B2B - Back to Basics Pharmacology Review
advertisement

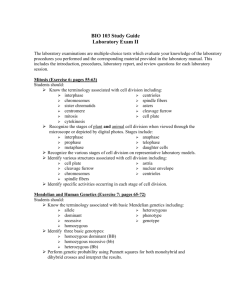
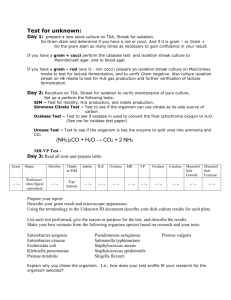
Back to Basics Practical Pharmacology Dr. Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Assistant Professor, Dept of Family Medicine, University of Ottawa Clinical Pharmacist, Bruyere Academic Family Health Team March 2013 rhalil@bruyere.org (Partially adapted from slides by Marc Riachi, R.Ph.) Objectives • Review all pharmacology in an abnormally short amount of time in preparation for LMCC • List the four steps of rational prescribing • Understand the pharmacological classes, generic examples and mechanisms of action of important tools in the practice of medicine. • Understand how the kinetics and dynamics of these agents can affect their use • Highlight clinical pearls in the proper use of these agents in practice. Topics to be covered • • • • • • • • • • • • • • • Antibacterials Antimycobacterials Antifungals Narcotic analgesics Autonomic nervous system Anti seizure drugs Migraines Antidepressants Antianxiety agents Agents for insomnia Antidiabetics Antilipemics Antihypertensives Diuretics Nitrates Ref: Marc Riachi, RPh • • • • • • • • • • • • • • Antiplatelets and anticoagulants Antiasthmatics BPH Erectile dysfunction Dementia Parkinson’s disease and schizophrenia Dyspepsia, GERD and PUD Antiemetics IBD IBS Osteoporosis Gout OTC drugs Appendix I & II Topics to be covered in this lecture • • • • • • • • • • • • • • • Antibacterials Antimycobacterials Antifungals Narcotic analgesics Autonomic nervous system Anti seizure drugs Migraines Antidepressants Antianxiety agents Agents for insomnia Antidiabetics Antilipemics Antihypertensives Diuretics Nitrates • • • • • • • • • • • • • • Antiplatelets and anticoagulants Antiasthmatics BPH Erectile dysfunction Dementia Parkinson’s disease and schizophrenia Dyspepsia, GERD and PUD Antiemetics IBD IBS Osteoporosis Gout OTC drugs Appendix I & II A Process for Rational Prescribing (your new best friend) Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, U of Ottawa March 2013 Objectives • To promote an efficient process for selecting optimal drug therapy for patients • To promote a process for applying population level evidence based medicine to individual patients. A Structure Requires Process To prescribe or not to prescribe? That is the question… • Rational prescribing requires a process for selecting therapy: (in order) 1. 2. 3. 4. Efficacy Toxicity Cost Convenience 1. Efficacy – Ask About… 1. Which HARD Outcomes a) Mortality benefit? b) Morbidity benefit? 2. Which SURROGATE Outcomes • Clinically relevant? 3. THEN “What is the quality of the evidence to prove this?” • • • • Meta-analysis? Randomized Controlled Trial? Case series? Anecdotal evidence? Efficacy • If there is no efficacy, why waste your time on the potential toxicity, cost and inconvenience of a drug? • If there is proven efficacy at the population level, then balance this against the potential toxicity to the individual. 2. Toxicity – Ask About… Bothersome Severe Common Rare Not legal Who cares • Age? • • Newer agents Older agents = = Less Safety Data More Safety Data 3. Cost – Ask About… • Patient cost vs Societal cost • Covered under provincial formulary? – Covered under private plans? 4. Convenience – Ask About… • What is the likelihood of compliance? 1. Frequency of administration? – Daily vs QID? 2. Special restrictions? (eg. bisphosphonates) – PO vs IV? – Home vs Office vs Hospital therapy? 3. Many interactions? 4. Special monitoring requirements? A simple example: Metformin Januvia® VS Why is Metformin first line therapy? Efficacy 1. HARD Outcomes – Mortality benefit » Metformin – reduction in CV events (UKPDS-34 trial) – Morbidity benefit » Metformin – reduction in microvascular complications 2. SURROGATE Outcomes a) Hgb-A1c reduction a) Metformin ~ 1% - 2% b) Januvia® ~ 0.5% - 0.8% b) Insulin Sparing Effects a) Metformin Toxicity • Metformin – Very rare risk of lactic acidosis? • 0.03 cases / 1000 pt-yrs (~ 50% fatal) • Never clearly implicated – GI upset / diarrhea • Start low, go slow! – B12 / folate deficiency / anemia (6 - 8/100) • Reduced absorption – easy to supplement – Anorexia • usually transient • Januvia® – ?Unknown - too new • ?Pancreatitis – Too few patients examined – GI upset – edema – ?elevated risk of infection? Cost & Convenience • Metformin • Januvia® – Ontario Drug Benefit: – Ontario Drug Benefit: • $ 0.0587 / tab • Covered by ODB • $ 2.8050 / tab • Covered by ODB – Rxfiles 2012: • ~ $33 / 100 days – QD to TID po – Rxfiles 2012: • ~ $315 / 100 days – Once daily po Topics to be covered in this lecture • • • • • • • • • • • • • • • Antibacterials Antimycobacterials Antifungals Narcotic analgesics Autonomic nervous system Anti seizure drugs Migraines Antidepressants Antianxiety agents Agents for insomnia Antidiabetics Antilipemics Antihypertensives Diuretics Nitrates • • • • • • • • • • • • • • Antiplatelets and anticoagulants Antiasthmatics BPH Erectile dysfunction Dementia Parkinson’s disease and schizophrenia Dyspepsia, GERD and PUD Antiemetics IBD IBS Osteoporosis Gout OTC drugs Appendix I & II Antibiotic Review (80% of the knowledge, 80% of the time) Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, U of Ottawa March 2013 Objectives • Review clinically relevant pathogens in human disease in an ambulatory care setting • Review antibiotic classes and spectra of activity – Focus on bread and butter examples of each • Review treatment recommendations for common infections in primary care Process 1. Map the Bugs – “Know your enemy” 2. Map the Drugs – “Save your ammo” 3. Map the Battlefield Part 1 - Map the (Clinically Important) Bugs “Know your enemy” Gram Negative Aerobic β-Lactamase Negative Cocci (spheres) Bacilli (rods) Gram Positive Anaerobic β-Lactamase Positive Map the Bugs Aerobes Anaerobes Gram Positive Gram Negative Gram Positive Gram Negative Cocci Bacilli Cocci Bacilli Cocci Bacilli Cocci Bacilli b-L[+] b-L[-] b-L[+] b-L[-] 1 2 3 4 b-L[+] b-L[-] b-L[+] b-L[-] 5 6 7 8 b-L[+] b-L[-] b-L[+] b-L[-] b-L[+] b-L[-] b-L[+] b-L[-] 9 10 11 12 13 14 15 16 Anaerobes Above & below the diaphragm Oral • Simple organisms • Easily handled by penicillins (beta-lactams) – Eg. Actinomyces Bifidobacterium Fusobacterium Lactobacillus Peptococcus Peptostreptococcus Propionibacterium etc Gut • Approx the same, except: • Human pathogens: • Bacteroides fragilis (B.frag) • Clostridium difficile (C.diff) – More virulent bugs requiring ‘bigger guns’… Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci Bacilli Above & Below diaphragm Bacilli B.Frag C.Diff b-L[+] b-L[-] b-L[+] b-L[-] 1 2 3 4 b-L[+] b-L[-] 5 6 b-L[+] b-L[-] 7 8 9 . Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci Bacilli Below diaphragm Bacilli B.Frag C.Diff b-L[+] b-L[-] b-L[+] b-L[-] 1 2 3 4 b-L[+] b-L[-] 5 6 b-L[+] b-L[-] 7 8 9 . Gram[+] Bacilli • Not usually pathogenic – Major Exception: Listeria monocytogenes • Listeriosis – enteritis, sepsis, meningitis +/- encephalitis Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci Bacilli Below diaphragm Bacilli B.Frag C.Diff (Listeria) β-L[+] β-L[-] 1 2 b-L[+] b-L[-] 3 4 β-L[+] β-L[-] 5 6 7 . Gm[-] Cocci • Not usually pathogenic – Major Exceptions: • Neisseria gonorrhea • Neisseria meningitidis and • Moraxella catarrhalis – (formerly thought to be a type of Neisseria) Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci (Neisseria & Moraxella) β-L[+] β-L[-] 1 2 Bacilli (Listeria) Below diaphragm Bacilli B.Frag C.Diff β-L[+] 3 β-L[-] 4 5 . β-Lactamase Enzymes • First penicillinase described in 1940’s even before penicillin was clinically available. • Most bugs produce some type of β-lactamase enzyme that destroys β-lactam antibiotics (pen’s, ceph’s, carbapenems) – Gm[+] cocci & β-lactamase [-]: only Group A strep give Penicillin Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Cocci (Neisseria & Moraxella) Bacilli (Listeria) β-L[+] β-L[-] 1 (GrpAStrep) Below diaphragm Bacilli B.Frag C.Diff β-L[+] 2 β-L[-] 3 4 . Map the Bugs Anaerobes Aerobes Gram Positive Gram Negative Cocci Below diaphragm Bacilli B.Frag C.Diff β-L[+] 1 both β-L[+]&[-] 2 3 . Map the Clinically Important Bugs Atypicals Aerobes Gram [+] Gram [-] Cocci Bacilli 1 2 1. Legionella pneumonia 2. Chlamydia pneumonia 3. Mycoplasma pneumonia 3 . Anaerobes (esp. Gut organisms) Eg. C-Diff & B-frag 4 . 1 - Gram [+] Cocci Staphylococcus • S. aureus – Methicillin resistant (MRSA) – Methicillin sensitive (MSSA) • S. epidermidis – Methicillin resistant (MRSE) – Methicillin sensitive (MSSE) – Skin commensal – Rarely pathogenic Streptococcus • Group A (pyogenes) (β-Lact[-]) • Group B (agalactiae) • Neonates, v. elderly, obstetrics • S. pneumonia etc. etc. Enterococcus • (Formerly thought to be ‘Strep D’) • E. faecalis • E. faecium 2 - Gram [-] Bacilli • • • • • • Easy to Kill Proteus mirabilis Escherichia coli Klebsiella pneumonia Salmonella Shigella Haemophilus influenza • • • • • Hard to Kill Serratia Pseudomonas Acinetobacter Citrobacter Enterobacter – (Moraxella catarrhalis) (actually a Gm[-] coccus) PEcKSS-HiM SPACE bugs Gram Negative vs Gram Positive Gm[-]: red on stain. (ie. Don’t retain stain) Gm[+]: blue-purple on stain; Gm[-]: must pass through pores Gm[+]: molecules < 100kDa pass easily. Gm[-]: b-lactamases concentrated in periplasmic space Gm[+]: b-lactamases diffuse outside cell; Atypicals: • Mycoplasma pneumo • Chlamydia pneumo • Legionella pneumo Map the Bugs • Gram positive aerobes: – Cocci Summary Anaerobes: • Oral • Gut – Bfrag & Cdiff • Gram negative aerobes: – Bacilli • Staph – Aureus » MRSA (~8-10%) » MSSA – Epiderimidis » MRSE (~65%) » MSSE • Easy to Kill – PEcKSS (Proteus, Ecoli, Klebsiella, Salmonella, Shigella) – HiM (H.flu and Moraxella (actually a Gm[-]coccus)) • Hard to Kill – SPACE bugs (Serratia, Pseudomonas, Acinetobacter, Citrobacter, Enterobacter) • Strep – – – – Group A strep (pyogenes) Group B strep (agalactiae) Strep Viridans Strep pneumo etc. • Enterococcus – Faecalis – Faecium – Bacilli • Listeria – Cocci • Neisseria – gonorrhaea – meningitidis • Moraxella catarhallis Part 2 - Map the Drugs (Save your Ammo) Map the Drugs • Arms race! – Remember: “Bigger guns breed higher walls” • Older drugs tend to be simpler drugs – More narrow spectrum – Broad spectrum drugs breed resistance – Superbugs develop • MRSA, VRE, ESBL, etc • Older drugs have more safety data – Tend to be less toxic – Learn their history – Learn their pharmacology Part 2 - Map the Drugs “Save your Ammo” Fluoroquinolones Penicillins Tetracyclines Aminoglycosides Vancomycin Macrolides Carbapenems Cephalosporins Clindamycin Metronidazole Antibiotics – Mechanisms of Action From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Beta-Lactams - Penicillins Penicillin Anti-Staph Anti-Strep Amoxicillin / Ampicillin (po) (iv) Amox + Clavulanic acid Cloxacillin / Methicillin (clinic) (lab) Beta-Lactams - Cephalosporins – Cephalexin (Keflex™)(or Cefadroxil) (po) – Cefazolin (Ancef™) (iv) • 2nd Generation – Cefuroxime (po & iv) • 3rd Generation – Ceftriaxone, Cefotaxime, Ceftazidime (iv) – Cefixime (Suprax™) (po) • 4th Generation – Cefepime (iv) Increasing Gram[-] coverage • 1st Generation Beta-Lactams – Other (FYI) (IV only, inpatient use only) • Piperacillin (plus tazobactam) – big gun, tazo = suicide substrate, like clavulanic acid • Carbapenems – Meropenem – Imipenem – Ertapenem • Monobactams – Aztreonam Broad spectrum, big gun antibiotics that cover Gm[+], both easy and hard to kill Gm[-] bugs, even some anaerobes. Antibiotics – Mechanisms of Action From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Fluoroquinolones • 2nd generation – Ofloxacin – Ciprofloxacin – Norfloxacin • 3rd generation – Levofloxacin • 4th generation – Moxifloxacin • Covers: strep & Gm[-]’s – PEcKSS-HiM & SPACE bugs • Ofloxacin • Ciprofloxacin – Anti-pseudomonal – the only PO option! – Norfloxacin • Same spectrum as Cipro (even anti-Pseudomonal) – but only for cystitis UTI. • Concentrates in the G.U. system only • N.B. Not good enough for pyelonephritis or systemic infection Fluoroquinolones • The “Respiratory FQs” – Concentrate in alveolar macrophages – Greater than serum concn 1. Levofloxacin – the more active Lenantiomer of Ofloxacin – Renal clearance 2. Moxifloxacin – Hepatic clearance • Enhanced coverage of: 1. Strep pneumo 2. Oral Anaerobes 3. Atypicals – N.B. only Moxi cover B.frag – Neither covers C.diff • (Both will cover Clostrium non-difficile strains) • Both have 100% oral bioavailability – Therefore PO = IV dose Antibiotics – Mechanisms of Action From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Macrolides • Coverage of: – Atypicals, Strep pneumo, & Hi.M. (Hflu & Mcat) • So, good for respiratory infections! – N.B. But doesn’t cover PEcKSS or SPACE bugs • Erythromycin – Efficacy: Poorer coverage of H.flu, MSSA – Toxicity: • Prokinetic – diarrhea! • Worse for QTc prolongation – Convenience: QID dosing • Clarithromycin – Better Hflu &MSSA coverage – Less QTc prolongation vs E – Shorter half-life vs Azithro • BID dosing x 7-10days • New daily ‘XL’ formulation • Azithromycin – An azalide, (not a macrolide) • Same spectrum of activity • Less QTc prolongation vs E & C! – Long t1/2 – QD dosing x 5d • BUT can breed resistant S.pneumo (since below [MIC] for long periods of time) Antibiotics – Mechanisms of Action From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Aminoglycosides 1. Gentamicin 2. Tobramycin – Reserved for Pseudomonas aeruginosa 3. Amikacin • Efficacy: excellent Gm[-] • Toxicity: – Nephrotoxicity – Ototoxicity – Less now with daily dosing • Cost: • All excellent Gram[-] coverage: – PEcKSS-HiM and SPACE bugs – Cheap, old meds • Convenience – Now Once daily IV/IM Pharmacodynamics Relationship between Abx Concentration & Effect Concentration Dependent Killing • Higher the peak, better the kill • i.e. Ratio of peak drug concentration and M.I.C. determines rate of kill. • Eg. FQs, AGs Log [Conc] Time Dependent Killing • Time over MIC matters • i.e. Independent of peak concentration. Determined by length of time over MIC • Eg. B-lactams (Pen, Ceph etc) Log [Conc] Peak MIC MIC Time (h) Time (h) Pharmacodynamics Relationship between Abx Concentration & Effect Concentration Dependent Killing • With renal impairment: – Maintain the peak, lengthen the interval – This ensures good rate of killing while allowing enough time to eliminate the drug and avoid toxicities – For eg: • Higher the peak, better the kill • i.e. Ratio of peak drug concentration and M.I.C. determines rate of kill. • Eg. FQs, AGs Log [Conc] Peak Log [Conc] Peak MIC Time (h) MIC Time (h) • If CrCL = 90mL/min Levofloxacin 750mg q24h po • If CrCL = 30mL/min – Levofloxacin 750mg q48h po Pharmacodymamics Bactericidal vs Bacteriostatic • Bactericidal Abx – – – – – – B-lactams (Pen, Ceph) Aminoglycosides (AGs) Fluoroquinolones (FQs) Rifampin Metronidazole Vancomycin • Bacteriostatic Abx – – – – Tetracyclines Macrolides Clindamycin Chloramphenicol Rarely a clinically important characteristic, unless the patient is immunocompromised or the risk of death with delayed/incorrect therapy is high. Combination Therapy • Why? – Broaden spectrum • (eg. Mixed infection) – Synergistic activity for hard to kill bugs • (eg. Enterococcus or pseudomonas) – Prevent resistance • (eg. TB) – Reduce dose and side effects Map the Drugs Pharmacology Summary • Many antibiotic classes – Beta-lactams generally safest agents. • Even at high doses – Some have overlapping mechanisms of action – Avoid combining similar mechanisms of action • Competing effects may reduce effectiveness of one agent • Eg. Penicillins + vancomycin – cell wall synthesis inhibitors • Eg. Tetracyclines + aminoglycosides –protein synthesis inhibitors via 30-S subunit of the ribosome Map the Drugs – Summary For: TB, MRSA For: skin, dental infx (staph, strep, & anaerobes) From: http://commons.wikimedia.org/wiki/File:Antibiotics_Mechanisms_of_action.png Accessed Dec 28/12 Part 3 – Map the Battlefield Map the Battlefield Rational Prescribing Individual Population 1. Efficacy 1. Efficacy – Could be reduced, BUT: – Empiric tx still effective if it is well chosen – Maintained long term with lower resistance rates 2. Toxicity • (Lower risk infections, properly dosed, clinically stable, true indication etc.) – Reduced since lifespan of older drugs is maintained 3. Cost 2. Toxicity – Reduced with narrow spectrum tx 3. Cost – Reduced with older tx 4. Convenience – Usually less convenient VS. – Reduced insurance costs, economic losses, hospital costs dealing with superbugs 4. Convenience Map the Battlefield Map the Battlefield Otitis media: S.pneumo, Hi,M Conjunctivitis: viral – no tx (Amox +/- Clav, Cef2, Septra) Sinusitis: viral – no tx AECOPD: S.pneumo, Hi,M Oral anaerobes: abscess drainage – no tx (Amox +/- Clav, Cef2, Septra) (Amox 2g – pre dental sx?) C.A.P: S.pneumo, atypicals – (Amox, Macrolides (Clarithro/Azithro)) CAP+comorb./risk factors, or NHAP: also HiM bugs (Combine AmoxClav or Cef2 + Macrolide (or use FQ)) Cellulitis: MSSA, S.pneumo – (Clox, Cef1, Clinda) Pyelonephritis: PEcK – (Septra, Amox/Clav, FQ (not Norflox) UTI (Cystitis): PEcK – (Septra, Macrobid, Amox, Norflox) Pharyngitis: viral – no tx (Group A Strep – Pen VK) Bronchitis: viral – no tx Skin abscess: drainage – no tx H.pylori: triple po tx PPI + (Clarithro +/Amox +/- Metro) Cdiff / Bfrag: Metro / po Traveller’s Diarrhea: (80% bacterial): EcSS, Vanco (camphlyobacter) - Septra, FQ, (Azithro) Map the Battlefield Penicillin (Group A Strep, oral anaerobes, Neisseria) Amoxicillin / Ampicillin (Strep & Enterococcus plus Easy-to-Kill Gm[-](ie. PEcKSS)) Cloxacillin (Staph aureus, Staph epi) Amox/Clav (Vancomycin) (for Strep & Entero & PEcKSS-HiM) (H.flu & Moraxella can be ~35% amox resistant) (for MRSA / MRSE) (~8-10% / ~ 65% resistant) Beta-Lactams - Cephalosporins – Cephalexin (Keflex™) or Cefadroxil (po) – Cefazolin (Ancef™) (iv) • 2nd Generation – Cefuroxime (po & iv) • 3rd Generation To boost: for PEcKSS-HiM (same as Amox/Clav) SPACE bugs: The Big Guns – Ceftriaxone, Cefotaxime, Ceftazidime (iv) – Cefixime (Suprax™) (po) • 4th Generation – Cefipime (iv) Increasing Gram[-] coverage • 1st Generation MSSA and Strep & PEcKSS (same as Amox) N.B. never Enterococcus! SPACE bugs • The Big Guns: – 3rd and 4th generation Cephalosporins – Carbapenems (Meropenem) – Piperacillin/Tazobactam – Aminoglycosides (Gentamicin, Tobramicin) – Fluoroquinolones (Levofloxacin, Moxi, Cipro) Reserved for Pseudomonas • Ciprofloxacin (FQ) – The only PO agent! – (Use Norfloxacin for UTI if a FQ is needed) • • • • • Ceftazidime (Cef3) Cefipime (Cef4) Tobramycin (AG) Piperacillin/Tazobactam Meropenem Need for Bigger guns • There is a higher risk of Gram negative SPACE bugs with: – More risk factors / comorbidities – COPD, HIV, Diabetes, CKD etc – More institutionalized settings • Community Retirement Home Nursing Home Hospital ward ICU ventilated pt in ICU. Map the Battlefield • PEN – for Group A Strep, oral anaerobes, Neisseria • ?What to do for Strep/Entero? – Amox po / Amp iv (also good for PEcKSS) – How to boost? Amox/clav (for HiM-PEcKSS) • ?What to do for Staph? – Clox (MSSA, MSSE); Else Vanco (MRSA, MRSE) • What about Cef1? (cephalexin / cefadroxil po or cefazolin iv) – Maps to Amox/Amp for PEcKSS and strep • N.B. NOT Enterococcus (Cef’s never cover enterococcus!) – How to boost? Cef2 (cefuroxime) for HiM-PEcKSS • What about SPACE bugs? – FQs, AGs, Cef3, Cef4, Pip/Tazo, Meropenem) – Reserved for Ps aureginosa:(cipro, tobra, ceftazidime, cefipime, pip/tazo, meropenem) • What about gut anaerobes? (Metro/PO Vanco) • What about atypicals? (Macrolides, Tetracyclines (doxy)) • Where does Septra fit? (with Amox/Clav and Cef2) Antibiotics contraindicated in pregnancy (category X) • • • • • • • • • Tetracyclines (also in children < 9 y.o.): are incorporated into fetal skeleton/unerupted teeth Fluoroquinolones Erythromycin estolate (may cause toxic liver reaction), clarithromycin TMP: in 1st trimester because it is a folate antagonist Sulfonamides: last trimester or if delivery is imminent because they interfere with the bile conjugating mechanism of the neonate and may displace bilirubin bound to albumin which may lead to jaundice and kernicterus Nitrofurantoin (during labor and delivery only): can affect glutathione reductase activity and hence can cause hemolytic anemia (analogous to the problems it causes in patients with glucose-6-phosphate dehydrogenase deficiency) and hemolytic crises have been documented in newborns and fetuses Aminoglycosides: nephrotoxic and ototoxic to the fetus High (>2 grams) single dose metronidazole Chloramphenicol (at term or during labour): limited glucuronidating capacity of the newborn’s liver Ref: Marc Riachi, RPh Antibiotics Preferred in Pregnancy • Penicillins • • • • • • Including those in combination with ß-lactamase inhibitors (clavulanic acid, sulbactam, and tazobactam) Cephalosporins Erythromycin base Azithromycin Clindamycin Metronidazole • Ref: Marc Riachi, RPh (regular dose 250-500 mg BID) Summary • This is far from an exhaustive review • Some parts have been highly simplified for use in clinical practice • Some memorization is needed with regular review of the material to retain this knowledge • Doing so will allow you to choose empiric antibiotics with greater comfort in difficult situations and unfamiliar settings. Penicillin: BL-ve aer obic GPC oral anaerobes N.meni ngitidis Lacking Activity Vs. Atypical Organism s BL+ Ae robic GPC Ae robic GNB Gut anae robe s (B. fragilis) 95% of Staph. s pe cies are BL +ve MRSA(7%)/ M RSE (>65%) MSSA/MSSE TMP/SMX Clindam ycin Easy to Kill GNB Macrolide s: Erythromycin Clarithromycin Azithromycin TMP/SMX Tetracyclines Res piratory Fluoroquinolones Gatif loxacin Levof loxacin Moxif loxacin Vancom ycin Rifam pin Fus idic Acid Linezolid Syner cid Me tronidazole Am picillin/Am oxicillin: HiPEELSS Isoxazoyl PCNs : e g. Cloxacillin, Nafcillin 1st Ge ne ration Ce phs: (Cefazolin iv / Ce phalexin po) PEcKSS Second Generation Cephs Am oxicillin/Clavulanic acid Am picillin/Sulbactam Ce furoxim e Ce furoxim e axetil Ce faclor B. fragil i s H. i nfluenza e Ce fote tan Ce foxitin Difficult to Kill GNB 3rd Generation Ce phs. Ce ftriaxone Ce fotaxim e Ce ftazidim e 4th Ge ne ration Ce phs: Ce fe pim e No Ce phalos porin cove rs : MRSA / M RSE enterococcus sp. Listeri a monocytogenes AM Gs: Ge ntam icin Tobram ycin Am ik acin Piper acillin: (P.aerugi nosa , Enteroba cter) Never Us e Alone ! Piper acillin/Tazobactam Ticarcillin/Clavulanic Acid FQs : ciprof loxacin ofloxacin norf loxacin Carbape ne m s: Im ipe nem Me rope ne m Adapted from : Winslade N. On Continuing Pr actice 1990-1, volum es 17-18. Prepared By: Sandr a A.N. Tailor, Pharm .D. Clinical Coor dinator - Infe ctious Dis ease s Sunnybr ook Health Scie nce Centre Depar tm e nt of Pharm acy 11/11/02 TB drugs Adapted from: Marc Riachi, RPh Mycobaterium tuberculosis The Consumption • Mostly latent, asymptomatic infection (90-95%) – – – – Activation risk ~ 10% Usually pulmonary; can occur anywhere Spreads via air droplet One third of world population infected! • Europe:, TB rates rose from 1600s to peak in the 1800s (caused ~25% of all deaths) • Organism has "waxy" hard to penetrate cell wall – Acid-fast bacilli – Combinations of drugs needed to treat • Slow growing – Therefore requires extended treatment period • Treatment: – Multiple side effects = reduced compliance by patient = further emergence of resistant strains – MDR, XDR strains Adapted from: Marc Riachi, RPh Available antimycobacterials • First-line: – Isoniazid (INH) – Rifampin (RIF) or Rifampicin (RMP) – Pyrazinamide (PZA) – Ethambutol (ETB) • Second-line: – Amikacin – FQs (Ciprofloxacin / Levofloxacin / Moxifloxacin) – Clarithromycin / Azithromycin Ref: Marc Riachi, RPh Treatment - Active Pulmonary TB • “4 drugs x 2 months, then 2 drugs x 4 mo” • (N.B. 2x/weekly dosing must be D.O.T.) Ref: PHAC. Canadian Tuberuclosis Standards, 6th Ed. 2007 p. 130 http://www.phac-aspc.gc.ca/tbpc-latb/pubs/pdf/tbstand07_e.pdf Access March 14, 2013. Treatment – Latent TB • INH – monitor LFTs – Hepatitis (rare < 20y.o.; >2% in >50y.o.) – Drug interactions! • RIF – GI toxicities, major drug interactions! – Huge inducer of cytochrome P450 Ref: PHAC. Canadian Tuberuclosis Standards, 6th Ed. 2007 p. 148 http://www.phac-aspc.gc.ca/tbpc-latb/pubs/pdf/tbstand07_e.pdf Access March 14, 2013. Which agents to use in active disease? • Pulmonary or extrapulmonary disease: – INH+RIF+PZA+ETB • If resistant to INH: – RIF+PZA+ETB (+FQ if severe) • If resistant to RIF: – INH+PZA+ETB+FQ • if resistant to INH and RIF: – PZA+ETB+FQ+amikacin • If resistant to INH, RIF and PZA or ETB – ETB (or PZA)+FQ+amikacin+two 2nd line agents Ref: Marc Riachi, RPh Anti-fungals Adapted from: Marc Riachi, RPh Drug info • • INH (inhibits formation of fatty acids found in the cell wall): – Bactericidal; penetrates cavitations – Hepatotoxicity (↑ with alcohol & rifampin) monitor LFTs – peripheral neuropathy (give vit B6) – GI symptoms, skin rash – ↑ phenytoin, carbamazepine & benzodiazepine blood levels RIF (inhibits mRNA synthesis): – Bactericidal; penetrates cavitations – Hepatotoxicity (↑ with alcohol) monitor LFTs – GI symptoms, skin rash – Pancytopenia – Colours urine, feces, saliva, tears orange may permanently stain contact lenses – Induces CYP450 Ref: Marc Riachi, RPh • • PZA (may inhibit mycobacterial metabolism): – Bactericidal in acid environment (in macrophages) – Hepatotoxicity (↑ with alcohol & rifampin) monitor LFTs – Hyperuricemia monitor uric acid – GI symptoms and arthralgias ETB (may inhibit cell wall synthesis): – Bacteriostatic – GI symptoms, hyperuricemia – Ocular toxicity and change in color perception monitor at high doses Antifungals • Topical • Oral – Azole anti-fungals • • • • • • Itra- (Sporanox), flu- (Diflucan), vori-, posaketoconazole (Nizoral) active vs. yeast and dermatophytes – Terbinafine (Lamisil) • active vs. yeast and dermatophytes – Nystatin • active vs. yeast only Ref: Marc Riachi, RPh – Ciclopirox • (cream, lacquer, shampoo), – nystatin • (cream, pv, oral suspension), – clotrimazole • (cream, pv), – miconazole • (cream, pv), – ketoconazole • (cream shampoo), – terbinafine • (cream, spray), – tolnaftate • (powder suitable for skin folds) • Injectables – usually require I.D. consult Which agents to use? • Onychomycosis: – oral terbinafine, oral itraconazole, ciclopirox lacquer (use lacquer only for mild distal form; expensive) • Fungal skin: – topical clotrimazole, topical miconazole, topical terbinafine, topical ketoconazole. Nystatin is ineffective vs. dermatophytes. Candidal skin infections respond to nystatin. Use topical azoles for tinea versicolor (not terbinafine). • Seborrheic dermatitis: – topical ciclopirox, ketoconazole • Oral candidiasis: – Oral nystatin swish and swallow (not absorbed from GI tract). Oral fluconazole. • Vulvovaginal candidiasis: – topical azoles, po fluconazole one dose (now available without a prescription), boric acid pv suppositories (very irritative) • Diaper rash: – Topical nystatin, clotrimazole, miconazole, or ketoconazole. Ref: Marc Riachi, RPh • • Drug info Terbinafine po: – Very active vs dermatophytes – headache, GI diarrhea, dyspepsia, abdominal pain – taste disturbance (may persist post treatment) – CYP2D6 inhibitor: • Decreases formation of active metabolites of tamoxifen • May ↓ breakdown of TCA’s, fluoxetine, paroxetine, fluvoxamine, sertraline, tamsulosin, mirtazapine, haloperidol, some beta blockers Azole antifungals po: – Itraconazole and ketoconazole particularly are strong inhibitors of CYP3A4 and so many drug interactions. Also hepatotoxic. Ketoconazole > itraconazole > terbinafine wrt hepatic toxicity. Itra may worsen heart failure symptoms. Ketoconazole is rarely used and is poorly tolerated; anorexia, nausea, vomiting high doses, and effects sexual function/sex hormones and steroidogenesis. – Fluconazole is considered a moderate inhibitor of CYP3A4 and so less clinically important drug interactions. Strong CYP2C9, 2C19 inhibitor. QT prolongation with amiodarone, clarithromycin, TCA’s. Bioavailability of PO similar to IV; use PO if possible. Ref: Marc Riachi, RPh Hypertension and BP Meds (The ABCD’s of HTN) Dr Roland Halil, BSc(Hon), BScPharm, ACPR, PharmD Pharmacist, Bruyere Academic FHT Assistant Professor, Dept Family Medicine, U of Ottawa March 2013 Objectives • List first line classes of medication for the treatment of essential hypertension • Explain how co-morbid indications may change your choice in therapy • Apply a rational approach in selecting therapy • Understand the dosing, monitoring and titration of key examples from each class of medication Rational Prescribing • Rational prescribing requires a process for selecting therapy: (in order) 1. 2. 3. 4. Efficacy Toxicity Cost Convenience A A B C D ARB ACEinh B-blockers CCB Diuretics (DHP-type) (Thiazide type) Angiotension Receptor Blocker Angiotensin Converting Enzyme Inhibitor Beta-Blocker Calcium Channel Blocker (dihydropyridine type) -sartan -pril -olol -dipine Losartan Valsartan Candesartan Etc Ramipril Enalapril Perindopril Etc Bisoprolol Metoprolol Atenolol Etc Amlodipine Nifedipine Felodipine Etc Chlorthalidone Hydrochlorothiazide Indapamide Etc Reduced sympathetic outflow, and heart rate Relaxation of coronary & peripheral arterial smooth muscle (not AV node!) Inhibits Na+ & Cl- reabsorption in the corticaldiluting segment of the ascending loop of Henle = diuresis. Reduction in systemic vascular resistance 1st line 1st line Blocks conversion of AT1 to ATII (ACEinh) or blocks ATII receptors (ARB) = Inhibition of vasoconstriction, aldosterone, catecholamine, and arginine vasopressin release, water intake, and hypertrophic responses (b1 receptor – in heart) (cardioselective ~ A-M) (b2 receptor – in lungs) (Non-selective ~ N-Z) (“one heart; two lungs”) Efficacy: 1st line 1st line 1st line (< 65y.o.) A A B C D Toxicity: Toxicity: Toxicity: Toxicity: Hypotension HyperK+ Acute renal failure (ARF) Angioedema Hypotension Bradycardia Bronchoconstric tion (in brittle asthmatics with noncardioselective bbl’s) Hypotension Edema Orthostatic hypotension Hypotension HypoNa+ HypoK+ ARF Monitor: SCr, K+, BP Monitor: BP, HR, RR Monitor: SCr, lytes, BP Cost: Generic - $$$ ODB covered Cost: Generic - $ ODB covered Cost: $ ODB covered Cost: Generic: $$$ ODB covered Cost: ¢ ODB covered Convenience: QD Losartan 25mg to 100mg Convenience: QD Ramipril 2.5mg to 10mg Convenience: QD Bisoprolol 2.5mg to 10mg Convenience: QD Amlodipine 2.5mg to 10mg Convenience: QAM Chlorthalidone 25mg Choosing Therapy • If efficacy (#1), cost (#3) and convenience (#4) are all more or less equivalent: – Choose based on potential Toxicities (#2) – Tailor the meds to the individual patient! • Evidence of efficacy is population based • Toxicities are individual. • Some combos are additive others synergistic BP lowering – Rarely clinically relevant – Can choose between groups A or B plus C or D (synergistic) • N.B. Choice will also be guided by various comorbidites Comorbidities Indication ARB ACEinh B C HTN (ALLHAT) MI (HOPE trial) CHF (CONSENSUS, SOLVD, ATLAS) DM2 (HOPE) (IDNT, IRMA-2, RENAAL) CVA (HOPE, PROGRESS) (LIFE, SCOPE, MOSES) PVD (HOPE) Afib D (VALIANT) (CAPRICORN, BHAT) (MERIT-HF, CIBIS II, COPERNICUS) (ALLHAT, PROGRESS) (Diltiazem) Second Line Therapy • What if you have used all available 1st line options? • 2nd line options: – – – – – – – Alpha blockers Spironolactone Hydralazine Nitrates Clonidine Beta-blockers (> 65 y.o.) etc. • ~ Equivalent efficacy – choose based on potential toxicity, cost or convenience factors. • Ensure that you balance these factors in their order of importance. Second Line Therapy • Alpha blockers – Eg. Terazosin, Prazosin, Doxazosin – Toxicity: Risk of orthostatic hypotension – Cost: cheap, generic – Convenience: only QD • Good 1st choice of 2nd line tx • Dual treatment of BPH & BP if also needed in male patients • Spironolactone – Efficacy: mortality benefit in late stage CHF (NYHA class III or IV) – Toxicity: risk of hyperK+ • esp with ARBs or ACEinh’s – Cost: cheap generic – Convenience: only QD • Hydralazine – MOA: direct vasodilation of arteries – Toxicity: orthostatic hypotension – Cost: cheap, generic – Convenience: QID dosing • Nitrates – eg. ISDN, ISMN, NTG – MOA: smooth muscle vasodilation of vasculature (veins > arteries); – Toxicity: headache, orthostatic hypotension, dizziness – Cost: cheap/ generic – Convenience: BID- QID dosing; Process 1. Start first drug 2. Increase to moderate dose 3. Monitor for efficacy (BP) and toxicity • If close to target: • Dose response curves – Flatten at top half – Less bang for your buck BP – increase dose • If far from target: – start new drug mg Comments, Questions & Requests? • rhalil@bruyere.org • Monday & Fridays: – 613-230-7788 ext 238 • Tuesday, Wednesday, Thursday: – 613-241-3344 ext 327 • Twitter: @Roland Halil, PharmD