HPI
advertisement

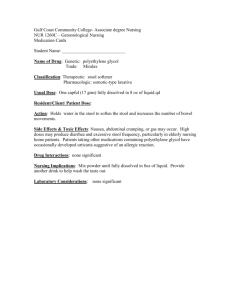
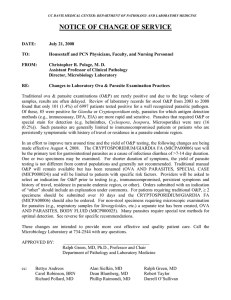
26 year old female from Texas presenting with loose stools and bloating for 2.5 weeks. She noticed that she also has intermittent dull abdominal pain 3/5 relieved by bowel movements and exacerbated with meals. She denies fever, chills, significant weight loss and blood in the stools. No other sick contacts at home. Hx of travel to Mexico one month ago. ROS: Negative, except as above Allergies: NKDA PMH: Chlamydia treated with doxycycline 1 year ago. PSH: tonsillectomy at age 10. SH: graduate student; no tobacco or illicit drugs. 23 glasses of wine monthly. OBGYN hx: LMP 2 weeks ago, lasts 5 days and is usually regular. Sexual hx: sexually active with boyfriend. 7 total sexual partners in her lifetime. Contraception: progesterone/estrogen pills. Condoms used occasionally. Infectious - Viruses ( HIV, CMV, HIV, rotavirus etc) - Bacteria ( E. coli, salmonella, shigella, food borne etc) - Parasites: Giardia, Amebiasis, Helminths. IBD - Crohn’s disease - Ulcerative colitis Functional - Irritable bowel syndrome - Biliary colic Autoimmune -Gluten enteropathy Vitals: T 98.1, BP 115/70, HR 80, RR 14, O sat 100% General: Alert and oriented x3, in no distress. HEENT: Normocephalic, PEERLA, EOMI, TM clear, nasal and oral mucosa moist. No oral thrush. Neck: Supple, no cervical lymphadenopathy. Cardiovascular: RRR, normal s1 s2, no murmurs or gallops. Radial pulses 2+ Chest: Lungs clear bilaterally. No chest tenderness. Abdominal: BS+, soft, bilateral lower quadrant tenderness. No rebound tenderness. No tenderness at McBurney’s point and negative Murphy’s sign. Skin: no rashes. Rectal Exams: hemeoccult negative. CBC normal with no eosinophilia. BMP normal. Stool microscopy for ova and parasites: pending Rapid HIV test: negative. RUQ U/S: negative for gallstones Stool microscopy ( for ova and parasites) • Cysts are the infectious form. Trophozoites usually attach to the wall of the small intestine leading to malabsorption, bloating and flatulence. • Trophozoite Protozoan parasite that can cause transient or chronic diarrhea worldwide. Most susceptible population are travelers, immunocompromised individuals and those living in poor sanitary conditions and with insufficient water systems. Transmission: water, food or fecal-oral transmission between infected individual. Clinical presentation: Diarrhea, malaise, abdominal cramps and weight loss. Diagnosis: - Stool microscopy: sensitive and specific. - Immunoassays: highest sensitivity. Used if stool microscopy results are not definitive. - Duodenal histopathology: villous atrophy Treatment: Metronidazole for 5-7 days. May acquire transient lactose intolerance so advice to avoid lactose containing products for a few weeks.