PEDS Exam 1 Fluid Electrolytes Ch 46
advertisement
Fluid & Electrolytes
{
Care of Children
Instructor: Crystal Jensen
Oral Rehydration Therapy
IV Fluid Replacement
Dehydration
Extracellular Edema
Edema
IV fluid overload: ( vs dx process
Sudden weight gain (grams), neck vein distention
Dependent edema (Rt side heart failure)
ankles or sacrum
Tx diuretics
Weigh pt, I/O, weigh diapers (milliliters)
Tx successful: output > intake
Complication: Pulmonary Edema (crackles,
increased RR)
Pain, restricted movement
Inflammatory edema: tx w/ice
Elevation of extremities
Hypernatremia
Because of certain physiologic characteristics,
infants are predisposed to dehydration. They have
a large surface area in relation to their height or
weight compared with adults and have relatively
large evaporative water losses. In infants,
hypernatremia usually results from diarrhea and
sometimes from improperly prepared infant
formula or inadequate mother-infant interaction
during breastfeeding.
The group most affected is intubated, critically ill
patients. Most cases result from a failure to freely
administer water to patients. The incidence of
breastfeeding-related hypernatremia is 1-2%.
Sodium Imbalance
In children with acute hypernatremia,
mortality rates are as high as 20%. Neurologic
complications related to hypernatremia occur
in 15% of patients. The neurologic sequelae
consist of intellectual deficits, seizure disorders,
and spastic plegias. In cases of chronic
hypernatremia in children, the mortality rate is
10%.
When dehydration is severe, skin turgor is reduced,
and the skin develops a characteristic doughy
appearance.
Patients in certain situations or with certain conditions are at risk for hypernatremia:
Hospitalized patients who receive exclusive intravenous fluids
Patients with coma
Newborns
Toddlers
Patients with diabetes insipidus
Patients receiving alkali therapy
Patients with diarrhea
Patients with fever
Patients with renal disorders (eg, dysplasia, medullary cystic disease,
polycystic kidney disease, tubulointerstitial disease)
Patients with obstructive uropathy
Patients with electrolyte disturbances (eg, hypokalemia, hypercalcemia)
Patients with heat stroke or excessive hypotonic fluid loss
Signs and symptoms of hypernatremia include the following:
Irritability
High-pitched cry or wail
Periods of lethargy interspersed with periods of irritability
Altered sensorium
Seizures
Increased muscle tone
Fever
Rhabdomyolysis[2, 3]
Oligoanuria
Excessive diuresis
Hypotnatremia: Case study
Sodium Imbalance
A first-time mother gave birth to a 5-pound girl. The baby is fullterm, but the mother has been concerned that the baby is small.
The mother has decided to feed formula, and so received
instructions in the hospital prior to discharge about proper
formula preparation and storage. Five days after the birth, the
nurse in the pediatric clinic received a call from the mother, who
was concerned because the baby was lethargic and was not
feeding well. The mother was instructed to bring the baby in to
the clinic immediately. Upon questioning, it was learned that the
mother had mixed "strong" formula by adding less water than
directed to a powder formula, in an attempt to have the baby
gain weight more rapidly. What assessments of the baby are
critical? What instructions does the mother need? What followup is required? Fill in the appropriate steps of the Care Plan
below.
Class Activity
Hyperkalemia
Hypokalemia
Word Document
Potassium Imbalance
Hypocalcemia is a laboratory and clinical abnormality that is
observed with relative frequency, especially in neonatal
pediatric patients.
The concentration of calcium in the serum is critical to many
important biologic functions, including the following:
Calcium messenger system by which extracellular messengers
regulate cell function
Activation of several cellular enzyme cascades
Smooth muscle and myocardial contraction
Nerve impulse conduction
Secretory activity of exocrine glands
hypocalcemia produces a wide range of peripheral and CNS effects,
including paresthesias, tetany (ie, contraction of hands, arms, feet,
larynx, bronchioles), seizures, and even psychiatric changes in
children.
Calcium Imbalance
Hypocalcemia continued: Cardiac function may also be impaired because of
poor muscle contractility.
One of the most common causes of hypocalcemia is renal failure
History
In patients with hypocalcemia, the history varies depending on age. In
newborns, patient history can include the following:
Possibly no symptoms
Lethargy
Poor feeding
Vomiting
Abdominal distension
History in children can be as follows:
Seizures
Twitching
Cramping
Laryngospasm, a rare initial manifestation
Calcium Imbalance
Hypocalcemia: Physical Examination-
Children’s symptoms include the following:
Lethargy
Cyanosis
Tremulousness
Seizures
Apnea
Tetany and signs of nerve irritability, such as the Chvostek sign,
carpopedal spasm, the Trousseau sign, and stridor
Abdominal distension
Prematurity, birth asphyxia, or congenital heart disease (features
associated with infants of mothers with diabetes mellitus)
Calcium Imbalance
Hypercalcemia is defined by a high calcium level in the blood.
Calcium is important for bone formation, but is also vital for
normal cell function in all cells.
High levels of parathyroid hormone or vitamin D cause
hypercalcemia. Excessive dietary intake of Vitamin D or Vitamin
A will cause hypercalcemia.
The most common cause of high parathyroid hormone levels in
children comes from a complication of chronic kidney disease.
Kidney stones are a major complication of hypercalcemia that can
cause blood in the urine or severe pain in the back, flank or lower
abdomen. Stomach pain and psychiatric issues also may occur
when blood calcium levels are too high.
Sometimes, children with hypercalcemia develop a severe acute
illness with intense stomach pain and dehydration.
Calcium Imbalance
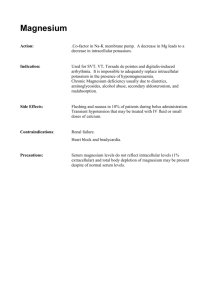
Hypermagnesemia
Hypermagnesemia is an uncommon clinical finding, and
symptomatic hypermagnesemia is even less common. This
disorder has a low incidence of occurrence, because the kidney
is able to eliminate excess magnesium
The most common cause of hypermagnesemia is renal
failure. Other causes include the following[3, 4] :
Excessive intake
Hypothyroidism
Addison disease
Familial
Milk alkali syndrome
Depression
Magnesium Imbalance
Hypermagnesemia
In patients with acute renal failure, hypermagnesemia usually
presents during the oliguric phase; the serum magnesium level
returns to normal during the diuretic phase. If a patient receives
exogenous magnesium during the oliguric phase, severe
hypermagnesemia can result, especially if the patient is acidotic.
One of the earliest symptoms of hypermagnesemia is deep-tendon
reflex attenuation. Facial paresthesias also may occur at moderate
serum levels.
Muscle weakness is a more severe manifestation, occurring at levels
greater than 5 mmol/L. This manifestation can result in flaccid
muscle paralysis and depressed respiration and can eventually
progress to apnea.
Magnesium is also cardiotoxic and, in high concentrations, can
cause bradycardia. Occasionally, complete heart block and cardiac
arrest may occur at levels greater than 7 mmol/L.
Magnesium Imbalance
hypomagnesemia, can result in disturbances in
nearly every organ system and can cause potentially
fatal complications (eg, ventricular arrhythmia,
coronary artery vasospasm, sudden death)
The main controlling factors in magnesium
homeostasis appear to be gastrointestinal absorption
and renal excretion.
Plentiful in green vegetables, cereal, grain, nuts,
legumes, and chocolate. Vegetables, fruits, meats,
and fish
Food processing and cooking may deplete
magnesium content, thus accounting for the
apparently high percentage of the population whose
magnesium intake is less than the daily allowance.
Magnesium Imbalance
Hypomagnesemia- disorders that cause
magnesium and potassium losses, include
diuretic therapy and diarrhea
The classic sign of severe hypomagnesemia (<
1.2 mg/dL) is hypocalcemia
Hypomagnesemia is now recognized to cause
cardiac arrhythmia
At-risk patients include acutely ill patients in
the intensive care unit
Magnesium Imbalance
Neuromuscular irritability, including tremor, fasciculations,
tetany, Chvostek and Trousseau signs, and convulsions, have
been noted with hypomagnesemia
Other manifestations include the following:
Convulsions
Apathy
Muscle cramps
Hyperreflexia
Acute organic brain syndromes
Depression
Generalized weakness
Anorexia
Vomiting
Magnesium deficiency has also been linked to chronic fatigue
syndrome, sudden death in athletes, impaired athletic
performance, and sudden infant death syndrome.
Magnesium Imbalance
Causes of hypomagnesemia related to decreased magnesium
intake include the following[4] :
Causes related to the redistribution of magnesium from
extracellular to intracellular space include the following:
Alcohol withdrawal syndromes
Refeeding syndrome
Acute pancreatitis
Causes related to gastrointestinal magnesium loss include the
following:
Starvation
Alcohol dependence
Diarrhea
Vomiting and nasogastric suction
Gastrointestinal fistulas and ostomies
Diuretics - Loop diuretics, osmotic diuretics, and chronic use of
thiazides
Class Activity:
Create a table to include the following:
Normal range lab values for children (Calcium, Potassium,
Magnesium, Sodium)
Include a column for critical lab values
The last column should provide information r/t nursing
management
Lab Values