HISTORY TAKING GIT
advertisement

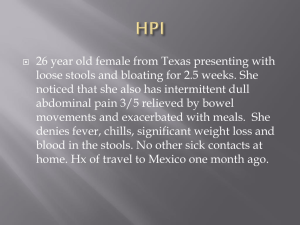
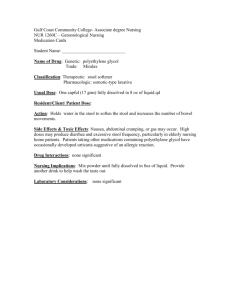
HISTORY TAKING GIT Dr. SOFI MD; FRCP (London); FRCPEdin; FRCSEdin DIFFICULTY IN SWALLOWING & NAUSEA AND VOMITING History of Presenting Complaint • Mouth– Pain, Ulcers, Growths? • DysphagiaOnset, Progression, Solids and /or liquids • Odynophagia – pain on swallowing – oesophageal candidiasis • Progressive dysphagia, i.e. difficulty with solids at first, then with liquids, suggests the presence of a malignant stricture. Especially in elderly patients with associated weight loss & iron deficiency anemia. Nausea & Vomiting • Frequency & Volume – patient may be dehydrated & have electrolyte disturbances • Projectile? – obstruction • What does the vomit look like? • Undigested food – pharyngeal pouch, achalasia, oesophageal stricture • Non-bilious vomit – pyloric obstruction (i.e. pyloric stenosis) • Bilious vomit/ Faecal matter – lower GI obstruction (i.e. severe constipation) • Time of day – Related to meals? Related to lying down in bed? (GERD) Target questions Has there been a gradual problem with When taking a history of dysphagia (difficulty swallowing) ask the patient: solids or liquids? How is your appetite? • What have you found most difficult to Have you lost any weight? Do you smoke? swallow? Solids or liquids, or both? Drink alcohol? Oesophageal malignancy • Where does the food stick? Do you find your swallowing problems • When did you first notice this? come only every so often? Do you suffer • Did it come on suddenly one day or has it been a gradual process? from heartburn? Do you have problems • When does it happen? drinking hot drinks? Gastro-oesophageal • Do you find it is painful to swallow? reflux disease (GERD) (odynophagia) Do you find your swallowing gets worse • Has food ever gone down the wrong way? over the course of the day and towards the • Do you have a cough or feel short of end of the meal? Do you become more breath? physically tired and weak over the course of Target questions the day? Myasthenia gravis Does it happen only intermittently? Oesophageal spasm Do you find the skin over your fingers and Do you gurgle when drinking? Pharyngeal lips is tight? Do your fingers get cold, pouch Are you on iron tablets? Plummer – painful and change colour? Systemic Vinson syndrome sclerosis Dysphagia HEMATAMESIS Hematemesis When taking a history of hematemesis (blood in vomit), ask the patient: • When did it start? • Was this of sudden onset or have there been previous smaller episodes? • How much blood did you vomit? • Is it fresh blood or clotted blood? Does it look like coffee grounds? Target questions Were you retching or vomiting before the blood? Mallory – Weiss tear Do you have pain in your upper abdomen? Do you have any past history of indigestion or ulcer disease? Ulcer bleed Are you on painkillers or bloodthinning drugs? Gastritis from NSAIDs, aspirin, warfarin Do you drink alcohol and how much? Have you any liver problems? Variceal bleed Have you noticed any weight loss or decreased appetite? Any problems swallowing? Upper GI cancer Is the stool black in colour? Melena PAIN ABDOMEN/BLOATING & ALTERED BOWEL HABITS Abdominal Pain Pain – if pain is a symptom, clarify the details of the pain using SOCRATES Site – where exactly is the pain / where is the pain worst Onset – when did it start? / did it come on suddenly or gradually? Character – what does it feel like? (sharp stabbing / dull ache / burning?) Radiation – does the pain move anywhere else? (e.g. chest pain with left arm radiation) Associations – any other symptoms associated with the pain (e.g. chest pain with SOB) Time course – does the pain have a pattern (e.g. worse in the mornings) Exacerbating / Relieving factors – anything make it particularly worse or better? Severity – on a scale of 0-10, with 0 being no pain & 10 being the worst pain you’ve ever felt Is pain localised to specific area of ab domen? • RIF – appendicitis, crohn’s disease • LIF – diverticulitis • Epigastric – peptic ulcer disease, gastritis Indigestion / Heartburn – suggestive of GERD / gastric ulcer Bloating (5F’s) • Fat – obesity • Flatus – paralytic ileus, obstruction • Faeces – constipation • Fluid – ascites • Foetus – pregnancy Altered Bowel Habit Diarrhoea Onset – sudden onset (gastroenteritis, IBD) Consistency – how formed is it? (Bristol stool chart) Blood – Fresh red blood (anal fissure, haemorrhoids). Melaena (UGI bleed, malignancy) Mucous – IBS, IBD Urgency– IBD, IBS, Gastroenteritis Incontinence – Cauda equina / Rectal malignancy Recent Antibiotics? – C. Difficile Constipation – Onset/Timing/Straining/Bleeding Colour of stool: • Melaena (Upper GI) – PUD / duodenal ulcer / malignancy • Fresh Blood (colon,rectum, superficial) – anal fissure / haemorrhoids / rectal tumour • Pale (Steatorrhoea) – Biliary obstruction (gallstones / malignancy) Diarrhoea When taking a history of diarrhea, ask the patient: • How long have you had it for? Longer than 2 weeks? • When was the last formed stool that you passed? • What is the consistency of the stool? • How often do you pass stool? How much stool do you pass? • Have you noticed any blood in your stool? • Do you get this regularly? • Have you been previously investigated for this? Target questions Do you have blood in your diarrhea? Do you have abdominal pain? Do you have mouth ulcers? Do you have a family history of inflammatory bowel disease? Inflammatory bowel disease Have you lost weight? Have you had any loss of appetite? Do you have alternating constipation and diarrhoea? Do you have the feeling of not completely emptying your bowels? Have you had it for more than 2 weeks? Colonic carcinoma Do you find your stool floats and has a greasy appearance? Malabsorption, e.g. pancreatic insufficiency/coeliac disease Do certain foods seem to cause the diarrhea more than others? Coeliac disease Have you recently taken antibiotics? Antibiotic induced Are you on laxatives? Laxative abuse Are you diabetic? Autonomic neuropathy Have you any thyroid problems? Do you feel hot and shaky? Do you find your appetite increased? Thyrotoxicosis JAUNDICE Jaundice When taking a history of jaundice, ask the patient: • When did you first notice the yellow tinge to your skin and eyes? • Have you ever had this before? Target questions Have you any family history of jaundice? What medications have you been taking? Prehepatic, e.g. Gilbert’s syndrome How much alcohol do you drink? What medications are you on? Have you had any recent blood transfusions? Where have you travelled recently? Have you had unprotected sex recently? Do you inject intravenous drugs? Have you eaten any shellfish? Do you have any tattoos? Have you been in contact with someone with jaundice? Hepatic, e.g. viruses Have you noticed any change in the colour of your urine or stool? Are you itchy? Do you feel bloated? Do you have any abdominal pain? Have you any history of gallstones? Have you had any weight loss or loss of appetite? Posthepatic, e.g. cholangiocarcinoma, pancreatic carcinoma PEPTIC ULCER PEPTIC ULCERATION Symptoms • Epigastric pain: • – Duodenal ulcer- occurs before eating & is relieved by eating – Gastric ulcer – occurs after eating & is worsened by eating • • • • • Nausea Oral flatulence Vomiting Weight loss Symptoms relieved by antacids – non-specific • Haematemesis • Melaena Signs • Often very few signs in uncomplicated cases • Epigastric tenderness Differential Diagnosis • Ulcer Gastric Malignancy GERD Gallstones Chronic pancreatitis Red Flags • GI Bleeding • Dysphagia • Unintentional weight loss • Abdominal swelling • Persistent vomiting CROHN’S DISEASE Symptoms • Abdominal pain • Diarrhoea – may or may not be bloody • Weight loss • Fever • Malaise • Nausea & Vomiting – can occur due to strictures / bowel obstruction • Perianal Discomfort – itching, pain – due to fistulas / abscesses • Aptheous ulcers Signs • Abdominal tenderness • Abdominal masses – most commonly right iliac fossa (terminal ileum) • Perianal abscesses / skin tags • Fistula’s • Rectal strictures – may be noted on PR Extra-intestinal Features of Crohn’s • Finger clubbing • Episcleritis / Uveitis – inflammation of the episclera or uvea • Seronegative Spondylarthropathy – inflammation of axial skeleton – Rh factor -ve • Erythema Nodosum – red tender nodules which are usually located over the shins • Pyoderma Gangrenosum – necrotic deep ulcers, often on the legs • Deep Vein Thrombosis • Autoimmune haemolytic anaemia – antibody mediated lysis of RBC’s Inspection Quadrants of the Abdomen Topical Anatomy of the Abdomen Various Causes of Abdominal Distension Obese abdomen Ascites Hepatomegaly Markedly enlarged gall bladder Palpation of liver • With patient supine, place right hand on patient's abdomen, just lateral to the rectus abdominis • Ask patient to take a deep breath and try to feel the liver edge as it descends. • Be sure to allow liver to pass under the fingers of your right hand, note texture. Pressing too hard may interfere. Abdominal Palpation Hooking Edge of the Liver Percussion of liver Technique 1. Starting in the midclavicular line at about the 3rd intercostal space, lightly percuss and move down. 2. Percuss inferiorly until dullness denotes the liver's upper border (usually at 5th intercostal space in MCL). 3. Resume percussion from below the umbilicus on the midclavicular line in an area of tympany. 4. Percuss superiorly until dullness indicates the liver's inferior border. 5. Measure span in centimeters. Abdominal Percussion Palpation of spleen • Start in the right lower quadrant and proceed diagonally toward the left upper quadrant. • Attempt to feel spleen with superficial palpation technique • With each step, ask the patient to take a deep breath. • Feel for the tip of the spleen. Bimanual palpation Stand on the patient's right side and with your left hand, pull the patient's rib cage anteriorly and palpate for the tip of the spleen (if enlarged) with your right hand as the patient takes a deep breath. Palpation of Kidney The ballottement method is normally used. • Keep your anterior hand steady in the deep palpation position in the right upper quadrant lateral and parallel to rectus muscle. • Attempt to ballot the kidney with the other hand in costophrenic angle. • An enlarged kidney should be palpable by the anterior hand. • Repeat the same maneuver for the left kidney. Normal: In an adult, the kidneys are not usually palpable, except occasionally for the inferior pole of the right kidney. The left kidney is rarely palpable. An easily palpable or tender kidney is abnormal. However, the right kidney is frequently palpable in very thin patients and children. Auscultation 1. Are bowel sounds present? 2. If present, are they frequent or sparse (i.e. quantity)? 3. What is the nature of the sounds (i.e. quality)? Abdominal Auscultation Assessing for a fluid thrill