post cath. Coronary artery ectasia (CAE) Also known as aneurysmal CAD Definition: localized or diffuse nonobstructive lesions of the epicardial coronary arteries that exceed the diameter or the normal adjacent segments of the largest coronary vessel Per CASS registry: dilatation is > or = to 1.5 times the adjacent normal coronary artery. CAE Types: -Saccular -Fusiform Classifications: (Markis et al, AJC 1976) Type I: diffuse ectasia with aneurysmal lesions in two vessels Type II: diffuse ectasia in one vessel and discrete ectasia in another Type III: diffuse ectasia in one vessel Type IV: discrete ectasia in one vessel CAE Areas of involvement: Prox and mid RCA (68%): most common sites Prox LAD (60%) Prox LCx (50%) LM – rare, ~0.1% CAE Causes: Pahlavan PS et al, Clin Card, 2006 CAE Pathogenesis -poorly understood -possible factors that are involved in vessel wall weakening: -systemic hypertension -inflammatory stimuli e.g. tobacco -hyperhomocysteinemia -genetic factors, assoc with HLA genes -increased inflammatory response in the vessel wall -activation of matrix metalloproteinases, may degrade structural proteins of connective tissue CAE Epidemiology: Baman TS et al, AJC 2004 CAE Presentation: -typically present with exertional angina -usually do not present with AMI, sudden death -can be complicated by thrombus formation, distal embolization, shunt formation, rupture -assoc with microvascular dysfunction CAE Management options: -aggressive risk factor modification -antiplatelet, anticoagulants -statins => may inhibit metalloproteinases -stenting e.g. covered stents -surgical excision, ligation, CABG