Substance Abuse Disorders
advertisement

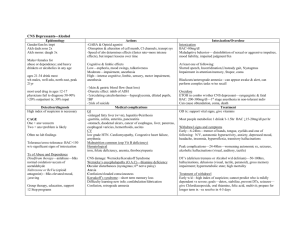
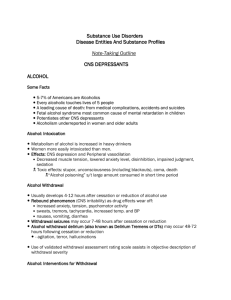
Substance Abuse Disorders NU124 Criteria: SUBSTANCE ABUSE Must have one or more in the past 12 months: Recurrent use in physically dangerous settings Recurrent drug-related legal problems Continued use despite recurring interpersonal problems Continued: Failure to fulfill role obligations at home, school, or work Criteria: SUBSTANCE DEPENDENCE Three more in the last 12 months: Drug intolerance Drug withdrawal Use is greater in amount and frequency of use than intended (loss of control) Persistent desire and unsuccessful attempts to stop or control Continued: Increasing time and energy to obtain the drug Lifestyle changes (social, recreational or occupational) Use continues despite problems Intoxication Reversible substance-specific syndrome Clinically significant behavioral or psychological changes Not due to another mental disorder Withdrawal Substance-specific syndrome due to cessation Clinically significant distress Not due to another condition Behaviors Manipulation Grandiosity Denial Isolation Decreased occupational functioning Impaired relationships Assessment CAGE: Cut down? Annoyed? Guilty? Eye-opener? ALCOHOL INTOXICATION CNS Impairment – brain function to peripheral NS, absorbed in stomach, all systems affected. See Townsend, p. 416+ Acute, Metabolize – gone and symptoms go Long tem effects with use = Amounts Quantities ****CNS depression**** Acute alcohol intoxication Changes in mood Poor psychomotor coordination Impaired memory and judgment Impaired social functioning Behavior changes BAL of 100-200 mg/ml Remember “Tolerance” Withdrawal What is the opposite of CNS depression? What have you studied in NU 110 that is similar to this? ***Sympathetic NS Hyperactivity*** Similar to physiological stress response Symptoms Tremors Elevated VS Anxiety, irritability Insomnia Diaphoresis ***Onset: 4-12 hours after last drink Withdrawal Peak is 2 – 3 days GREATEST RISK: Alcohol delirium, DT’s, Delirium tremens *** A medical crisis Occurs on second to third day following last drink Prevent DT’s. Get pt. past this window. Alcohol delirium Autonomic NS hyperactivity: cardiac, smooth muscles, glands Hallucinations, illusions, delusions Fluctuating LOC Seizures N and V Detoxification Priority #1: Physiological stability, safety Monitor: BP and P, R and T; q 4 hrs: Medicate: Use of cross dependent sedatives, titration based on degree and number of symptoms. What class of drugs have a sedative/CNS depressant effect? Use these_________________________ Continued: Fluids – replacement and enhance detoxification via kidney and liver - if functioning normally Nutrition – alcohol decreases appetite; Thiamine(Wernick’s encephalopathy), Folic acid and MVI Continued: Reduce risk of seizures: MgSo4, Anticipate anticonvulsants Reduce risk of stroke: antihypertensives Continued: Priority #2: Address the denial Around day 3 Matter of fact, no judgment, tell the facts of patient condition and directly link to alcohol use “As a result of your body’s dependency on alcohol, it reacted with the symptoms of__________________. This indicates damage to …” Continued: “Alcohol use is damaging your body. Examples of this are____________.” continued Priority #3: Plans for sobriety, learning to live sober. Contingent upon belief that alcohol use has created problems. “What would you like to have happen in your life now?” “What do you wish for?” At discharge In-patient rehabilitation or, home and AA Sobriety Medications – adjunct to learning to cope, re programming responses Antabuse – negative reinforcement Naltrexone – decrease cravings Campral – decrease distress, improve mood, contraindicated in liver inpairment MEMORIZE THESE Continued: Continue to address denial and powerlessness over alcohol – AA Practice new ways to cope Counseling on coping and repairing relationships New relationships, lifestyle changes Family Don’t feel Don’t trust Don’t expect Continued: Deny the problem Use a substance Develop a symptom Kick the user out Co-dependence (part of denial) – the need to be needed Learn to cope with substances Family treatment Family therapy to repair relationships, family structures, re-set family roles Alanon – adult – learn to give up responsibility for the user and his/her substance use Alteen – Adolescents: Leaning to cope, not overfunction, have sx., or use substances Part II - Other drugs Why does the brain prefer opium to broccoli? A shortcut to the brain’s reward system Floods the nucleus accumbens with dopamine Hippocampus lays down memories of rapid satisfaction – Feels GREAT Continued: Amygdala creates a condition response to certain stimuli Stressors or something associated with substance use, trips the mental machinery of relapse* Conditioned response Very neuophysiologic *Harvard Mental Health Newsletter, Volume 21, No. 1, 2004, p.1. OTHER DRUGS CNS DEPRESSANTS: Opiods Effects: Suppress sympathetic NS. Load endorphin receptor sites = euphoria and analgesia Depletes serotonin which regulates pain perception and anxiety Heroin Name other similar CNS depressants _____ Continued: Withdrawal: 6 – 8 hrs = nervous and edgy Runny nose, tearing, pilorection Muscle, joints and bones ache N and V, diarrhea Lasts 4 – 8 days Not lethal Continued: Treatment: No CNS drugs;will cause cross addiction Systems support - e.g., diarrhea Fluids and nutrition as tolerated Emotion support Replacement therapy/ methadone clinics Lifestyle change and coping STIMULANTS: Cocaine/crack Effects: Stimulates CNS = well-being, energy and euphoria Blocks reuptake of norepinephrine, dopamine and serotonin Tachycardia, HTN, increased resp. and metabolic rate Name other stimulants: ____________ Continued: Anorexia but craves high-sugar, restlessness Massive systematic vasoconstriction = MI, CVA, spontaneous abortion Who will be at risk? Aged, pregnant f females Continued: Withdrawal: Overwhelming fatigue Dysphoria and anhedonia Even after drug has been detoxed, neurotransmitter levels are so unbalanced = clinical depression Suicide precautions STIMULANT: Methamphetamine Coming soon to your neighborhood Releases high levels of dopamine Enhances mood Intense rush or “flash”. Very different from cocaine MA high lasts 8 – 24 hrs; cocaine lasts 20 - 30 minutes Continued: MA effects Euphoria, increased attention and libido Increased activity with decreased fatigue and appetite Toxicity from binging – visual hallucinations, violence, elevated BP, R, and Temp. Tolerance Continued: Treatment for toxicity (Intoxication) Acute ER: IV Haldol for agitation, IV medications for controlling BP and preventing seizures Cardiac monitoring, IV hydration Reducing hyperthermia if present Continued: Chronic use at lower dosages: No physical manifestations of withdrawal BUT: Depression, anxiety, fatigue, paranoia, aggression and an intense craving for the drug HALLUCINOGENS Mind Altering: PCP, LSD Low doses – euphoria Higher - hallucinations, delusions, peripheral anesthesia, agitation Risk for trauma due to altered state Long term: sympathomimetic signs Continued: Treatment: No Withdrawal syndrome but: When insufficiently metabolized, stored in fat. Metabolize fat tissue = released into circulation producing hallucinations later = flashbacks OR brain damage due to use. Acute sx. in ER – agitation, ensure pt. safety Inhalants Benzene, nitrates: paint, glue, lighter fluid Very addicting Affects Cardiac and CNS Intoxication: euphoria, giddiness, drowsiness Chronic: Dysrythmias, renal and liver, organic mental changes Teens – buy in drugstore or hardware store