Biosafety in the TB Laboratory Powerpoint Presentation
advertisement

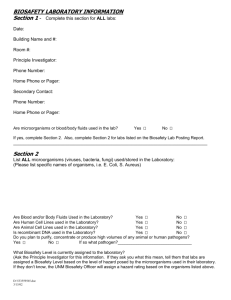
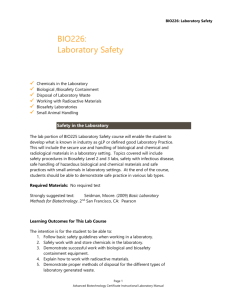
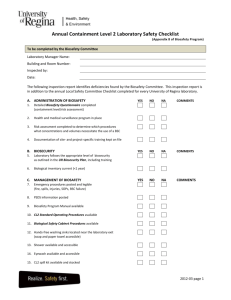
Biosafety in the TB Laboratory Presented by Peggy Coulter with (Patient Safety Monitoring in International Laboratories) Prepared for the ACTG Conference 24 June 2009 Purpose of Training GCLP Standards: DAIDS supported clinical trials and studies involving human subjects must ensure compliance with federal regulations including procedures to protect the safety of all participants. Safety of laboratory employees must be a top priority for all lab facilities. Abbreviations • BMBL- Biosafety in Microbiological and Biomedical Laboratories (CDC) • LBM- Laboratory Biosafety Manual (WHO) • BSC- Biosafety Cabinet • LAI- Laboratory Associated Infection • TB- for Mycobacteriology testing Objectives: At the end of this training you will be able to: • Locate resources for biosafety guidelines; • Describe the elements of biosafety; • Identify standard and special practices in biosafety; • Select and use appropriate biosafety control measures; • Conduct an internal risk assessment and self inspection of the laboratory. Training Topics • • • • • • • • Principles of Biosafety Standard Microbiological Practices Special Practices Personal Protective Equipment Containment Equipment Laboratory Facilities Safety Practices Risk Assessment and Self Inspection Resources for Principles of Biosafety • Biosafety in Microbiological and Biomedical Laboratories (BMBL) from CDC at http://www.cdc.gov/OD/ohs/biosfty/bmbl5/B MBL_5th_Edition.pdf • Laboratory Biosafety Manual from W.H.O. at http://www.who.int/csr/resources/publication s/biosafety/Biosafety7.pdf Introduction to Biosafety All laboratory facilities must follow “Standard or Basic Precautions”. Biosafety guidelines evolved from the microbiological and biomedical community to reduce laboratory associated infections (LIA’s) and to protect the public health and environment. Principles of Biosafety Two basic elements: • Containment • Risk Assessment Routes of transmission for LAI’s • Direct skin, eye, or mucosal membrane; • Parenteral inoculation by a contaminated sharp or needle; • Ingestion of liquid suspension; • Inhalation of infective aerosols. Risk Assessment • • • • • • Pathogenicity of the microorganism Prevalence of tuberculosis and rate of MDR Types of testing performed or referred Volume of tests Personnel expertise and attitude Facilities and equipment WHO Risk Group Risk Microorganism 1 No or low individual and community risk. A microorganism that is unlikely to cause human or animal disease. Moderate individual risk, low community risk. A pathogen that can cause human or animal disease but is unlikely to be a serious hazard to laboratory workers, the community, livestock or the environment. Laboratory exposures may cause serious infection but effective treatment and preventative measures are available and the risk of spread of infection is limited. High individual risk, low community risk. A pathogen that usually causes serious human or animal disease but does not ordinarily spread from one infected individual to another. Effective treatment and preventative measures are available. High individual and community risk. A pathogen that usually causes serious human or animal disease and that can be readily transmitted from one individual to another, directly or indirectly. Effective treatment and preventative measures are not usually available. 2 3 4 Levels of Biosafety, and Testing Levels Testing Level One Two Three Biosafety Level (BSL) Activity 2 •Collect clinical specimens •Transport specimens to a higher level testing laboratory •May prepare and examine smears of killed tubercle bacilli 3 •Level One activities •Process specimens for microscopy and culture •Identify M. tuberculosis •Perform DST on M. tuberculosis 3 •Level One and Two activities •Identify all Mycobacterium species from clinical specimens •Perform DST against all mycobacteria •Conduct research and provide training to other laboratories Basic Microbiology Practices • Policies and access • Safety practices • Decontamination and Waste • Training Specimens Photo of washroom Handling of Specimens • Collection • Transportation • Receipt of incoming specimens • Opening packages Special Practices enhance worker safety, provide environmental protection and address the risk of handling agents requiring increasing levels of containment. Reminder: BSL-3 practices should be used whenever M.tuberculosis is handled even if the physical facilities are a BSL-2. All persons entering the laboratory must be advised of the potential hazards and meet specific entry/exit requirements. Animals and plants not associated with the work being performed must not be permitted in the laboratory. Laboratory personnel must be provided medical surveillance and offered appropriate immunizations for agents handled or potentially present in the laboratory. A laboratory-specific biosafety manual must be prepared, adopted as policy and made available and accessible to the laboratory staff. This is a written plan that defines safe lab practices, spill and emergency procedures The laboratory supervisor must ensure that the laboratory personnel demonstrate proficiency in standard and special microbiological practices before working in the mycobacteriology lab. Personal Protective Equipment (PPE) • Gowns, lab coats • Gloves • Respirators, masks, goggles, glasses • Shoe cover, boots Lab coats vs. Gowns Gloves Approved Type Correct Size Donning Proper Use Removal Shoes and Covers Open-toed footwear is not appropriate in the laboratory. Respirator program implemented by the laboratory's safety officer or person designated to perform this task and should include written procedures concerning how to: a)select the appropriate respirator, b)conduct fit-testing, and c)train personnel on the use, fit checking, and storage of the respirator. Correct Type and Fit of Respirators Dust Dust and Paint Fumes N-95 Surgical Mask PAPR Safety Equipment • • • • Needle locking syringes Centrifuge safety carriers Microburners Biosafety Cabinets (BSC) Centrifuge Safety Biosafety Cabinets (BSC) All procedures involving the manipulation of infectious materials must be conducted within a BSC, or other physical containment devices. No work with open vessels is conducted on the bench. When a procedure cannot be performed within a BSC, a combination of personal protective devices, such as centrifuge safety cup with sealed rotor, must be used. Use of BSC A BSC is the most important piece of containment equipment but only • if properly installed, • appropriate air velocity is maintained during use, • proper procedures are used. Use of biological safety cabinets Facilities –Ventilation –Temperature control –Sinks, eyewash, trashcans –Furniture and decontamination Plan of a culture laboratory Handling of contaminated laboratory supplies • Glassware • Sputum containers • Applicator sticks, paper, pipettes • Positive and negative slides Waste Handling Potentially infectious materials must be placed in a durable, leak proof container during collection, handling, processing, storage, or transport within a facility. No infected material should leave the laboratory except when it is properly packed for transport to another laboratory. Cleaning laboratory materials Disinfection and Sterilization A basic knowledge of disinfection and sterilization is crucial for biosafety in the laboratory. Laboratory equipment should be routinely decontaminated, as well as, after spills, splashes, or other potential contamination. Autoclaves Boiling and burning Safety Practices • Pipetting • Microscopy • Handwashing Handwashing Training Initial on hire Annual updates Staff should be observed in their biosafety practices Laboratory safety does not just happen. The best defense against a laboratory accident is a well-thought-out plan to neutralize its effects as quickly and effectively as possible. • recognize that accidents can and will occur • formulate a plan of action • discuss ways to minimize and prevent accidents Spill Procedures Laboratory accidents in the TB laboratory result in possible formation of aerosols. Spills involving infectious materials must be contained, decontaminated, and cleaned up by staff properly trained and equipped to work with infectious material. Emergency Procedures • Puncture wounds, cuts and abrasions • Ingestion of potentially infectious material • Potentially infectious aerosol release (outside a biological safety cabinet) • Broken containers and spilled infectious substances • Breakage of tubes containing potentially infectious material in centrifuges not having sealable buckets • Breakage of tubes inside sealable buckets (safety cups) Incidents that may result in exposure to infectious materials must be immediately evaluated and treated according to procedures described in the laboratory biosafety manual. All such incidents must be reported to the laboratory supervisor. Medical evaluation, surveillance, and treatment should be provided and appropriate records maintained. Support Staff The safe and optimum operation of a laboratory is dependent to a great extent on the support staff, it is essential that such personnel are given appropriate safety training. THE MYCOBACTERIOLOGY LABORATORY IN NEED OF IMPROVEMENT Physical facilities BSL-2 vs BSL-3 Laboratory Inspection • • • • Engineering controls Administrative controls Personal protective equipment General Laboratory Safety Risk Assessment Will evaluate all procedures for risks related to aerosol generation and injury from contaminated sharp objects (e.g., needle sticks) and develop a strategy for safe, stepby-step manipulation of both specimens and cultures. Why an assessment? Who should perform it? When should it be done? What tools are used? How should it be done? Potential Hazards: The following slides show some improper biosafety practices or containment safeguards found in some TB laboratories. Summary Although the incidence of tuberculosis is higher in laboratory workers than for the general population, the risk of becoming infected with M. tuberculosis in the laboratory can be minimized through the use of the engineering controls, administrative procedures, and specific work-place practices that are presented in these guidelines. Questions? Resources • www.psmile.org • www.asm.org • www.clsi.org • www.cdc.gov • www.who.int./csr/resources/publi cations/biosafety/en/Biosafety7.pdf