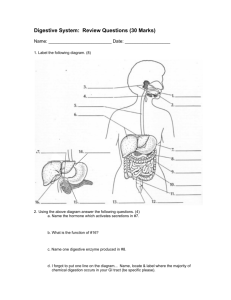
Organs of the Digestive System
advertisement

Organs of the Digestive System For student copy The Mouth • aka oral or buccal cavity • cheeks form lateral walls – internally covered by mucous membrane: nonkeratinized, stratified sq epith – wall of cheeks: buccinator muscle then subq & skin • lips or labia surround opening – inner surface of each lip attached to its gum by a midline fold of mucous membrane called a labial frenulum “small bridle” Mouth - 2 • vestibule: space between buccal mucosa & teeth • oral cavity proper: space that extends from gums & teeth fauces: opening between oral cavity & pharynx • hard palate: anterior portion of roof of mouth – maxillae & palatine bones form bony partition between oral & nasal cavities – covered by mucous membrane MOUTH - 3 • soft palate: forms posterior portion of roof of mouth – muscular partition between oropharynx & nasopharynx – uvula : hangs from free border of soft palate – when swallowing soft palate & uvula drawn superiorly preventing food & liquids from entering nasal cavity Salivary Glands • release saliva into oral cavity • 4 sets: 1. Parotid glands (“near ear”) – between masseter & skin – parotid duct secretes saliva into vestibule opposite 2nd molar 2. Submandibular glands – floor of mouth/ enter just lateral to lingual frenulum 3. Sublingual glands – under tongue 4. lesser Sublingual glands: floor of mouth Salivary Glands Saliva • 99.5% water • 0.5% solutes: – ions – urea & uric acid – mucus – Ig A – lysozyme (bacteriostatic enzyme) – salivary amylase: digestive enzyme acts on starch Salivation • controlled by ANS • average adult secretes 1000 – 1500 mL/day • parasympathetic stimulation promotes continuous secretion keeps mouth moist & lubricates tongue & lips during speech • saliva is then swallowed moistening esophagus most water is reabsorbed • sympathetic stimulation dominates if stressed mouth dry • dehydration: secretion stops to conserve water Mumps • inflammation & enlargement of parotid glands • pain, malaise, fever • swelling on affected side Tongue • skeletal muscles covered by mucous membrane forming floor of oral cavity • median septum separates tongue into symmetric ½ s (attaches to hyoid bone) • lingulum frenulum – limits movement posteriorly – if abnl short: “tongue-tied” • each ½ composed of extrinsic & intrinsic muscles – extrinsic: origins out of tongue/ insert to CT in tongue: move tongue side-to-side/ anchor tongue – intrinsic: origin & insertion in tongue: alter shape & size of tongue for speech & swallowing Tongue - 2 • dorsum (upper surface) & lateral surfaces covered with papillae – projections of lamina propria covered with keratinized epithelium – some contain taste buds – others touch receptors – all increase friction between tongue/food – lingual glands secrete mucous & a watery serous fluid that contains enzyme lingual lipase: acts on triglycerides Taste Buds • most on tongue, few on soft palate, pharynx, & epiglottis • each taste bud has 3 types epith cells: 1. supporting cells – surround ~50 receptor cells 2. gustatory receptor cells – single microvillus 3. basal cells Taste Buds - 2 • each taste bud has 3 types epith cells: 1. supporting cells – surround ~50 receptor cells 2. gustatory receptor cells – single microvillus from each = gustatory hair extends thru a taste pore (opening in taste bud) 3. basal cells – stem cells @ edge of taste bud – produce supporting cells that then develop into gustatory cells (each lasts ~10 days) Teeth • dentes • in alveolar processes of mandible & maxillae – covered by gingivae: “gums” – lined by peridontal ligament: anchors tooth to socket • parts of a tooth: 1. Crown 2. Root 3. Neck Crown of Tooth • visible portion, above level of gums • interior made of dentin: calcified CT – gives shape & rigidity to tooth – harder than bone • covered by enamel – Ca++ phosphate & carbonate – hardest substance in body – protects tooth from: • wear & tear of chewing • acids that could dissolve dentin Pulp Cavity • w/in dentin • pulp: CT with blood, lymph & nerve supply to tooth • extension thru roots = root canals opening @ base for vessels/nerve to enter/exit tooth Root of Tooth • below gums • covered by cementum 2 Dentitions 1. Deciduous teeth – baby or primary teeth – ~6 mos 24/mo 20 total – lost age 6 - 12 2. Secondary teeth – 32 – begin to erupt ~ 6 adult Digestion in the Mouth • mastication: chewing MECHANICAL – food manipulated by tongue/ground by teeth & mixed with saliva – bite of food reduced to soft, flexible, easily swallowed mass = bolus 1. Salivary amylase • initiates breakdown of starch – – into di- & trisaccharides, shorter polymers only monosaccharides can be absorbed 2. Lingual lipase • becomes activated in acid pH of stomach CHEMICAL Pharynx • funnel-shaped tube extends from internal nares esophagus posteriorly & to the larynx anteriorly • skeletal muscle covered by mucous membranes • 3 parts: 1. Nasopharynx: functions only in respiration 2. Oropharynx: digestive + respiratory functions 3. Laryngopharynx: digestive & respiratory Esophagus • collapsable muscular tube • posterior to trachea • begins @ inferior end of laryngopharynx passes thru mediastinum pierces diaphragm (opening called esophageal hiatus) ends in superior portion of stomach Histology of the Esophagus • mucosa: – nonkeratinized stratified sq epith – lamina propria – Muscularis mucosae (smooth muscle) • submucosa: areolar CT • muscularis: – upper 1/3 skeletal – mid 1/3 skeletal & smooth – lower 1/3 smooth Ends of Esophagus • muscularis thickens forming: 1. upper esophageal sphincter (UES) – skeletal – regulates movement of food from pharynx esophagus 2. lower esophageal sphincter (LES) – smooth – regulates movement of food from esophagus stomach Physiology of the Esophagus • secretes mucus & transports food stomach • No enzymes produced or secreted • No absorption Deglutition • swallowing • facilitated by secretion of saliva & mucus • involves mouth, pharynx, esophagus 1. Voluntary stage – bolus of food from oral cavity to oropharynx – stimulates receptors in oropharynx deglutition center in medulla & lower pons effector fibers cause soft palate & uvula to move up to close off nasopharynx AND epiglottis closes off opening of larynx Deglutition Involuntary Stage 2. Esophageal stage • bolus enters esophagus • peristalsis: progression of coordinated contractions & relaxations of circular & longitudinal layers of muscularis, pushes bolus onward Stomach • J-shaped enlargement of GI tract • just inferior to diaphragm • connects esophagus duodenum – most distensible part of GI tract • serves as a 1. mixing chamber 2. holding reservoir Stomach Adaptations for Digestion 1. 2. 3. 4. 5. 6. 7. rugae mucus glands: secretion of H+ & Clpepsin gastric lipase intrinsic factor 3-layered muscularis Anatomy of the Stomach Histology of the Stomach • 4 basic layers in stomach wall: – (stomach wall is impermeable to most substances) 1. surface mucosa = simple columnar epith that extend down into lamina propria where they form columns of secretory cells called gastric glands, channels between columns called gastric pits Mechanical Digestion in Stomach • few minutes after food bolus enters stomach: gentle, rippling, peristaltic movements called mixing waves pass thru stomach q15 – 25 s – macerate food – mix with mucus secretions – results: chyme soupy liquid pylorus Pyloric Sphincter • slightly open • when chyme down to lower pylorus, each mixing wave forces ~ 3 mL chyme into duodenum = gastric emptying Chemical Digestion in the Stomach • salivary amylase: – continues to function while food in fundus – when churning forces bolus further into stomach the acid pH inactivates it • lingual lipase: – acid pH activates – triglycerides fatty acids & diglycerides Chemical Digestion - 2 • H+ & Cl- ions secreted separately by parietal cells • secretion stimulated by: – parasympathetic neurons – gastrin (from G cells) – histamine (from mast cells in lamina propria): receptors on parietal cells = H2 receptors Stomach Acid • kills many microbes in food • partially denatures proteins • stimulates secretion of hormones that promote flow of bile & pancreatic juice Pepsin • secreted by chief cells • greatest activity in low pH / inactivates in higher pH of small intestine • secreted as pepsinogen: inactive form of pepsin (so will not break down proteins in chief cells • severs peptide bonds breaking protein smaller peptide fragments • stomach wall protected from pepsin by alkaline mucus secreted by surface cells Gastric Lipase • splits short-chain triglycerides fatty acids & monoglycerides • most effective @ pH 5-6 (limited role in stomach) Absorption in Stomach • very little in stomach (epithelial cells impermeable to most substances) • mucous cells do absorb some: – water – ions – short-chain fatty acids – aspirin – alcohol Stomach • • • • 2 – 4 hrs for food to exit meal mostly carbs: shortest time protein – rich meal longer fat-laden meal longest Emesis (vomiting) • forcible expulsion of contents of upper GI tract (stomach +/- duodenum) • strongest stimuli: irritation & distension of stomach • other irritants: – unpleasant sites – general anesthesia – dizziness – drugs: morphine, digitalis derivatives Pancreas • retroperitoneal gland: lies posterior to greater curvature of stomach • 3 parts: 1. Head: expanded portion near curve of duodenum 2. Body: 3. Tail: tapering portion • Ducts: 1. Pancreatic: runs length of pancreas, joins bile duct 2. Accessory: branch of pancreatic Histology of the Pancreas • exocrine portion made up of small cluster of glandular cells = acini – about 99% of pancreas – secrete mixture of fluid & digestive enzymes = pancreatic juice Pancreatic Juice • 1200 – 1500 mL/d • mostly: water, salts, sodium bicarbonate (makes pH 7.1 – 8.2), & enzymes (secreted in an inactive form): 1. 2. 3. 4. 5. 6. pancreatic amylase trypsin chymotrypsin carboxypeptidase elastase pancreatic lipase: #1 triglyceride-digeting enzyme 7. ribonuclease & deoxyribonuclease Liver • heaviest gland in body (~1.4 kg or 3 lb) • 2nd largest organ in body • found inferior to diaphragm taking up most of RUQ Anatomy of the Liver • Ligaments: 1. falciform: attaches liver to anterior abdominal wall 2. coronary: attaches liver to diaphragm 3. ligamentum teres: remnant of umbilical vein Anatomy of the Liver • Lobes: 1. left: smaller – includes inferior lobe: quadrate – and a posterior lobe: caudate 2. right: larger Histology of the Liver • lobules: • functional unit of liver • 6-sided structure made of specialized epith cells called hepatocytes – arranged in branching, interconnected plates around a central vein – highly permeable capillaries called sinusoids – fixed macrophages in sinusoids called Kupffer cells destroy worn out RBCs, bacteria or other foreign material in venous blood that just arrived from small intestine Bile • secreted by hepatocytes bile canaliculi bile ductiles bile ducts @ periphery of lobules • eventually, bile flows into larger right & left hepatic ducts combine to form & exit liver as common hepatic duct • made by hepatocytes stored in gallbladder small intestine • function: emulsification of fats (large lipid globules suspension of small lipid globules so can be absorbed Jaundice • yellowish coloration of sclera & mucous membranes due to a buildup of bilirubin – formed as product of breaking down heme pigment in worn out RBCs – excreted in bile – 3 categories: 1. Prehepatic • excess production of bilirubin 2. Hepatic • due to congenital liver disease, cirrhosis, hepatitis 3. Extrahepatic: • blockage bile drainage by gallstones or CA of bowel or pancreas Neonatal Jaundice • aka physiologic jaundice • liver enzymes not always mature @ birth – generally resolves in <10 -12 days – treated with blue lights: changes bilirubin into products that can be cleared by kidneys Functions of the Liver #1 • Carbohydrate Metabolism • liver has important role in maintaining a normal blood glucose level – if low: glycogen glucose increases blood levels – enzymes can convert a.a. or lactic acid glucose – if high: glucose glycogen or triglycerides for short-term or long-term storage Functions of the Liver #2 • Lipid Metabolism • Hepatocytes: – store some triglycerides – fatty acids broken down ATP – synthesize lipoproteins (transport fatty acids, triglycerides, steroids) – synthesize cholesterol & use some to make bile salts Functions of the Liver #3 • Protein Metabolism • Hepatocytes: – deaminate a.a. (remove amine group) (rest of a.a. then used to make ATP or convert to carbs or fats) • amine group urea excreted in kidneys – synthesize most plasma proteins • α & β globulins • albumin • prothrombin • fibrinogen Functions of the Liver #4 • Processing of Drugs & Hormones • detoxifies alcohol & drugs • chemically alters & excretes steroid hormones – thyroid – estrogens – aldosterone Functions of the Liver #5 • Excretion of Bilirubin • absorbed by hepatocytes from aged RBCs then secreted into bile – most bilirubin in bile metabolized in small intestines by bacteria eliminated in feces Functions of the Liver #6 • Synthesis of Bile Salts • used in small intestine for emulsification & absorption of lipids Functions of the Liver #7 • • • • Storage glycogen Vitamins A, B12, D, E, & K Fe, Cu Functions of the Liver # 8 • Phagocytosis • Kupffer cells eat aged RBCs, WBCs, & some bacteria Functions of the Liver # 9 • Activation of Vit D • skin, liver, & kidneys all have role in synthesizing the active form of Vit D Gallbladder • pear-shaped sac found in a depression tucked under liver • function: store bile until fatty chyme enters duodenum – bile cystic duct common bile duct ampulla of Vater duodenum • parts: 1. fundus 2. body 3. neck Gallstones • If bile contains insufficient bile salts or lecithin or excessive cholesterol, the cholesterol crystallizes to form stones • passing small ones can cause intermittent pain but larger ones can obstruct severe pain/infection Small Intestine • site of most major events of digestion & absorption • adaptations 1. 2. – – – long: ~ 10 ft in living adult/ 21 ft in dead surface area increased by circular folds villi microvilli Functions of the Small Intestine 1. segmentations mix chyme with digestive juices & bring food particles into contact with the mucosa for absorption; peristalsis propels chyme thru 2. completes digestion of carbs, proteins, lipids; begins & completes digestion of nucleic acids 3. absorbs 90% of nutrients & water that pass thru Anatomy of Small Intestine • 3 regions 1. Duodenum – “12” width of 12 fingers 2. Jejunum – – 1 m in length “empty” 3. Ileum – – 2m joins large intestine @ ileocecal valve Histology of Small Intestine • same 4 layers of GI tract • mucosa: simple columnar epith with 6 types of cells 1. absorptive cells 2. goblet cells 3. intestinal glands (crypts of Lieberkϋhn) 4. Paneth cells 5. Enteroendocrine cells: S, CCK, K Absorptive Cells • digest & absorb nutrients from chyme • apical membranes form microvilli: projections that increase surface area: form fuzzy line called brush border Crypts of Lieberkϋhn • intestinal glands w/in deep crevices of small intestine mucosa • secrete intestinal juices Paneth Cells • enteroendocrine cells • secrete lysozyme: bactericidal enzyme • also can act as phagocytes Enteroendocrine Cells • S cells: secrete hormone secretin • CCK cells: secrete hormone cholecystokinin (CCK) • K cells: secrete hormone glucosedependent insulinotropic peptide (GIP) Histology of Small Intestine • Lamina Propria: • areolar CT with: – abundance of MALT (mucosa-associated lymphoid tissue) – solitary lymphatic nodules in distal ileum – Peyer’s Patches: aggregated lymphatic follicles also found in ileum Histology of Small Intestine • Submucosa: • Bruner’s glands in duodenum: secrete alkaline mucus that neutralizes the gastric acid in chyme Structural Features that Facilitate Digestion & Absorption: 1. Circular folds: – folds of mucosa & submucosa (~1 cm long) – proximal duodenum mid-ileum – increase surface area for absorption 2. Villi: – fingerlike projections of mucosa (~,5 – 1 mm long) – gives mucosa velvety appearance 3. Microvilli: – brush border Lacteals • the arteiole, venule, capillary bed & a lymphatic capillary (the lacteal) found w/in a villus Intestinal Juice • clear, yellow fluid • + pancreatic juice makes a liquid environment for chemical digestion & absorption • contains: water, alkaline mucus (pH 7.6) Brush-Border Enzymes • absorptive cells secrete several digestive enzymes inserting them into the plasma membranes of microvilli – lumen enzymes (from pancreatic secretions) break larger molecules into smaller ones) – – brush- border enzymes break them down even smaller (small enough to be absorbed) – cytoplasmic enzymes finish digestion Mechanical Digestion in Small Intestine • Segmentations: localized, mixing contractions, occur in portions of sm intestine distended by large vol of chyme – mix chyme with digestive juices – bring particles of food into contact with mucosa for absorption – Do Not push chyme onward Brush-Border Enzymes • • • • • • • digest: α-dextrins maltose sucrose lactose peptides nucleotides Absorption in Small Intestine Absorption of Alcohol • lipid-soluble – so begins absorption in stomach where surface area for absorption much less than in small intestine – longer stays in stomach the slower blood alcohol levels rise – fatty acids in chyme slow gastric emptying – gastric juices have enzyme alcohol dehydrogenase (breaks down alcohol): ♀ 60% less than ♂ so become intoxicated on less • alcohol chyme into small intestine absorption more rapid – greater surface area Large Intestine terminal portion of GI tract ~1.5 m long & 6.5 cm diameter ileocecal sphincter anus attached to posterior abdominal wall by its mesocolon • Regions: 1. Cecum 2. Colon 3. Rectum 4. Anal Canal • • • • Functions of Large Intestine 1. haustral churning, peristalsis, & mass peristalsis 2. bacteria convert proteins to a.a., breakdown a.a., & produce some B vitamins and vitamin K 3. absorption of some: water, ions, vitamins 4. forming feces 5. defecation (emptying rectum) Large Intestine: Layers • Mucosa: – many mucous cells – mucus only secretion – absorptive cells that absorb water • Muscularis: – external layer of longitudinal smooth muscle & internal layer of circular but here longitudinal layer in bands = teniae coli that run most of length – contraction of teniae cause series of pouches = haustra (singular: haustrum) which give organ a puckered appearance Cecum • opening from ileum has fold of mucous membrane = ileocecal valve – hanging inferior to it is cecum (small pouch) – vermiform appendix attached to cecum which is attached to mesocolon by mesoappendix Appendicitis • inflammation of appendix • starts with obstruction to entry of appendix – chyme, tumor, foreign body • Symptoms: high fever, elevated WBC’s (neutrophils), anorexia, pain McBurney’s point – appendix can become edematous, gangrenous, rupture w/in 24 hrs – often patient presents after rupture (much higher mortality rate) Colon Parts of Colon • ascending colon rt hepatic flexure transverse colon lt splenic flexure descending colon level of iliac crest where it becomes sigmoid colon (Sshaped) projects medially to midline terminates as rectum Rectum • last 20 cm of GI tract • anterior to sacrum & coccyx • anal canal: last 2 – 3 cm – mucous membranes arranged in longitudinal folds called anal columns: contain network of arteries & veins – opening to outside body = anus: guarded by an internal anal sphincter (smooth muscle) & an external anal sphincter (skeletal muscle) – normally, both closed except during elimination of feces Mechanical Digestion in Large Intestine • ileocecal sphincter: controls chyme entering cecum – relaxes from hormone gastrin • gastroileal reflex: – starts immediately after meal – intensifies peristalsis in ileum – which forces any chyme there cecum: when distended ileocecal sphincter tightens Mechanical Digestion in Large Intestine - 2 • Haustral churning: characteristic movement in large intestine – Haustra remain relaxed & become distended while they fill up • Peristalsis: – slower rate (3 – 12 contractions/min) than in proximal GI tract • Mass Peristalsis: – strong peristaltic wave begins mid-transverse colon & quickly drives forward contents rectum Chemical Digestion in Large Intestine • done by bacteria acting on chyme 1. use fermentation on remaining carbs gases (H2, C2, CH4) • Flatulence: excessive gas 2. convert remaining proteins a.a. skatole, indole (contributes to odor of feces) 3. decompose bilirubin simpler pigments (gives brown color to feces) 4. produce Vitamin K & some B Vitamins Occult Blood • “hidden blood” (not visible) • screen for colorectal cancer GI Tract Homeostatic Imbalances • Colorectal Cancer: – 2nd to lung ca in males & 3rd after lung & breast in females for deaths due to ca – >1/4th have family hx – 5 – 6% have known gene – ~95% adenocarcinomas: • many start as colon polyp • flat, depressed lesions more likely to be malignant GI Tract Homeostatic Imbalances • Hepatits – – – – inflammation of liver Causes: viruses, drugs, alcohol, chemicals Viral Hepatitis: A: hep A virus • spread by fecal contamination orally • mild in children & young adults • jaundice, malaise , anorexia, nausea, diarrhea, fever, chills • resolves 4 – 6 wks • NO lasting damage GI Tract Homeostatic Imbalances • Hepatitis B – Hep B virus – spread thru body fluids: • sexual contact, contaminated needles or transfusion equipment • tears, saliva, – can be present a lifetime cirrhosis or ca of liver – vaccines available • Hepatitis C hep C virus similar to hep B GI Tract Homeostatic Imbalances • Hepatitis D • Hepatitis E – Hep E spread like Hep • hep D virus A • person must already – No liver damage be infected with hep B – has high mortality in to get hepD pregnant women • severe liver damage • higher fatality rate than hep B alone Medial Terminology • Cirrhosis: • scarred liver due to chronic inflammation due to hepatitis, chemicals, parasites, or alcoholism • jaundice, swelling of lower limbs, uncontrolled bleeding, increased sensitivity to drugs • Dysphagia: • difficulty swallowing due to inflammation, paralysis, obstruction, trauma Medical Terminology • Halitosis: • bad breath • Hernia: • protrusion of all or part of an organ thru a membrane or cavity wall • hiatal hernia • umbilical hernia • inguinal hernia Medical Terminology • Irritable Bowel Syndrome (IBS): • involves entire GI tract • stress-related abd pain or cramping ass’c with alternating diarrhea/constipation • Nausea: • discomfort characterized by loss of appetitie & sensation of impending vomiting • caused by local irritation of GI tract, some other systemic disease, brain trauma, overexertion, or 2° to meds/drugs