Aortic Insufficiency - Framing the Issue Through INTERMACS
advertisement

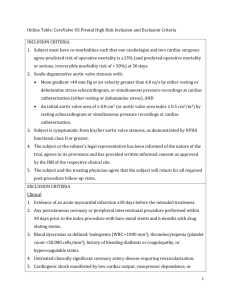
Aortic Insufficiency – Framing the Issue Through INTERMACS Scott Silvestry, MD Disclosures. Consultant Thoratec , HeartWare Research Support Thoratec (2012) No off label use/indications will be discussed. Asking a Question? Question (Respondent) Response What movie would you like to see?( Spouse) Is it cancer?(Radiologist) Would you agree that the standard was not met? (Lawyer) What is the best treatment?(Clinician) What should a surgeon do with AI at the time of a VAD?(INTERMACS) Tread lightly- consider previous choices and whose choice was last made. Cannot rule out…. Please restate. It depends. Let’s look at the data. Aortic Insufficiency Clinician Aspects Mechanical Valve Carries Perceived Risk Of Stroke Aortic Insufficiency Impaisr MCS By Short Circuit Aortic Insufficiency Will Worsen With Time How durable are any of the options? Considerations The addition of ischemic time ( cross clamp) to sick hearts (RV) Cross clamp time varies by technique Don’t Valves and repairs just fuse eventually anyway? DAAP Suggestions 1) What are the outcomes of patients with important AI who do not undergo an AV procedure compared to those that do have an AV procedure performed; and, 2) What are the outcomes of patients that undergo an AV procedure with respect to the type of procedure performed? Compare important outcomes of patients stratified to the following groups by pre-implant assessment of the degree of AI and subsequent intervention: Group 1: AI – None; Group 2: AI – Mild with NO AV procedure performed; Group 3: AI – Mild with AV procedure performed; Group 4: AI – Moderate or more with NO AV procedure performed; and Group 5: AI – Moderate or more with AV procedure performed. For those patients that did receive an AV procedure, the patients should be stratified by type of procedure; Group I – AV replacement; Group II – AV repair; Group III – Other AV procedure. The outcome measures that the DAAP Committee would recommend/suggest to assess would be: 1) survival; 2) duration of inotrope support; 3) freedom from RV failure; 4) renal function (both early and late); 5) duration of ICU stay; 6) total LOS for index hospitalization; 7) freedom from readmission; and 8) freedom from AI – Moderate or more. The outcome measures that the DAAP Committee would recommend/suggest to follow would be 1: Survival; 2) Freedom from stroke; 3) Freedom from AI – Moderate or More; and 4) Freedom from RV failure. These outcomes measures would importantly assess the stroke risk from each of the procedures and durability of preventing recurrence of AI. Why INTERMACS? Size of Data Prospective data Data Capture LONGITUDINAL DATA- ALIVE/DEAD/ECHO DATA Nice People. INTERMACS: June 2006 – December 2012: Aortic Insufficiency All Primary Pts implanted As of 12/31/2012 N=7887 Pediatric Patients: n=79 (patients < 19 yrs of age at time of implant) Adults: n=7808 Pulsatile Flow: * N=1087 BiVAD: 301 TAH: 158 Patient Pool Continuous Flow: n=6721 LVAD: 628 Bi VAD: 179 LVAD: 6542 7 * The left ventricular device indicates the type of pump implanted (continuous flow or pulsatile flow). A visit to INTERMACS Problems? • Data not complete • Apparent Inconsistencies in responses – Severe AI with no procedure???? – Replacement with mechanical valve • Previous version did not capture the same fields/data • Massive Variation in Clinical practice and terminology. "The aorta was clamped and infused with cold blood cardioplegia antegrade for a total of 1L. A Transverse aortotomy was made. Mildly to moderately thickened aortic valve lesions were noted. Using three stripes of Teflon and running 4-0 Prolene suture, the aortic valve was closed shut to deal with the aortic insufficiency. The aortomoy was then closed with 4-0 Prolene suture in two layers." "The previously placed Bjork-Shiley valve was visualized. A sandwich felt technique was used to patch the valve from the ventricular and the aortic aspect in order to prevent any exposure of the valave to circulation to reduced the development of thrombosis and passive mobilization. This was done with 2 circular patches sutured together through the aortic valve prosthesis. An additional portion of felt patch had to be used to completely cover the aotic valve on the aortic aspect. The patch was then sewn to the side of the graft to fully exclude the valve. The aortotomy was then closed with 2 running layers of 4-0 Prolene." 3 pledgeted sutures 3 pledgeted sutures 4 pledgeted matress sutures These were the good ones! 4-0 prolene pursestring suture on each leaflet; additional pledgeted 4-0 prolene between rt & lt commissures. A piece of bovine pericardial patch was fashioned to the size of the aortic valve. It was sewn into place to cover the aortic valve using a series of 4 pledgeted 4-0 Prolene sutures. All had notes that stated AV was repaired, but in details in the notes all were found to have been oversewn with leaflets closed. Aortic VALVE OVERSEWN-pericardial patch Aortic VALVE OVERSEWN-pericardial patch AV oversewn closed w/ pledgetted suture and prolene AV oversewn closed w/ pledgetted suture and prolene N/A N/A N/A Oversewing of aortic valve Pre-exisiting MECHANICAL AV SURGERY--Aortic VALVE OVERSEWN-percardial patch Replacement of aortic valve with Hemashield patch INTERMACS: June 2006 – December 2012: Aortic Insufficiency Additional Data Collection Summary Question 1: Patients with Moderate/Severe Aortic Insufficiency at time of implant but no concomitant AV surgery recorded: patients=131, hospitals=59 Question 2: Patients with Documented Concomitant Aortic Repair at time of implant – verification of AV closure and/or AV repair: patients=213, hospitals=62 Total Patients = 326 Total Hospitals = 88 11 INTERMACS: June 2006 – December 2012: Aortic Insufficiency Original Groups prior to additional data collection Groups 1)Aortic Closure 2)Aortic Repair 3)Aortic Replacement – Bio/Mech 4)All Others Total n 81 213 95 6332 6721 LVAD 76 209 92 6165 6542 BiVAD 3 4 3 169 179 Group distribution AFTER finalization of additional data collection Final Groups 1)Aortic Closure 2)Aortic Repair 3)Aortic Replacement – Bio/Mech 4)All Others Total n 136 165 103 6317 6721 LVAD 131 163 100 6148 6542 BiVAD 5 2 3 169 179 13 INTERMACS: June 2006 – December 2012: Aortic Insufficiency Group Summary AFTER finalization of additional data collection Aortic Regurg – Pre-implant Groups n None Mild 1)Aortic Closure 136 19 (14.0%) 58 (42.6%) 2)Aortic Repair 165 20 (12.1%) 69 (41.8%) 3)Aortic Replacement (Bio/Mech) 103 12 (11.7%) 33 (32.0%) 4)All Others 6317 3584 (56.7%) 1348 (21.3%) 83 (1.3%) Total 6721 3635 (54.1%) 1508 (22.4%) Mod 34 (25.0%) 47 (28.5%) 28 (27.2%) 14 (0.2%) 192 (2.9%) Sev Unknown 8 (5.9%) 17 (12.5%) 1 (0.7%) 28 (16.9%) 7 (6.8%) 23 (22.3%) 1288 (20.4%) 30 (0.4%) 1356 (20.2%) Aortic Regurg – Pre-implant Groups n None Mild 1)Aortic Closure 119 19 (16.0%) 58 (48.7%) 2)Aortic Repair 137 20 (14.6%) 69 (50.4%) 3)Aortic Replacement (Bio/Mech) 80 12 (15.0%) 33 (41.3%) 4)All Others 5029 3584 (71.3%) 1348 (26.8%) 83 (1.6%) Total 5365 3635 (67.8%) 1508 (28.1%) Mod 34 (28.6%) 47 (34.3%) 28 (35.0%) 14 (0.3%) 192 (3.5%) Sev 8 (6.7%) 1 (0.7%) 7 (8.7%) 30 (0.6%) 14 16 Concomitant Aortic Valve Procedures in Patients Undergoing Implantation of Continuous-Flow LVADs: An INTERMACS Database Analysis April 11, 2014 Jason Robertson, M.D., M.S.; David C. Naftel, Ph.D., Sunil Prasad, M.D.; Akinobu Itoh, M.D.; Susan Myers; Gail Mertz, B.S., R.N., CCRC; James Kirklin, M.D.; and Scott Silvestry, M.D. Disclosures: Robertson – none; Naftel – none; Prasad - none; Itoh – none; Myers – none; Mertz – none; Kirklin – none; Silvestry – Consultant for Thoratec and HeartWare This project has been funded in whole or in part with federal funds from the National Heart, Lung and Blood Institute, National Institutes of Health, Department of Health and Human Services, under Contract No. HHSN268201100025C Outcomes Following Aortic Valve Procedures • Previous studies have disagreed on whether mortality after concomitant aortic valve procedures is increased, with some studies demonstrating equivalent or improved survival. • The largest of these used data from the HeartMate II BTT and DT Trials (n=1,106), including: • 30 AVRs • 32 AV closures • 18 AV repairs • Long term survival was significantly reduced compared to HMII implant alone: • 1-year Survival: 57% vs. 75%, p=0.001 • 2-year Survival: 43% vs. 64%, p=0.001 Dranishnikov N, et al. Int J Artif Organs. 2012; 35 (7): 489-94. John R, et al. JTCVS. 2014; 147: 581-589 Pal JD, et al. Circulation. 2009; 120: S215-219 Adamson RM, et al. JHLT. 2011; 30: 576-582 Goda A, et al. Ann Thorac Surg. 2011; 91: 750-754 Morgan JA, et al. JHLT. 2013; 32: 1255-1261 INTERMACS Database Additional Data Collection Summary Question 1: Audit of patients with documented moderate/severe AI without a documented AVP to determine if an AVP was in fact performed: Queried: patients=113 hospitals=59 Responded: patients=86 (76%) hospitals=47 (80%) Question 2: Clarification of whether patients with documented AV repairs underwent a closure or a repair: Queried: patients=213 hospitals=62 Responded: patients=143(67%) hospitals=40 (65%) Unconfirmed: patients=70 (33%) hospitals=19 (31%) Total Patients queried = 326 Total Hospitals queried = 88 Total Patients with response = 229 (70%) Total Hospitals responded = 63 (72%) INTERMACS Patient Population: June 2006 – December 2012 All patients implanted as of 12/31/2012 N=7,887 Pediatric Patients: N=79 (patients < 19 yrs of age at time of implant) Adults: N=7,808 Pulsatile Flow: N=1,087 BiVAD N=301 TAH N=158 Continuous Flow: N=6,721 LVAD N=628 Reduced Cohort: Mean Follow-up = 12.3 months Bi VAD: N=179 LVAD: N=6,542 Database Audit Bi VAD: N=140 LVAD: N=5,204 Total Cohort: N=5,344 INTERMACS Patient Population: June 2006 – December 2012 Aortic Valve Closure Aortic Valve Repair • Total=125 • LVAD=121 • BiVAD=4 • Total=95 • LVAD=93 • BiVAD=2 Aortic Valve Replacement All Others • Total=85 • LVAD=83 • BiVAD=2 • Total=5,039 • LVAD=4,907 • BiVAD=132 Survival by Type of Aortic Valve Procedure Performed % Survival No AV Procedure n=5039, deaths=1078 AV Replacement n=85, deaths=24 AV Repair n=95, deaths=22 AV Closure, n=125, deaths=46 Overall p = 0.0003 Months Post Implant Event = Death with a device in place (censored at transplant or recovery) Survival for INTERMACS Level 1-2 Patients by Type of AVP 1 year 56% 76% 67% 79% % Survival Groups AV Closure AV Repair AV Replacement No AVP % Survival post implant n events 6 months 65 25 67% 56 16 85% 37 11 76% 2780 652 85% Overall p=0.003 Months Post Implant Survival for INTERMACS Level 3-7 Patients by Type of AVP % Survival Groups AV Closure AV Repair AV Replacement No AVP % Survival post implant n events 6 months 60 21 85% 39 6 86% 48 13 87% 2258 426 89% Overall p = 0.04 Months Post Implant 1 year 73% 82% 75% 84% Multivariate Model for Death After Implant Risk Factor Hazard Ratio Confidence Interval P-value Aortic Regurgitation 0.98 0.87-1.10 0.75 AV Repair 0.83 0.54-1.27 0.39 AVR 1.36 0.84-2.19 0.21 Closure 1.87 1.39-2.53 <0.0001 INTERMACS Level 1 1.23 1.01-1.51 0.04 Preop Dialysis Dialysis BiVAD BiVAD 1.85 1.32-2.58 0.0003 2.34 2.34 1.8-3.05 1.8-3.05 <0.0001 <0.0001 % of Patients with Moderate/Severe Aortic Regurgitation Recurrence of Aortic Insufficiency Postoperatively by Group 100% Aortic Closure, n=112 Aortic Repair, n=85 Aortic Replacement, n=67 No AV Procedure, n=4,061 90% 80% 70% 60% 50% p (6 months) < 0.0001 40% 30% 18% 20% 10% 0% 8% 5% 1 week 17% 15% 12% 10% 3% 0% 19% 9% 10% 9% 3% 0% 1 month Aortic Closure 7% 6% 3 month Aortic Repair 5% 6 month 12 month Aortic Replacement Note: If the total n for the group is < 20 then it is not plotted in this figure. 18 month 24 month No AV Procedure 27 Question Answered? • Elements of Spouse, Radiologist, Lawyer, clinician answers rolled up into one. • Our study highlights some of the strengths and weakness of the data in INTERMACS • Clinical Question answered but questions remain. – Role of CPB/Cross Clamp – Clinician Bias? – Non Responsive centers- some want in. 28 Thank You to INTERMACS 29