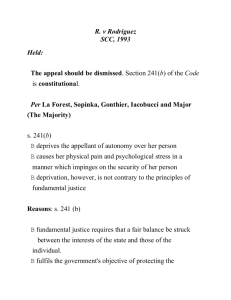
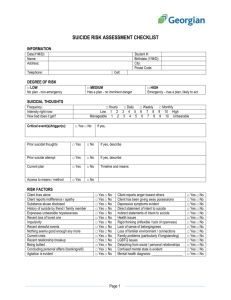
The difficult patient
advertisement

The difficult patient Psychodynamics: Coping styles, defense mechanisms and countertransference Suicide: Assessment of suicide risk and management Consult question • „Sixty-five year old male with end-stage renal disease on hemodialysis. He has been kicked out of all other dialysis centers due to his obnoxious behaviour. He hollers and berates the staff. How to manage his behaviour?“ Difficult patient presents with Vague and generalized somatic symptoms Depression 15% of patients labeled as Anxiety difficult Medication non-adherence A personality disorder Excessive demands and repeated visits Difficult patients evoke strong emotional reactions • • • • Aversion Fear Despair Malice Remember! Medical illness and hospitalization is stressful • Experiencing a medical illness requiring admission is a narcissistic injury: a threat to self-worth or self-esteem • Patient re-examines his self-view while confronting the impermanence of life • Patient feels defective, weak and less desirable • Being in a hospital is very uncomfortable, body exposure, personal and bodily intrusions • Patients are separated from their comfortable environment and have to accept dependency on their caregivers Understand psychodynamic factors Personality structure of the patient: • coping styles: consciously applied behavioral actions • defense mechanisms: unconscious, psychological processes used by patients to deal with reality and to maintaint self-image Emotions experienced by the team: countertransference Personality • Personality types • Personality disorders Continuum Personality types • Personality: a combination of characteristics that predisposes them to think, feel and behave • Inborn: temperament • Environmentally influenced: character Identify personality types Sanguine Melancholic Phlegmatic Choleric Quizz: Have you seen this picture before? a) Yes b) No c) Do not know Personality disorder Individual uses a personality style: • Rigid • Extreme • Maladaptive • Damaging to self or others • Result: impairment in interpersonal, social or occupational domains Coping styles and illness behavior • How an individual manages and attempts to alter stressful situation: consciously applied behavioral actions • Problem-focused: Seeking information, planning, taking action • Emotion-focused: Focusing on positive aspects of the situation, mental or behavioral disengagement and seeking emotional support from others Name positive aspect of the illness and treatment Healthy and adaptive copers • Use combination of problem and emotionfocused copingto deal with a stressor and use different strategies for varied situations • Are optimistic, practical, flexible and composed • View illness as a challenge, strategy, value Poor copers • • • • • Are passive, Deny excessively Hold rigid and narrow views Unable to make decisions Paradoxically they have moments of impulsivity and unexpected compliance • View illness as an enemy, punishment, weakness, relief or irreparable loss Coping style Description Confrontative Hostile or aggressive efforts to alter a situation Distancing Efforts to mentaly detach self from a situation Self-controlling Attempting to regulate one´s feelings or actions Seeking social support Atempting to seek emotional support or information from others Accepting responsibility Accepting a personal role in the problem Escape-avoidance Efforts to escape/avoid a problem or situation, both cognitively and behavioraly Planful problem solving Attempting to come up with solutions to alter a situation Positive re-appraisal Re-framing a situation in more positive light Defense mechanisms • Defenses: used by all individuals to protect the self from anxiety • To provide refuge from a situation with which one cannot currently cope • Psychotic, immature, neurotic and mature What defenses are used by „difficult patients?“ Defense mechanism Mature Humor Description Sublimation Channeling unacceptable impulses into more constructive activities Suppression Intentional exclusion of material from conscioussness Neurotic Displacement Transfer of unacceptable thoughts, feelings or desires from one object to a less threatening substitute Emphasizing the amusing or ironic aspect of the conflict or stressors Isolation of affect Rationalization Separation of painful idea /event from feelings associated with it Reaction formation Repression Immature Acting out Going to the opposit extreme to overcompensate for unacceptable impulses Devaluation Idealization Exagerating negative qualities of others Overestimating the desirable qualities of self or others Passive aggression Projection Indirect and passive expression of anger towards others Regression Reversion of personality to a lower level of expression Splitting Separating people and actions into categories of all good and all bad Psychotic Projective identification Projecting a negative aspect of the self onto another and then coercing the other into identifying with the projected emotion Inventing a socially acceptable and logical reason why one is not bothered Involuntary forgetting of a painful event Performing an action to express unconscious emotional conflicts usually antisocial in nature Attribution of own unaccpetable desires /imulses to another person Psychotic denial Failing to recognize obvious implications or consequences of a thought, act or situation Immature defenses Acting out Description Performing an action to express unconscious emotional conflicts usually antisocial in nature Devaluation Exagerating negative qualities of others Idealization Overestimating the desirable qualities of self or others Passive aggression Indirect and passive expression of anger towards others Projection Attribution of own unaccpetable desires /imulses to another person Regression Reversion of personality to a lower level of expression Splitting Separating people and actions into categories of all good and all bad Immature defenses • Characteristic of the cluster B personality disorders: antisocial, borderline, histrionic, narcissistic • Irritating to others as this defense style transmits patients „shame, impulses and anxiety to those around them“ • Make others suffer (x neurotic defenses cause the self to suffer) Do not confront the patient directly, as defenses are unconscious! Risk of further escalation of oppositional behavior! Identify defenses and understand behaviors • Awareness of the potential for eidealizing/devaluing: Glowing praises follow by harsh criticizing • Awareness of splitting: The patient tend to divide the medical staff as „all good“ or „all bad“ caregivers Physician´s factors and countertransference • Doctor – vs. Patient centered approach? • Strict bio-medical model – vs. Psychosocial approach? • Countertransference: reactions to a patient that represents the past life experiences of the clinician Examples? Management Understand them, recognize the defense mechanisms and coping styles • Ensure that the basic needs of the patient (privacy, food, etc.) including maintaining consistent staff are met. • Attempt to understand and empathize with the patient and acknowledge the real stresses in the current situation (OARS!!!) • Accept the patient´s limitations by not directly confronting immature defenses or poor coping styles • Set firm limits on unreasonable expectations by consistently declaring „in order to provide the best medical care possible….“Reasonable requests should not be refused. Management • Do not directly confront the patient´s entitlement or rage • Gently discuss any irrational fears about the illness or treatment and assess ability for reality testing (transient psychosis?) • Acknowledge and empathize with the primary team´s countertransference. Discuss with them the universality of these emotions. • Use psychopharmacology when appropritate Psychopharmacology • depression and anxiety: SSRI, bupropion, avoid benzodiazepines • insomnia: mirtazapine, trazodone, melatonin • irritability/impulsivity: divalproex, quetiapine, olazapine, risperidone JZ Suicide „There are only two kinds of psychiatrists: those who have had patients commit suicide, and those who will.“ Suicide • No treatment outcome is more devastating than suicide. • Coping with the devastating aftermath – both in MDs and psychotherapists and families: shock, guilt and shame, isolation, grief, dissociation, crises of faith about psychotherapy and other treatments Suicide • • • • 11th leading cause of death in te USA 30 000 suicide attempts are reported annually in the USA 5-6% of attempts occur in hospitals Study of 76 patients who commited suicide on an inpatient psychiatric unit, 78% denied suicide ideation or intent as their last communication • Severe agitation or anxiety was found in 79% of the patients during the week before their suicide Do not rely only on oral reports of patients denying suicidal ideas, but pay closer attention to psychic and motor anxiety as a risk factor. Medical conditions as predictors of suicide • • • • Severe pain Congestive heart failure Seizure disorder Chronic lung disease AS Suicide: Questions • Have you ever felt that life was not worth living? • Did you ever wish you could go to sleep and just not wake up? • Have things ever reached the point where you ´ve thought about harming yourself? • When did you first notice such thoughts? • Have you made a specific plan to harm or kill yourself? • If so, what does the plan include? Source: APA Practice Guidelines for Assessment of Patients with Suicidal behaviors Suicide risk assessment • The presenting suicide ideation and behaviors • Recent suicide ideation and behavior over the preceding 8 weeks • Past suicide ideation and behaviors • Immediate suicide ideation and future suicide plans Suicide risk assessment S sex: male A age: >45, <19 D depression P previous attempts E ethanol abuse R rational thinking loss (psychosis?) S social suppot lacking O organized plan N no spouse S sickness (somatic illness with pain) Management Each positive answer = 1 point Write it to the medical record! • 0-2: low risk • 3-4: medium risk; outpatient treatment, observation • 5-6: high risk; hospitalization, especially in cases without social support • 7-10: very high risk; hospitalization Literature • Amos JJ. And Robinson RG. Psychosomatic Medicine. An introduction to consultationliaison psychiatry. Cambridge, 2010