Salt and Water Balance
advertisement

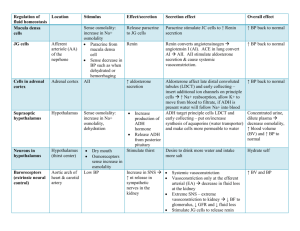
Regulation of Salt and Water Balance General Considerations • Perfusion of tissues is ensured by maintaining both a sufficient volume of arterial blood and adequate pressure to drive it through the capillaries • Several factors go into maintenance of the central pressure: 1. 2. 3. the beating of the heart arteriolar constriction sufficient volume of blood • Central control exerted through the autonomic nervous system provides the minute-to-minute adjustments to cardiac function and arteriolar constriction that maintain blood pressure relatively constant • Volume is regulated largely by the endocrine system, where volume and pressure are closely interrelated Dr. M. Alzaharna (2014) 2 General Considerations • It is not surprising, therefore, that hormones that play vital roles in regulating blood volume also constrict or dilate arterioles • Permeability of capillaries to small molecules allows blood in the vascular compartment to equilibrate quickly with interstitial fluid • Water distributes freely between the vascular compartment and the interstitial compartment • Major determinants of this distribution are: – the protein content of plasma (colloid osmotic pressure), principally albumin, – and blood pressure within the capillaries Dr. M. Alzaharna (2014) 3 • The volumes of fluid in the intracellular and extracellular compartments also are determined by their solute contents • With a few important exceptions in the kidney, biological membranes are freely permeable to water Dr. M. Alzaharna (2014) 4 Salt and Water Balance • Blood plasma is in osmotic equilibrium with interstitial and intracellular fluids; – therefore regulation of plasma osmolality regulates total body osmolality • Because sodium is the major contributor to the osmolality of blood, and because it is largely excluded from the intracellular compartment, changes in sodium balance can change both: – the distribution of body water – and its total volume • Thus, homeostatic regulation of blood volume depends on regulation of intake and excretion of sodium as well as water Dr. M. Alzaharna (2014) 5 Salt Balance • Salt and water balance are maintained remarkably constant despite wide variations in intake and loss of both sodium and water • Intake of sodium may vary from almost none in saltpoor environments to several grams during a binge of potato chips and pretzels • Output is primarily in urine, but smaller losses are also incurred in sweat and feces • Large losses can result from excessive sweating, vomiting, diarrhea, burns, or hemorrhage Dr. M. Alzaharna (2014) 6 Salt Balance • The kidney is a powerful regulator of sodium output and can preserve sodium balance even when daily intake varies over the 4,000-fold range between 50 mg and 200 g Dr. M. Alzaharna (2014) 7 Water Balance • Under basal conditions the typical adult turns over about 1.75 liters of water each day • Most of the water originates from – the diet in the form of solid and liquid foods, – and the remainder is formed metabolically from the oxidation of carbohydrate and fat • Loss occur by: – evaporation from the lungs and skin, – as well as by elimination of wastes in the urine and feces Dr. M. Alzaharna (2014) 8 • So long as intake exceeds losses, balance can be achieved by controlling excretion • Intake, however, is a voluntary act and varies widely • Thirst and salt appetite are increased when intake falls below the amount needed to maintain balance Dr. M. Alzaharna (2014) 9 • Blood volume is monitored indirectly, primarily as a function of pressure • The concentration of sodium, which is the principal osmolyte of plasma and the primary determinant of blood volume, is monitored only indirectly as a function of osmolality • The kidney is the primary effector of regulation, and at least four hormones are used to signal regulatory • Adjustments: – – – – ADH, aldosterone, angiotensin II, and atrial natriuretic factor (also called atrial natriuretic peptide, ANP) Dr. M. Alzaharna (2014) 10 Antidiuretic Hormone (ADH) • ADH (AVP) is the hormone that signals the kidney to conserve water when plasma osmolality is increased or when plasma volume is decreased – The name ADH describes the prompt decrease in urine volume that follows hormone administration – The name AVP refers to the acute increase in blood pressure seen as a result of arteriolar constriction produced when the hormone is administered in sufficient dosage • Osmolality of blood plasma can be increased or decreased by adjusting the proportion of water relative to solute that is excreted in the urine, and thus produce reciprocal changes in the osmolality of the urine Dr. M. Alzaharna (2014) 11 Antidiuretic Effect • The two actions of the hormone are produced by two different G-protein coupled receptors, V1 and V2 Dr. M. Alzaharna (2014) 12 Antidiuretic Effect • Antidiuretic hormone conserves free water by increasing collecting duct permeability to water • Plasma membranes of most cells are permeable to water because of the presence of specialized proteins, called aquaporins (AQPs) that form water channels • ADH stimulates an exocytosis-like process in which the AQP-2 bearing vesicles fuse with the luminal membrane and thus insert AQP-2 • In the absence of ADH, AQP-2 is removed from the luminal membrane by endocytosis and stored in vesicular membranes Dr. M. Alzaharna (2014) 13 Principal cells of the collecting duct Before ADH Dr. M. Alzaharna (2014) After ADH 14 Regulation of ADH Secretion • Plasma osmolality – Osmoreceptors are finely sensitive and elicit increased secretion of ADH when the osmolality increases by as little as 1 to 2% • Blood volume – Changes in blood volume are sensed by receptors in both arterial (high pressure) and venous (low pressure) sides of the circulation – Volume is monitored indirectly as the tension exerted on stretch receptors – The minimal change needed for low pressure receptors to signal ADH secretion is a 10 to 15% reduction in volume • As a general rule, osmolality is preferentially guarded when volume depletion is small • When volume loss is large, however, osmolality is sacrificed in order to maintain the integrity of the circulation Dr. M. Alzaharna (2014) 15 Dysfunctional States • The disease state associated with a deficiency of ADH is called diabetes insipidus and is characterized by abundant production of dilute urine • Nephrogenic diabetes insipidus is the disease that results from failure of the kidney to respond to ADH and may result from defects in: – the V2 receptor, – aquaporin-2, – or any of the regulatory proteins that govern cellular responses to ADH Dr. M. Alzaharna (2014) 16 Dysfunctional States • In the syndrome of inappropriate secretion of ADH , ADH secretion is increased above baseline despite low plasma osmolality • Death may result from a profound dilution of plasma electrolytes because of excessive reabsorption of free water Dr. M. Alzaharna (2014) 17 The Renin-Angiotensin-Aldosterone System Dr. M. Alzaharna (2014) 18 Renin Secretion • Renin is secreted by an exocytotic process that is activated in response to a decrease in blood volume • Three different, but related inputs signal increased secretion of renin: – Juxtaglomerular cells are richly innervated by sympathetic nerve fibers which are activated reflexly by a decrease in arterial pressure – Blood pressure (volume) also is sensed as tension exerted on the smooth muscle cells of the afferent glomerular arterioles – Decreased glomerular filtration, decreases the rate of sodium chloride delivery to the distal convoluted tubules also results in increased renin secretion Dr. M. Alzaharna (2014) 19 Actions of Angiotensin II • Angiotensin II is the primary signal for increased aldosterone secretion by adrenal glomerulosa cells • Actions on the kidney – By constricting renovascular smooth muscle it increases vascular resistance in the kidney and hence decreases renal blood flow and glomerular filtration – Therefore, by decreasing glomerular filtration, angiotensin II decreases sodium and water excretion Dr. M. Alzaharna (2014) 20 Actions of Angiotensin II • Cardiovascular effects – Stimulation of angiotensin II receptors in vascular smooth muscle results in increased intracellular calcium concentrations and sustained vasoconstriction – Acts directly on cardiac myocytes to increase calcium influx and therefore cardiac contractility • Central nervous system effects – Angiotensin II, acting both as a hormone and as a neurotransmitter, stimulates thirst, appetite for sodium, and secretion of ADH through actions exerted on the hypothalamus Dr. M. Alzaharna (2014) 21 Dr. M. Alzaharna (2014) 22 Regulation of the ReninAngiotensin Aldosterone System Dr. M. Alzaharna (2014) 23