Neurodevelopmental and Oral-feeding Outcomes for Infants Born
advertisement

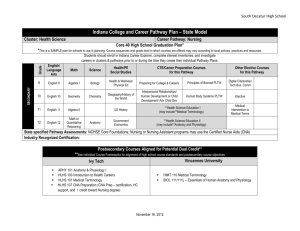
Neurodevelopmental and Oral-feeding Outcomes for Infants Sharon Sables-Baus, PhD, RN, MPA, PCNS-BC Associate Professor, University of Colorado College of Nursing/ School of Medicine, Department of Pediatrics Table of Contents Single-ventricle Physiology, Background (I) Definitions (A) Incidence (B) Diagnosis (C) HLHS: A Single-ventricle Defect (II) Anatomy of Hypoplastic Left-heart Syndrome (A) Physiology of Hypoplastic Left-heart Syndrome (B) Surgical Repair of Hypoplastic Left-heart Syndrome (C) Impact of Single-ventricle Defects (III) Neurodevelopmental Issues (A) Subsequent Feeding-related Outcomes (B) Neurodevelopmental Research Foci (C) Studying the Impact of Caregiving: Sables-Baus et al, 2013 (IV) Care Paradigm Utilized in Study (A) Care Environment Utilized in Study (B) Study Metrics/Methods/Objectives (C) Study Results, Objective by Objective (D) Implications for Future Research (E) (I) Single-ventricle Physiology, Background (A) Definition (B) Incidence (C) Diagnosis (I) Single-ventricle Physiology, Background (I.A) Definitions Examples of Single-ventricle defects: • Tricuspid atresia • Double-outlet left ventricle • Some heterotaxy defects • Hypoplastic left-heart syndrome (I) Single-ventricle Physiology, Background (I.B) Incidence (I) Single-ventricle Physiology, Background (I.C) Diagnosis Examples of Symptoms: • Blue/purple tint to lips, skin, and nails (cyanosis) • Difficulty breathing and/or feeding • Lethargy (sleepiness/unresponsiveness) A. Anatomy of Hypoplastic Left-heart Syndrome B. Physiology of Hypoplastic Left-Heart Syndrome C. Surgical Repair of Hypoplastic Left-heart Syndrome (II) HLHS: A Single-ventricle Defect (II.A1) Anatomy of Hypoplastic Left-heart Syndrome (HLHS) 1. HLHS—1/5000 babies, 1% of congenital heart disorders 2. Left ventricle (pumping chamber)-small 3. Mitral and/or aortic valves—narrow, blocked, or not formed at all 4. Aorta—often small (hypoplastic) (II) HLHS: A Single-ventricle Defect (II.A2) Anatomy of Hypoplastic Left-heart Syndrome (HLHS) (II) HLHS: A Single-ventricle Defect (II.B) Physiology of HLHS 1. Deoxygenated blood flows into right atrium, through tricuspid valve, into right ventricle 2. From right ventricle, blood pumped up to lungs, receives oxygen 3. Oxygenated blood flows from lungs into left atrium—unable to pass into left ventricle (valve blocked or narrowed) www.ihm.org.uk 7. Gradually, sicker; ultimately, dies 6. When ductus arteriosus closes, no oxygenated blood flowing in baby’s body 5. While ductus arteriosus still patent, blood passes from pulmonary artery into aorta, then, around body 4. Oxygenated blood passes through hole between ventricles, mixes with deoxygenated blood in right ventricle, follows normal path to lungs (II) HLHS: A Single-ventricle Defect (II.C) Surgical Repair of HLHS (II.C1) Norwood (II.C2) Glenn (II.C3) Fontan (II) HLHS: A Single-ventricle Defect (II.C) Surgical Repair of HLHS (II.C1a) Norwood Procedure Aim (ii) of the Norwood: To provide blood flow to lungs through Gore-Tex passage (shunt) that links pulmonary artery and aorta (When: performed within a few days of birth) www.ihm.org.uk Aim (iii) of the Norwood: To create permanent passage (septectomy) between collecting chambers (left and right atria), ensuring that mix of oxygenated and deoxygenated blood flows throughout body (II) HLHS: A Single-ventricle Defect (II.C) Surgical Repair of HLHS (II.C1b) Norwood Procedure (II) HLHS: A Single-ventricle Defect (II.C) Surgical Repair of HLHS (II.C2a) Glenn Shunt (Cavo-Pulmonary Shunt) When: normally performed between three and nine months of age www.ihm.org.uk What (i): redirects flow of deoxygenated blood to lungs How: attaches superior vena cava directly to pulmonary artery What (ii): Gore-Tex shunt from Norwood taken away (II) HLHS: A Singleventricle Defect (II.C) Surgical Repair of HLHS (II.C2b) Glenn Shunt (Cavo-Pulmonary Shunt) www.ihm.org.uk (II) HLHS: A Single-ventricle Defect (II.C) Surgical Repair of HLHS (II.C3a) Fontan Procedure When: performed around three years of age www.ihm.org.uk What (i): separates deoxygenated blood supply from oxygenated blood supply What (ii): allows children to grow, enjoy more physical activity; does not make heart function normal (II) HLHS: A Single-ventricle Defect (II.C) Surgical Repair of HLHS (II.C3b) Fontan Procedure www.ihm.org.uk III. Impact of Single-ventricle Defects A. Neurodevelopmental Issues B. Subsequent Feeding-related Outcomes C. Neurodevelopmental Research Foci (III) Impact of Single-ventricle Defects (III.A) Neurodevelopmental Issues Peak synaptogenesis of medulla seen at 3436 weeks gestation By 35-38 weeks, nervous system sufficiently mature to carry out some integrative functions (e.g., nipple feeding (clumsiness v. coordination) (drawing, cutting, handwriting) (III) Impact of Single-ventricle Defects (III.B) Subsequent Neurobiological/Feeding-related Outcomes (a) Single-ventricle in-utero physiology inhibits synaptogenesis/nervous system development, leading to (b) feeding challenges for the newborn child with surgery-necessitating single-ventricle physiology; (c) corrective surgery results in (d) a post-op recovery period during which oral-feeding challenges are heightened; the (e) extended period of inadequate nutrition yields (f) growth failure and (g) adverse impact on cognitive and socio-emotional development, all of which yield (h) parental anxiety and lack of confidence; parental anxiety and lack of confidence, in turn, produce a tense atmosphere that heightens oral-feeding challenges, which cycles back to (e) and then begins to loop. (Einarson & Arthur, 2003; Lawoko & Soares, 2002) (III) Impact of Single-ventricle Defects (III.C) Neurodevelopmental Research Foci No studies to date have examined best caregiving practices postsurgery IV. Studying the Impact of Caregiving on Post-operative Neurodevelopmental and Oral-feeding Outcomes among Infants Born with Problematic Single-ventricle Physiology: Sables-Baus et al., 2013 A. Care Paradigm Utilized in Study B. Care Environment Utilized in Study C. Study Metrics/Methods/Objectives D. Study Results, Objective by Objective E. Implications for Future Research (IV) Sables-Baus et al., 2013 (IV.A[1-3]) Care Paradigm Utilized in Study (IV.A3) Early, consistent, high-quality interactions to maximize neurodevelopment, social-emotional development, probability of school readiness (IV.A2) Thus, caregiving paradigm similar to one used in NICU to improve neurodevelopment and neurodevelopmental outcomes (IV.A3a) Early, consistent, high-quality interactions with clinical caregivers (IV.A3b) Early, consistent, high-quality parent-child interactions (evidence-based practice) (IV) Sables-Baus et al., 2013 (IV.A4) Care Paradigm Utilized in Study (IV.4a) Profound difference in children’s developmental outcomes (IV.4b) Profound long-term savings in human cost (IV.4c) Profound long-term savings in social expenditures (IV) Sables-Baus et al., 2013 (IV.B1) Care Environment Utilized in Study (IV) Sables-Baus et al., 2003 (IV.B2) Care Environment Utilized in Study Helps families find community programs and resources Includes at homemonitoring program Offers screening for atrisk children with singleventricle physiology Team includes MD, PhD, PNP, CSW, RD Provides neurological/developmental evaluation, diagnosis, intervention Helps educate community health-care providers to increase understanding of needs of children with CHD Has effective tracking mechanisms to increase knowledge and refine care for future patients Administers BSID every 3 months Collects/shares data to establish international guidelines for neurodevelopmental evaluation and care of children with complex congenital heart defects (IV) Sables-Baus et al., 2013 (IV.C1) Study Metrics/ Methods/Objectives Bayley Scales: An Example Subtest Composite Score Percentile Classification Cognitive 105 63 average Motor 100 50 average Age Equivalent 16 mos Fine Motor 18 mos Gross Motor 12 mos Language 121 92 superior Receptive 20 mos Expressive 17 mos Individually administered exam that picks up current condition of developmental delay; does not predict subsequent ability levels, but triggers anticipatory planning of potential intervention strategies • (IV) Sables-Baus et al., 2013 (IV.C2) Study Metrics/Methods/ Objectives Study Methods Chart review of 52 infants with single-ventricle physiology requiring surgical repair, 8/2009-7/2011 Consideration of medical/surgical variables: gestational age, age at surgery, weight at surgery, cross clamp, DHCA/cerebral perfusion time, length of stay, days on ventilator Consideration of Bayley domains: Cognitive, Speech, and Motor Consideration of oralfeeding variables: consultation to OT/SLP, consultation to ENT, swallow studies, UGI, feeding method (IV) Sables-Baus et al., 2013 (IV.C3) Study Metrics/Methods/ Objectives a) To evaluate changes in infants’ Bayley scores from 6 to 12 months b) To evaluate the relationships between medical/surgical variables and 12-month Bayley scores d) To evaluate the relationships between oral-feeding variables and Bayley scores c) To evaluate the relationships between surgical variables and oral-feeding variables (IV) Sables-Baus et al., 2013 (IV.D) Study Results, Objective by Objective First Objective 1. Bayley scores at 6-month follow-up: 20 2. Bayley scores at 12-month follow-up: 29 3. Bayley scores at both time points: 16 4. Data at both time points: paired t-tests used to compare mean Bayley scores from 6 to 12 months 5. Marginally significant decrease in Cognitive and Language scores over time; no change in Motor scores Changes in Bayley Scores from 6 – 12 Months Variable Cognitive Language Motor 6-month Mean (SD) 106.25 (16.38) 98.31 (13.10) 94.06 (21.67) 12-month Paired t-test Mean (SD) 92.00 t=1.90 (28.81) p=0.077 93.38 t=1.90 (11.53) p=0.077 96.44 t=0.70 (18.32) p=0.492 • N=16 infants tested at both 6 & 12 months • Single LV=37.5% (N=6); Single RV=62.5% (N=10) • Paired t-tests (IV) Sables-Baus et al., 2013 (IV.D) Study Results, Objective by Objective Second Objective 1. Variety of medical/surgical variables examined as correlates of 12-month Bayley scores 2. No medical/surgical variables correlated with Cognitive subscale 3. Evidence that greater total LOS, greater CICU LOS, and greater number of days on ventilator related to lower Language and Motor scores at 12 months 4. None of the other medical/surgical variables was related to Language or Motor scores (IV) Sables-Baus et al., 2013 (IV.D) Study Results, Objective by Objective Second Objective, continued In addition, the following categorically measured surgical variables were examined to determine relationships to Bayley scores using independent-sample t-tests: 1. Surgery category (arch & shunt; shunt & PA band; none [native PS]) 2. Complications (yes or no) 3. Diagnosis category (single LV or single RV) 4. Pulse-Ox at discharge (yes or no) None of these t-values was significant, indicating that none of the categorically measured surgical variables related to any of the three Bayley outcomes measured at 12 months. Cognitive Language Motor -0.08 -0.05 0.15 -0.003 -0.05 -0.13 -0.03 0.02 -0.10 0.02 -0.33+ -0.64*** -0.01 -0.38* -0.55** -0.12 -0.37* -0.51** 0.13 -0.02 -0.01 0.07 -0.09 0.16 0.23 -0.12 -0.14 Gestational Age Age at Surgery (in Days) Weight at Surgery Total LOS CICU LOS Days on Ventilator Clamp Time DHCA Time Cerebral Perf Time +p<.10, *p<.05, **p<.01, ***p<.001 Bivariate correlations of medical/surgical variables to Bayley scores (IV) Sables-Baus et al., 2013 Third Objective (IV.D) Study Results, Objective by Objective 1. Surgical Variables: • • • • • • Surgery category (Category 1 v. Categories 2 & 3 combined) Complications (yes or no) Diagnosis category (1 or 2) Clamp time (yes or no) DHCA time (yes or no) Cerebral perfusion time (yes or no) 2. Oral-feeding Variables: • • • • • UMBS (yes or no) ENT consult (yes or no) Feeding method at discharge (breast and/or bottle v. other) Enteral feeding (yes or no) Bottle prior to surgery (yes or no) UMBS (% Yes) Surgery Category Category 1 Categories 2 or 3 Complications Yes No Diagnosis Category Category 1 Category 2 Clamp Yes No DHCA Yes No Cerebral Perf Yes No ENT Consult (% Yes) Feeding@DC (Breast/Bottle) Enteral Feeding (% Yes) Bottle Prior to Surgery (% Yes) 32% 17.7% 34.6% 11.8% 23.1% 58.8%* 69.2% 70.6% 61.5% 64.7% 27.5% 0% 26.8% 0% 31.7% 70.0%* 70.7% 60.0% 60.98% 40.0% 9.1% 31.0% 9.1% 30.0% 63.6% 23.3%** 68.2% 70.0% 45.5% 66.7% 24.4% 17.7% 29.4% 5.9%* 32.4% 52.9% 64.7% 76.5% 58.8% 52.9% 30.0% 10.0% 29.0% 10.0% 29.0% 55.0% 64.5% 75.0% 67.7% 40.0%* 27.8% 18.8% 42.1% 9.4%** 26.3% 46.9% 57.9% 75.0% 52.6% 59.4% Cross tabs were calculated to examine the relationships between the surgical variables and oral-feeding variables. The table shows the percent responding “yes” to the oral-feeding variables across the surgical-variable categories. The * indicates a significant chi-square value (*p<.05, **p<.01). (IV) Sables-Baus et al., 2013 (IV.D) Study Results, Objective by Objective Oral-feeding Variables Used: • UMBS (yes or no) • ENT consult (yes or no) • Feeding method at discharge (breast and/or bottle v. other) • Enteral feeding (yes or no) • Bottle prior to surgery (yes or no) • Oral-feeding amount (total amount divided by LOS) Fourth Objective Relationships of Oralfeeding Variables to 12month Bayley Scores: • No oral-feeding variables related to Cognitive scores • ENT consult related to lower Language (t=2.61, p=0.015) and Motor (t=2.29, p=0.03) scores • Breast and/or bottle feeding v. other method related to higher Motor scores (t=2.37, p=0.025) • No other oral-feeding variables related to Bayley scores (IV) Sables-Baus et al., 2013 (IV.E) Implications for Future Research Need for Further Examination of: • Potential impact of timing of surgical repair • Feeding experience as opposed to feeding volume • Specific caregiving practices • Consistent parental presence—holding, enfolding, olfactory inputs • NIDCAP philosophy—physiological, motor, and state systems • Kangaroo care and pumping *6th World Congress: Pediatric Cardiology & Cardiac Surgery. Cape Town, South Africa, February 17 – 22, 2013: Neurobehavioral Outcomes of Infants seen in Complex Congenital Heart Disease Clinic. *Sables-Baus, S. (2013) Neurocognitive outcomes of infants with single-ventricle physiology seen in complex congenital heart disease clinic. Journal of the South African Heart Association.