Lecture Slides
advertisement

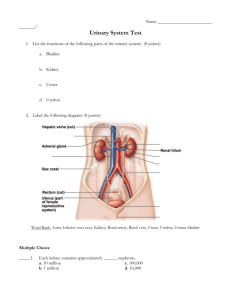
The Urinary System Functions of the urinary system • • • • Homeostatic regulation of blood plasma • • • • Regulating blood volume and pressure Regulating plasma ion concentrations Stabilizing blood pH Conserving nutrients Filter many liters of fluid from blood Excretion - The removal of organic waste products from body fluids • Urea • Uric acid • Creatinine Elimination - The discharge of waste products into the environment Urinary System • • • • Kidneys – produce urine Ureters –transport urine to bladder Urinary bladder stores urine Urethra transports urine to exterior Figure 26.1 Location and External Anatomy of Kidneys • Located retroperitoneally • Lateral to T12–L3 vertebrae • Average kidney • • Hilus • • • 12 cm tall, 6 cm wide, 3 cm thick On concave surface Vessels and nerves enter and exit Renal capsule surrounds the kidney Urinary System in Gross Dissection Figure 26.3 Internal Gross Anatomy of the Kidneys • Frontal section through the kidney • • • • Renal cortex Renal pyramids Renal pelvis • Major calicies • Minor calicies Gross vasculature • • Renal arteries Branch into segmental arteries Anatomy of the kidneys • Superficial outer cortex and inner medulla • • The medulla consists of 6-18 renal pyramids The cortex is composed of roughly 1.25 million nephrons • Major and minor calyces along with the pelvis drain urine to the ureters Nephron – The Functional Unit of Kidney • Nephron consists of: • Renal corpuscle • Renal tubule: • Proximal • convoluted tubule (PCT) • Loop of Henle • Distal convoluted tubule (DCT) Nephron empties tubular fluid into a system of collecting ducts and papillary ducts • Renal Corpuscle Consists of: • Glomerulus – tuft of fenestrated capillaries • Glomerular (Bowman’s) capsule • Parietal layer – simple squamous epithelium • Visceral layer – consists of podocytes • Blood travels from efferent arteriole to peritubular capillaries • Blood leaves the nephron via the efferent arteriole Renal Corpuscle and the Filtration Membrane Figure 23.6a Glomerulus anatomy • Podocytes cover lamina densa of capillaries • Project into the capsular space • Pedicels of podocytes separated by filtration slits Two types of nephron • Cortical nephrons • ~85% of all • • nephrons Located in the cortex Juxtamedullary nephrons • Closer to renal • medulla Loops of Henle extend deep into renal pyramids Nephron • Proximal convoluted tubule (PCT) • • • Actively reabsorbs nutrients, plasma proteins and ions from filtrate Released into peritubular fluid Loop of Henle • • • Descending limb Ascending limb Each limb has a thick and thin section Nephron • Distal convoluted tubule (DCT) • Actively secretes • ions, toxins, drugs Reabsorbs sodium ions from tubular fluid Collecting Tubules (Collecting ducts) • Collecting tubules - Receive urine from distal convoluted tubules Figure 23.8 Uriniferous Tubule Figure 23.5a Types Of Capillary Beds In Nephron • Glomerulus - Fed and • drained by afferent and efferent arterioles Peritubular capillaries • • • Arise from efferent arterioles Low-pressure, porous capillaries Absorb solutes • Vasa recta • • Thin-walled looping vessels Part of the kidney’s urineconcentrating mechanism Mechanisms of Urine Production • • • Filtration - filtrate of blood leaves kidney capillaries Reabsorption – most nutrients, water, and essential ions reclaimed Secretion - active process of removing undesirable molecules Microscopic Anatomy of the Kidney • Juxtaglomerular apparatus • Functions in the regulation of blood pressure • Juxtaglomerular cells – secrete renin • Macula densa • A portion of distal convoluted tubule • Tall, closely packed epithelial cells • Act as chemoreceptors Summary of Nephron Function • Each segment of nephron and collecting system contribute • • • • • Glomerulus PCT Descending limb Thick ascending limb DCT and collecting ducts • Concentrated urine produced after considerable modification of filtrate Urine Excretion • Leaves Collecting System • Enters renal pelvis • Rest of urinary system transports, stores and eliminates • • • Ureters Bladder Urethra The Ureters • • • • Pair of muscular tubes Extend from renal pelvis to the bladder Peristaltic contractions force urine from the kidneys to the urinary bladder Oblique entry into bladder prevents backflow of urine Histology of Ureter • • Mucosa – transitional epithelium Muscularis – two layers • • Inner longitudinal layer Outer circular layer • Adventitia – typical connective tissue Urinary Bladder • • A collapsible muscular sac Stores and expels urine • Full bladder – spherical • Expands into the abdominal cavity • Empty bladder – lies entirely within the pelvis Figure 23.13 Urinary Bladder • Wall of bladder • Mucosa - transitional epithelium • Muscular layer - detrusor muscle • Adventitia The urethra • Extends from the urinary bladder to the exterior of the body • Passes through urogenital diaphragm (external urinary sphincter) • Differs in length and function in males and females • Internal urethral sphincter - involuntary smooth muscle • External urethral sphincter - voluntarily inhibits urination, relaxes when one urinates Urinary Bladder and Urethra - Male • • Males – 20 cm in length Three named regions • Prostatic urethra • • passes through the prostate gland Membranous urethra through the urogenital diaphragm Spongy (penile) urethra passes through the length of the penis Figure 23.16a Urinary Bladder and Urethra - Female • • In females - length of 3–4 cm The smooth triangular region of the base is is called the trigone - many bladder infections persist in this region Urethra • Epithelium of urethra • Transitional epithelium at the proximal • • end (near the bladder) Stratified and pseudostratified columnar – mid urethra (in males) Stratified squamous epithelium at the distal end (near the urethral opening) Micturition • • • Bladder can hold 250 400ml Greater volumes stretch bladder walls initiates micturation reflex: Urination coordinated by micturition reflex • • Initiated by stretch receptors in wall of bladder Urination requires coupling micturition reflex with relaxation of external urethral sphincter Blood Flow Through the Kidney