drug of abuse
advertisement

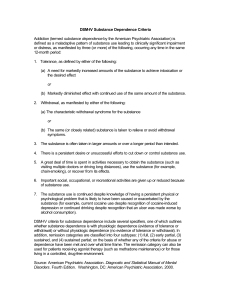
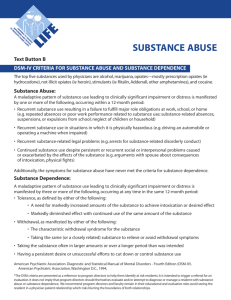
DRUG OF ABUSE Israa omar Drug of abuse • Drug of abuse is usually taken to mean the use of an illicit drugs or the excessive or nonmedical use of a licit drug. • It is also denotes the deliberate use of chemicals that generally are not considered drugs by the lay public but may be harmful to the user. • A primary motivation for drug abuse appear to be the anticipated feeling of pleasure derived from the CNS effects of the drug. Drug of abuse • The older term physical dependence is now generally denotes as dependence, whereas psychological dependence is more simply called addiction. High-yield terms to learn • Abstinence syndrome: – Term used to describe the signs and symptoms that occur on withdrawal of a drug in a dependent person. • Addiction: – Compulsive drug using behavior in which the person uses the drug for personal satisfaction, often in the face of known risks to health; – Formerly termed psychological dependence. High-yield terms to learn • Controlled substance: – A drug deemed to have abuse liability that is listed on governmental schedules categorize illicit drugs, control prescribing practices, and mandate penalties for illegal possession, manufacture, and sale of listed drugs. – Controlled substance schedules are presumed to reflect current attitudes toward substance abuse; therefore which drugs are regulated depends on social judgment. High-yield terms to learn • Dependence: – A state characterized by signs and symptoms, frequently the opposite of those caused by a drug, when it is withdrawn from the chronic use or when the dose is abruptly lowered; – Formerly termed physical or physiologic dependence High-yield terms to learn • Designer drug: – A synthetic derivative of a drug, with slightly modified structure but no major change in pharmacodynamics action. – Circumvention of the schedules of controlled drug is motivation for the illicit drug synthesis of designer drugs High-yield terms to learn • Tolerance: – Decrease response to drug, necessitating larger doses to achieve the same effect. – This can result from increased disposition of the drug (metabolic tolerance), an ability to compensate for the effect of a drug (behavioral tolerance), or changes in receptor or effector systems involved in drug actions (functional tolerance) • Withdrawal symptoms: – May be experienced upon discontinuation. – Some of these symptoms are generally the opposite of the drug's direct effect on the body. The Dopamine Hypothesis Of Addiction • Dopamine is the mesolimbic system appears to play a primary role in the expression of reward, but excessive dopaminergic stimulation may lead to pathologic reinforcement such that behavior may become compulsive and no longer under control-common features of addiction. • Though not necessarily the only neurochemical characteristic of drug abuse, it appears that most addictive drugs have actions that include facilitation of the effects of dopamine in the CNS. Major groups of drugs that are subject to abuse 1. 2. 3. 4. 5. 6. 7. Opioids analgesics: Morphine and Heroin Sedative/hypnotics. Stimulants. Hallucinogens Marjuana Inhalants Steroids 1. Opioid analgesics (Effect) • The primary targets underlying the action of opioids analgesics are the δ,µ and ĸ receptors. • They also have action including disinhibition in dopaminergic pathways in the CNS. • The most commonly abused drug in this group are heroin, morphine, codeine, oxycodone and among health professionals, meperidine and fentanyl. • The effect of IV heroin are described by abusers as a rush or orgasmic feeling followed by euphoria and then sedation • IV administration is associated with rapid development of tolerance , dependence and addiction. Opioid Analgesics (Over dose) • Overdose of opioids leads to respiratory depression progressing to coma and death. • Overdose is managed with intravenous Naloxone or Nalmefene and ventilatory support. Opioid Analgesics ( Withdrawal) • Deprivation of opioids from physiologically dependent individuals leads to an abstinence syndrome that includes lacrimation, rhinorrhea, yawning, sweating, weakness, gooseflesh, nausea and vomiting, tremor, muscle jerks and hyperpnoea. • Withdrawal from opioids although unpleasant is rarely fatal Opioid analgesics ( withdrawal) • Treatment involves replacement of illicit drug with a pharmacologically equivalent agent (e.g. Methadone) followed by dose reduction. • Buprenorphine a partial agonist at µ and longer acting (more than 40 h), is also used to suppress withdrawal symptoms and as substitution therapy for opioids addicts. • The administration of naloxone to a person who is using strong opioids (but not overdosing) may cause more rapid and more intense symptoms of withdrawal). • Neonates born to mothers physiologically dependent on opioids require special management of withdrawal symptoms 2. Sedative- Hypnotics • The sedative-hypnotics drugs are responsible for many cases of drug abuse. • The group include ethanol, barbiturates, and benzodiazepines. • Benzodiazepines are commonly prescribed drugs for anxiety and as Schedule IV drugs, are judged by the US government to have low abuse liability. • Short acting barbiturates have high addiction potential. • Ethanol is not listed in schedules of controlled substances but it has abuse liability. Sedative- hypnotics (effects) • Sedative-hypnotics reduce inhibitions, suppress anxiety, and produce relaxation. • All of these action are thought to encourage repetitive use. • These drugs also enhance brain dopaminergic pathways, the latter action possibly related to the development of addiction. • These drugs are CNS depressants, and their depressant effects are enhanced by concomitant use of opioids analgesics, Marijuana, antipsychotics and any other drugs with sedative properties. Sedative- hypnotics(effects) • Flunitrazepam (Rohypnol), a potent rapid onset benzodiazepines with marked amnestic properties, has been used in (date rape). • Added to alcoholic beverages, chloral hydrate or ϒ-hydroxybutrate (GABA agonist) also render the victim incapable of resisting rape. Sedative- Hypnotics (Overdose ) • Acute over doses may result in death through depression of the medullary respiratory and cardiovascular centers. • Management of overdose include maintenance of patent airways plus ventilatory support . • Flumazenil can be used to reverse the CNS depressant effect of benzodiazepines, but there is no antidote for barbiturates or ethanol. Sedative- hypnotics (Withdrawal ) • Physiological dependence occur with continued use of sedative-hypnotics; the signs and symptoms of the withdrawal (abstinence) syndrome are most pronounced with drugs that have a half life of less than 24 h (e.g. ethanol, secobarbital). • However it also occur with any sedativehypnotics, including the longer acting benzodiazepines. • The most important signs of withdrawal derive from excessive CNS stimulation and include anxiety, tremor, nausea and vomiting, delirium and hallucination. • Seizures are not uncommon and may be life threating. Sedative- hypnotics (Treatment of withdrawal ) • Treatment of withdrawal involves administration of long acting sedative-hypnotics ( chlordiazepoxide or diazepam) to suppress the acute withdrawal syndrome, followed by gradual dose reduction. • Clonidine (inhibits exaggerated neurotransmitter release) or propranolol may also be of value to suppress sympathetic over activity. Sedative- hypnotics (Treatment of withdrawal) • The opioid receptor antagonist naltrexone reduces alcohol-induced reward (unclear mechanism) • Disulfiram: blockade of ADH lead to accumulation of acetaldehyde- nausea, flushing, tachycardia, hyperventilation, panic… • Aim: to make alcohol consumption unpleasant and intolerable it is used for treatment of dependence not for acute withdrawal syndrome. 3. Stimulants I. Methylxansines • Natural alkaloids occurring in various beverages, namely tea, coffee, cocoa and cola-flavored drinks • Substances: caffeine, theophylline, theobromine • Pharmacological effects: 1. CNS stimulation 2. Diuresis (vasodilatation of the afferent glomerular arteriole) 3. Stimulation of cardiac muscle 4. Relaxation of smooth muscle, especially bronchial. Methylxansines Effects 1. Inhibition of phosphodiesterase, responsible for intracellular metabolism of cAMP 2. Antagonism on adenosine receptors • Tolerance and habituation develop to a small extent and withdrawal effects are very slight (headache, fatigue) • Toxicity: from over-dosage of caffeine include excessive CNS stimulation with tremor, insomnia, and nervousness; cardiac stimulation and arrhythmia. II. Nicotine • It appears to be the only pharmacologically active substances in tobacco smoke. • One cigarette contain about 9-17mg of nicotine, of which 10% is normally absorbed. Effects : 1. In the brain it causes neuronal excitation that can be blocked by Mecamyline 2. In the spine it inhibits spinal reflex and thus causing muscle relaxation 3. In the peripheral tissues, nicotine stimulates the receptors at the ganglion and causes tachycardia, hypertension and reduced GI motility Nicotine • Tolerance: to peripheral (not central) ganglionic stimulation, perhaps due to desensitization of receptors • Physical dependence craving: increased irritability, anxiety, impaired performance of psychomotor tasks, aggressiveness and sleep disturbances, headache increased appetite lasts for 2-3 weeks. • Psychological dependence and addiction. • Severe toxicity has been described in children who ingest nicotine gum or patches. Nicotine (Treatment of dependence) 1. Counselling 2. Nicotine replacement therapy – Nicotine in patches (controlled release), chewing gums, nasal sprays several times daily (short effect) 3. Adjunct therapy – Bupropion, TCAs and MAOI – Mecamylamine – Varenicline: which occlude the rewarding effect of nicotine – Rimonabant: is also used in smoking cessation III. Amphetamines • Substances: Amphetamine, dextrometamphetamine and methamphetamine • Routes of administration: oral, nasal, inhalation and parenteral • Mechanism of action: – Indirect CNS ‘sympathomimetic’ effect – release of monoamines (noradrenaline, dopamine, or 5HT) from nerve terminals in the brain. Main effects on CNS: 1. Locomotor stimulation 2. Euphoria and excitement, increased selfconfidence, stereotyped behavior, resistance to fatigue, decreased appetite, anorexia Amphetamines (Withdrawal syndrome) • Tolerance develops rapidly to the peripheral sympathomimetic and anorexic effects, but more slowly to the central effects • No clear-cut physical withdrawal syndrome → dependence seems to be a consequence of the unpleasant after-effects (i.e. fatigue, lethargy, anxiety, depression, hunger) and the effort to avoid them. Amphetamines (Dependence) • Full-blown dependence occurs in 5% of users – characterized by strong craving, increased doses, and common uncontrolled ‘runs’) • Amphetamine psychosis – closely resembles the Schizophrenic attack – incoherent thought, hallucinations, paranoia, aggression. • Chronic abuse can cause necrotizing arteritis leading to cerebral hemorrhage and renal failure. • Therapeutic use: minimal e.g. narcolepsy, hyperkinetic syndrome and treatment of obesity IV. Congeners Of Amphetamines • Several chemical congeners of amphetamines have hallucinogenic properties. • These include: – 2,5-dimethylamphetamine (DOM) – Methylene dioxyamphetamine (MDA) – Methylene dioxymetamphetamine (MDMA) Congeners Of Amphetamines • MDMA has more selective action on serotonin transporter in the CNS and is used to cause euphoria and as sexual enhancer. • Overdose toxicity include hyperthermia, serotonin syndrome and seizures. • Withdrawal syndrome with protracted depression has been described in chronic users of MDMA. V. Cocaine • The most expensive drug illegally sold • Routes of administration: Salt - nasal or I.V., free base: smoking-inhalation Mechanism of action: • Inhibition of catecholamine Re-uptake → increase noradrenaline and dopamine transmission • Indirect ‘sympathomimetic’ agent Pharmacological effects: • Very similar to those of amphetamines yet less prone to cause stereotyped behavior, paranoia, delusions. Cocaine • Duration of effect is much more shorter (30 min, I.V) than in amphetamines, • Rapid metabolism – liver and plasma esterase (hair deposit of metabolites). • No clear-cut physical dependence syndrome but depression, tiredness and dysphoria coupled with very intensive craving for the drug (strong psychological dependence). 4. Hallucinogens I. Phencyclidine PCP • Antagonist at NMDA receptors, has no action on dopaminergic neurons in the CNS. • The most dangerous of the hallucinogenic agents. • Chemically related to ketamine (anesthetic drug) and originally also developed as a drug with this indication. • Not so frequent among abusers, unpleasant vegetative effects. • Can cause severe delusions and/or hallucination which may turned into the violent behavior • Overdose can cause nystagmus, marked hypertension, and seizures, which can be fatal. II. LSD (Lysergic Acid Diethylamide) • Originally produced as a drug candidate in Sandoz Labs in 1938 by Albert Hoffman • It is among the most potent drugs known so far • Mechanism of action: – Acting on different 5-HT receptors in CNS no effect on dopamine receptor. – Interestingly it dose not cause dependence. – Mainly as agonist on 5-HT2A autoreceptors in CNS →↑firing of 5-HT neurons in Raphe N • Somatic effects: – Sympathomimetic (↑BP and HR) – Tolerance: develops quickly (on CNS effects) • Adverse effects: – Persistent mental disorder – Schizophrenia – Injury due to violent behavior 5. Marijuana • Extracts of the hemp plant; originally from Himalaya and Kashmir • Marijuana - dried leaves and flower heads • Hashish - extracted resin • Active substances: cannabinoids (lipophilic nonalkaloid natural compounds) • Routes of administration: mainly inhaled in cigarette smoke Marijuana (mechanism of action) • Through cannabinoid receptors (GPCR type) 1. CB1- brain – Highly abundant in: hippocampus (memory), cerebellum (loss of coordination), and substantia nigra (motor disturbances), hypothalamus (appetite) and mesolimbic dopaminergic pathway (reward) and cortex. – Mostly localized presynaptically– their activation inhibits neurotransmitter release – Their paucity in the brain stem → lack of serious respiratory and cardiovascular toxicity. – Endogenous agonist: anandamide 2. CB2- periphery – immune system (immunosuppressive effects?!) Marijuana (Pharmacological effect) On CNS a combination of psychotomimetic, depressant effect: • A feeling of relaxation, well-being and euphoria without accompanying aggression • Uncontrolled laughing without reason • A feeling sharpened sensory awareness • Impairment of motor coordination (driving), short-term memory and judgment. • Feeling of time passing slowly, depersonalization; increased appetite. • Analgesia, antiemetic action • In high doses: hallucination, paranoia, anxiety Marijuana (Pharmacological effect) Peripheral effects: • Vasodilatation (obvious on conjunctive vessels) • Tachycardia • Bronchodilation (but opposite may appear during smoking) • Reduction of intraocular pressure • Tolerance and physical dependence occur only to a minor degree in heavy users Withdrawal syndrome: • Weak and usually mild irritability, restlessness, confusion, sweating tremor and sleep disturbances Marijuana (Harmful effect) • Relatively safe from the viewpoint of acute drug overdose • Problems are rather with chronic use: – Somatic effects: decreased testosterone and sperm count – Long-term psychological changes: apathy, impaired memory and decision ability, may promote schizophrenia in pre-disposed patients. 6. Inhalants • Certain gases or volatile liquids are abused because they provide a feeling of euphoria or disinhibition. • This group include: 1. Anesthetics 2. Industrial solvents I. Anesthetics • This group includes nitrous oxide, chloroform and diethylether. • Such agents are hazardous because they affect judgment and include loss of consciousness. • Inhalation of nitrous oxide as the pure gas (with no oxygen) has caused asphyxia and death. II. Industrial solvents • Solvents and wide range of volatile compounds are present in commercial products such as gasoline, paint thinners, glues and shoe polish. • Because their ready availability, these substances are most frequently abused by children in early adolescence. • Active ingredients that have been identified include benzene, hexane, methylethylketone, toluene and trichloroethylene • Many of these are toxic to liver, kidneys, lungs, bone marrow, and peripheral nerves and cause brain damage in animals. III. Organic Nitrites • Amyl nitrite, isobutyl nitrate, and other organic nitrates are referred to as poppers and are mainly used as sexual intercourse enhancer . • Inhalation of the nitrites causes dizziness, tachycardia , hypotension and flushing. • With the exception methaemoglobinaemia the adverse effect are usually mild . 7. Steroids • In many countries, including the US, anabolic steroids are controlled substances based o their potential for abuse. • Effect sought by the abusers are increases in muscle mass and strength rather than euphoria . • However, excessive use can have adverse behavioral, cardiovascular, and musculoskeletal effects. • Behavioral manifestation include increase libido and aggression (roid rage) Steroids • Severe acne and female masculinization are anticipated androgenic adverse effects. • Hepatic dysfunction has been reported, and increase risk of myocardial infarction. • A withdrawal syndrome has been described with fatigue and depression of mood. Good luck Reference: • pharmacology by Lange • Rang and dale pharmacology