The Duke Stroke Policy Model (SPM)
advertisement
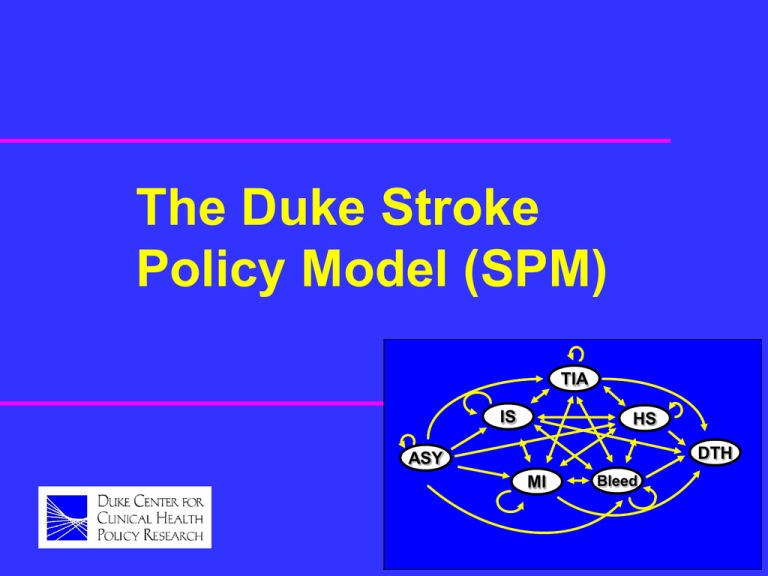
The Duke Stroke Policy Model (SPM) TIA IS HS DTH ASY MI Bleed Developers David Matchar, MD -- principal investigator Greg Samsa, PhD -- project director, statistician Giovanni Parmigiani, PhD -- statistician, software developer Joe Lipscomb, PhD -- health economist Greg Hagerty, MS -- software developer Outline Rationale for modeling (*) SPM described Applying the SPM to a randomized trial Extensions Rationale for modeling Why model? Arguments for modeling Arguments against modeling Discussion Conclusions Application to stroke Why model? (cont’d) “To me, decision analysis is just the systematic articulation of common sense: Any decent doctor reflects on alternatives, is aware of uncertainties, modifies judgements on the basis of accumulated evidence, balances risks of various kinds, . . .” Why model? (cont’d) “ considers the potential consequences of his or her diagnoses and treatments, and synthesizes all of this in making a reasoned decision that he or she decrees right for the patient…” (cont’d) Why model? “… All that decision analysis is asking the doctor to do is to do this a lot more systematically and in such a way that others can see what is going on and can contribute to the decision process.” -- Howard Raiffa, 1980 Advantages of modeling Clarifies decision-making Simplifies decision-making Provides comprehensive framework Allows best data to be applied Extrapolates short-term observations into long-term Encourages “what if” analyses Disadvantages of modeling Ignores subjective nuances of patientlevel decision-making Problem may be incorrectly specified Inputs may be incorrect / imprecise Usual outputs are difficult to interpret or irrelevant to decision-makers Individual decisionmaking is subjective For individual decision-making, primary benefit of modeling is clarification. As normative process, decision-making works better for groups. – Most applications involve group-, rather than individual-level, decisions (e.g., CEA, purchasing decisions, guidelines). An aside Interactive software (possibly including models) shows great potential to help decision-makers (e.g., patients, physicians, pharmacy benefits managers) clarify and make better decisions. – We are developing prototype for a “user-friendly version” of the SPM. Some models are mis-specified A good model will simplify without over-simplifying. Poor models exist, but this need not imply that modeling itself is bad. We need more explicit standards under which models are developed, presented, and assessed. An observation The fundamental problem with many of the poor models in circulation is that they assume the answer they are purporting to prove (often, that a treatment which is trivially effective or even ineffective is nevertheless cost-effective). Users are understandably wary. Model inputs may be incorrect/ imprecise This problem is often most acute for utilities and costs, and least acute for natural history and efficacy. – We need more and better data on cost and quality of life. The less certain the parameter, the greater the need for sensitivity analysis. An aside In practice, the conclusions of a model / CEA are never stronger than the strength of the evidence regarding efficacy. If the evidence about efficacy is weak, then modeling / CEA should not be performed. Usual outputs are difficult to interpret In academic circles, results are presented as ICERs using the societal perspective. – Present this as a base case for purposes of publication / benchmarking. – Also present multiple outcomes from multiple perspectives (vary cost categories, vary time periods, present survival, eventfree survival, QALY, …). General conclusions Modeling is of great potential benefit and indeed is sometimes the only reasonable way to proceed. However, models must be held to a high standard of proof. Although the standard reference model cannot be ignored, modeling should be done flexibly, with the needs of the end user in mind. Application to acute stroke treatment RCTs follow patients in the shortterm, but the large majority of benefits accrue in the long-term. Simple heuristics will not suffice to adequately trade off complex risks, benefits, and costs. Modeling allows a large body of evidence to be efficiently synthesized. Outline Rationale for modeling Stroke model described (*) Applying the SPM to a randomized trial Extensions SPM described History / background Types of analysis Structure Validation / citations SPM history / background SPM development (cont’d) First version developed in 1993 by Stroke PORT Goals of stroke PORT: – Summarize epidemiology of stroke – Describe best stroke prevention practices – Describe current practices, and test methods for improving practice SPM development SPM was used: To summarize epidemiology of stroke To support CEA As a basic organizing structure for the PORT SPM versions Original C++ code (uses waiting time distributions, research tool, difficult to extend) New S+ code (uses waiting time distributions, highly structured code used as development tool, inefficient) New C++/Decision-Maker code (uses Markov-based cycles, intervention language, better interface, extendable) New C++ version Decision-Maker used to specify natural history and effect of interventions in a decision tree format Efficient C++ code used as simulation engine Expandable into a web-based tool