Communication
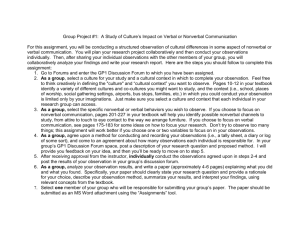
advertisement

Basic Concepts of Communication Dr. Belal M. Hijji, PhD, RN Febuary 6, 2011 Learning Outcomes By the end of this lecture, students will be able to: • Define the communication process and identify its components • Describe the component system of communication • Identify the factors that impact on verbal communication • Describe the importance of nonverbal communication in health care settings • Discuss the factors that impact on nonverbal communication • Identify communication style factors that influence the nurseclient relationship • Describe the levels and types of communication • Discuss the various techniques of therapeutic communication 2 The Communication Process and its Components Communication: It is the process of transmission thoughts, feelings, facts, and other information. In nursing, communication is a vehicle for establishing therapeutic relationship with the patient. The quality of patient client relationship is dependent on the quality of communication between them. Its components are: • Sender: Generates a message which stems from the person’s need to relate to others, to create meaning, and to understand various situations. • Message: Is a stimulus produced by a sender. Messages may be verbal, nonverbal, written material, and arts. • Channel: The medium through which a channel is transmitted. Channels are visual, auditory, and kinesthetic. 3 • Receiver: Is the person who receives and interprets the sender’s message. Receiving is influenced by complex physiological, psychological, and cognitive processes. • Feedback: Is the information the sender receives about the receiver’s reaction to the message. 4 Basic concepts of Communication Metacommunication Definition: It is a broad term used to describe all factors that influence how a message is perceived or interpreted (Slide 4). For ten years (1952-1962), Bateson and colleagues conducted research on communication, and pioneered the concept of metacommunication. Verbal and nonverbal components of communication are interrelated; they need to be congruent with each to avoid misinterpretation. 5 Metacommunication Culture Native language Gender Vocal pitch Body language Culture Gender Appearance Factors in communication styles 6 Verbal Communication Spoken words are symbols that people use to think about ideas, to share experiences with others, and to validate the meaning of perceptions about the world and one’s place in. Spoken words are essential for classifying and ordering information in ways that individuals understand them. Feedback on spoken words is essential in enabling mutual understanding of the meaning of a message. 7 Factors Impacting on Verbal Communication • Culture: Many nurses lack an understanding of communication principles and techniques of effective communication with patients from other than their own culture. – Effective communication requires, amongst others, knowledge of the values of another person’s culture. Example: A Muslem patient admitted in Ramadan in a UK hospital. • Language: Nurses need to be proficient in the language of the patient they care for. Otherwise, the communicative process will be impaired which will negatively impact on the quality of care. 8 • Gender: Gender differences in communication patterns exist between men and women in both the content and process. – Content: • Men use less verbal communication that women. • Women tend to disclose more personal information than men • Men are more likely to initiate an interaction, talk more, interrupt and use hostile language, when discussing issues. – Process: • In health care settings, women use more active listening, using encouraging responses, and using more supportive words. 9 • Vocal pitch and tone: – Paralanguage: is the oral delivery of a verbal message, expressed through tone of voice and inflection, sighing, or crying. – Understanding paralanguage affects how the verbal message is likely to be interpreted. – A statement by a nurse in a voice that sounds rushed, high pitched, or harsh is likely to be misinterpreted by the patient, although the nurse’s intention is good. In contrast, the same statement made in soft, unhurried voice would express genuine interest. – To achieve mutual understanding, the tone of voice should support the content of the message. 10 Nonverbal Communication Function: To convey cues about a content to be communicated. Channels: Facial expression, eye movement, body movement, posture, gestures, touch, and proxemics. Confusion arises when the nonverbal cue is inconsistent with the verbal message. Therefore, congruency aids understanding. Nurses use nonverbal communication to build rapport with patients. The patient’s nonverbal behaviour may reveal important information that affect nurse-patient relationship. 11 Factors That Affect Nonverbal Communication Body language: Your body language is as important as your patient’s. During history taking, keep your body posture relaxed to convey a calm, reassuring attitude. Work at the same level as your patient. Standing over her/ him conveys a sense of dominance and authority, enhancing her/ his sense of dependence. Give reaffirming gestures such as nodding. Your facial expression should convey care and concern. Maintain eye contact to show the patient you are interested in what s(h)e has to say. 12 • Culture: Nonverbal gestures convey different meanings in different cultures. Putting thumb and index finger into a circle means “approval” in the American culture, but is an obscene gesture in Brazil. – Touch: As Muslems, touch is prohibited between a man and a woman who are from outside of family. However, touch in health care is important component of assessment. Therefore, care needs to be taken so that the use of touch is not misinterpreted. • Gender: Women tend to demonstrate more effective use of nonverbal communication and are better decoders of nonverbal meaning. • Women tend to use more facial expression, smiling more often, maintaining eye contact, and touching more often. • Men prefer a greater interpersonal distance between themselves and others. 13 • Appearance: For example, a patient who tells you he is having “crushing chest pain” should look like he is having “crushing chest pain.”His nonverbal behavior should be consistent with what he is telling you. A relaxed posture with arms at the sides conveys openness, whereas a tense posture with arms crossed may reflect anger, discomfort, or mistrust. A tense, guarded posture may also indicate pain. A tripod position (sitting position, leaning forward with elbows on table and hands supporting head) is assumed to ease breathing. 14 Interpreting Nonverbal (Slide 15) Body Cues • The emotional component of a message can be indirectly interpreted by observing the client’s body language. • Body stance may convey a message about an individual. – Direct eye contact while talking or listening create more a sense of confidence and credibility than turning one’s body to one side. – A slumped, head-down posture and slow movements may indicate lassitude or low self-esteem; erect posture and decisive movements suggest confidence and self-control. – Rapid, diffuse, and agitated body movements may suggest anxiety. 15 • Downward glances or averted eyes signal submission, weakness, or shame. • Facial expression either reinforces or modifies the message being conveyed. In circumstances of incongruence, nonverbal expression assumes prominence and generally is perceived as more trustworthy than the verbal content. • Is your facial expression always an indicator of emotional response to a situation? 16 17 Style Factors That Influence Nurse-Client Relationship • Responsiveness of participants: – How responsive the participants are affects the depth and breadth of communication. – Nurses should direct efforts to increase the responsiveness of less verbal clients, through verbal and nonverbal approvals, active listening, demonstration of empathy, and acknowledgment of the content and feelings of messages. – Sometimes, acknowledging the difficulty a client has in expressing certain feelings, praising efforts, and encouraging use of different routes of communication helps promote responsiveness. 18 • Roles of participants: – The relationship between the roles of the sender and of the receiver influence how a message is likely to be received and interpreted. – A statement of constructive criticism issued by a friend and by one’s immediate supervisor may be interpreted differently. – Communication between nurses and their supervisors is more likely to be influenced by power and style than by gender. – More powerful supervisors tend to speak in a more dominant style 19 • Validation of individual worth: – A caring style conveys a message of individual worth and this fosters the relationship with the clients. – Confirming responses validate the intrinsic worth of an individual. These responses that affirm the individual’s right to be treated with respect, and affirm his autonomy. – Disconfirming responses disregard the validity of feelings. Such responses take the form of changing the topic, or presuming to know what a client means without verifying the message with him. 20 • Context of the message: – Communication is always influenced by the environment in which it takes place. – Nurses should take sometime to evaluate the physical setting, time, and space in which contact takes place, in order to select the most appropriate context. 21 • Involvement in the relationship: – Relationships generally develop over time – Hospital nurses have less time to develop relationships with patients – Community-based nurses may have greater opportunities to develop relationships – Nurses’ should be aware of behaviours that increase a client’s involvement and apply them – Nurses should be aware of behaviours that decrease involvement and avoid them 22 Levels of Communication • Intrapersonal level: This is the message one sends to oneself, including a self talk, or communication with oneself. • Interpersonal level: Is the process that occurs between two people either in face-to-face encounter, over the phone, or through other communication media. • Group communication: This occurs when 3 or more people meet in face-to-face encounters or through another communication medium. An example is a focus group interviews. 23 Types of Communication • Interdisciplinary communication: The health care team consists of the patient and all medical personnel involved in providing care. Each member of the medical performs important, though different, role and responsibility. Members of the team should communicate with each other regarding assessment, interventions, and client status. • Therapeutic communication: Is the use of communication for the purpose of creating a beneficial outcome for the patient. 24 Principles of Therapeutic Interaction • • • • • • • • Choose an appropriate interview time Assure privacy Establish guidelines for therapeutic interaction Provide for comfort during interaction Accept the client as is Encourage spontaneity Focus on the client, avoid talking for the sake of curiosity Encourage the expression of feelings 25 Techniques of Therapeutic Communication • Affirmation/Facilitation. Acknowledge the patient’s responses to reassure him that you are paying attention. • Silence. Sometimes this may facilitate communication. Periods of silence allow your patient to collect her or his thoughts before responding. Silence also gives you more time to think and plan your responses. • Clarifying. If you are unsure or confused about what your patient is saying, rephrase what she said and then ask the patient to clarify. • Restating. Indicates to the patient that you are listening and acknowledging his feelings. • Active Listening. Pay attention, maintain eye contact, and really listen to what your patient tells you both verbally and nonverbally. Active listening conveys interest and acceptance. 26 • Broad or General Openings. This technique is effective when you want to hear what is important to your patient. Use openended questions such as," What would you like to talk about?” • Reflection. Reflection allows you to acknowledge your • patient’s feelings, encouraging further discussion. • Humor. Humor ( )الدعابة والفكاهةcan be very therapeutic when used in the right context. It can reduce anxiety, help patients cope more effectively, put things into perspective, and decrease social distance. • Informing. Giving information allows your patient to be involved in his or her healthcare decisions. • Redirecting. Redirecting your patient helps keep the communication goal-directed. Keep your patient on track. 27 • Focusing. Focusing allows you to hone in on a specific area, encouraging further discussion. Examples include: “You said your mother and sister had breast cancer?” or “Do you do BSE, and have you ever had a mammogram?” • Sharing Perceptions. With this technique, you give your interpretation of what has been said in order to clarify things and prevent misunderstanding. • Identifying Themes. Identifying recurrent themes may help your patient make a connection and focus on the major theme. For example, you might say, “From what you’ve told me, it sounds like every time you were discharged from the hospital to home you had a problem.” • Sequencing Events. If your patient is having trouble sequencing events, you may need to help her or him place the events in proper order. 28 • Suggesting. Presenting alternative ideas gives your patient options. Suggesting is also a good teaching tool. For example, if the patient says, “I’ve tried so hard to lose weight, but I can’t,” you might say, “Have you tried combining diet and exercise?” • Presenting Reality. If your patient seems to be exaggerating or contradicting the facts, help her or him re-examine what has already been said and be more realistic. • Summarizing. Summarizing is useful at the conclusion of a major section of the interview. It allows the patient to clarify any misconceptions you may have. For example, you might say, “Let me see if I have this correct: You came to the hospital with chest pain, which started an hour ago, after eating lunch.” 29