Who gets IBD and WHY

Who gets IBD and Why?
Dr Miles Parkes, Cambridge
Dr Hannah Gordon, London
RSM and CCUK® 2015
Introduction
• Who?
• Epidemiology
• Why?
• Heritability – twin and family studies
• Genetics
• Environment
• Interface between Genes and Environment
• Microbiota
• Epigenetics
Prevalence
• UK prevalence 4/1000
• 620,000 affected within the UK (IBD Standards, CCUK® 2015)
Age
• All ages affected
• Peak incidence 15-30 years
• 2 nd peak 50-80 years
• Incidence rising in children
(Henderson 2012)
Sex
Men and women are affected almost equally
Race
Traditionally a disease of the West, rates of IBD remain high in Western
Europe and North
America (Cosnes
2011).
However all countries are affected with incidence rapidly rising in Asia.
Highest incidence of IBD in the World
Faroe Islands – 80 per 100,000 new cases diagnosed per year
Ethnicity and affluence
• Ashkenazi Jews
• Caucasians
• Socio-economic status
• Previously thought to be associated with affluence
• Not replicated in all studies
Is Inflammatory Bowel Disease Heritable?
Heritability is the extent to which a trait is caused by our genes
How can we estimate heritability of IBD?
Family studies Twin studies
Calculating extent identified genes explain IBD prevalence
Family studies
The greatest single risk factor for developing IBD is having one or more first degree family members diagnosed
Odds Ratio sibling risk vs population risk:
• CD 25-42
• UC 4-15
However, family history only reported in 5-16% IBD patients
Family studies
IBD in families shows concordance in
• Behaviour
• Location
• Age of onset
IBD in families tends to present earlier and be more severe
BUT Families share similar environment as well as similar genes…..
Twin studies
Why?
• Both identical and nonidentical twins share similar environment
• Identical share genetic code, twice as genetically similar
How?
• Concordance of identical and non-identical twin pairs are compared
Difference between identical and non identical groups is crucial – ie almost all twin pairs share a history for chickenpox, but this is not inherited!
UK Twins with IBD:
Pair concordance (UK IBD TAM 2014)
Previous twin cohorts (Tysk et al 1988, Halfvarson 2007, Brant 2011)
Monozygotic
Dizygotic
Crohn’s Disease
20-55%
0-3.6%
Ulcerative Colitis
3.6-17%
0-6.3%
Genetic Studies
• Compare the genomes of people with IBD vs people without
IBD
=> identify gene variants associated with IBD
=> work out functional impact + how they predispose to IBD
(role for IBD Bioresource)
=> 1. clues re environmental triggers
2. ? ‘druggable’ targets
Genome Wide Association Scanning
=> Unbiased survey of whole genome
• Genotype >0.5 million markers in thousands of cases + controls
• Use stringent statistics to identify ‘associated’ SNPs i.e. with significantly different allele frequencies in cases vs controls
• Identify genes mapping to same region
• Study impact of associated gene variant on protein function in relevant cell type
UKIBDGC and IIBDGC GWAS Studies
GWAS studies in IBD
Jostins et al Nature 2012: International IBD Genetics Consortium
GWAS meta-analysis + Immunochip deep replication
163 discrete risk loci identified
Immunchip - 14,763 CD / 10,920 UC / 15,977 control subjects
GWAS - 6,333 CD / 6,687 UC / 15,056 control subjects
163 genes and loci: What have we learned?
Large overlap between UC and CD
Jostins et al. Nature 2012
IFNgamma
Th 1
STAT4
IL23R pathway
Duerr et al Science 2006;
Parkes et al Nature Genet 2007;
Barrett et al Nature Genet 2008;
Franke et al Nature Genet 2010.
IL-17
IL-6
TNF alpha
IL-12 p35 p40
IL-23 p19 p40
Naive CD4+ve T Cell
CCR6
Th 17
STAT3
JAK2
ICOS
ICOSL
McKenzie et al.
TRENDS in Immunology 2006:27(1), 17-23
Clinical impact…
A pipeline for drug discovery
Genes discovered ‘early’ have biggest effect: Odds ratio for CD according to NOD2 genotype
Hugot
Ogura
Hampe
Ahmad
Heterozygote
3
1.5
2.6
2.4
Homozygous
38
Compound
Het
44
17 § only
42 § only
9.8 29.3
NOD2 not assoc with UC
NOD2 domains & mutations
CARD 1 2 NBD
*
* non-synonymous
§ frameshift - premature stop
3 main mutations – all in LRR domain
LRR
* §
Autophagy
ATG16L1
• ATG16L1 – a key component of autophagy
• independent discovery in German, N American (NIDDK) and UK (WTCCC) CD GWA panels
• Hampe et al Nature Genetics 2007
• Rioux et al Nature Genetics 2007
• WTCCC Nature 2007
Association at IRGM – another autophagy gene
Parkes et al. Nature Genetics 2007
The power of hypothesis-free GWAS
• 2 genes in same (previously unsuspected) pathway associated with CD susceptibility
= ATG16L1 and IRGM
Autophagy
Phagophore lysosome
AH cytoplasm
Autophagosome
AH
Autophagolysosome
• T300A
↑↑ cleavage of ATG16L1 by caspase 3 when latter is activated through TNF / metabolic / infection stress
↓↓ xenophagy
disrupted pathogen elimination
Murthy et al Nature 2014
GWAS studies in UC
UC-specific
• Epithelial barrier loci -
– HNF4a
– E-cadherin...etc
Franke et al Nat Genet 2009
Fisher et al Nat Genet 2008
Silverberg et al 2009
UKIBDGC / WTCCC Nat Genet 2009
Epithelial barrier
• Increased permeability as risk for IBD
• Allows commensals to breach epithelial barrier and activate mucosal immune system
• Questions:
• Why UC-specific?
• What leaks through?
Overlap with other diseases
... implicates Mycobacterial infection as a evolutionary selection pressure for IBD?
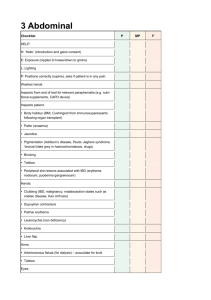
Disease
Ankylosing spondylitis
Psoriasis
Atopic dermatitis
Primary sclerosing cholangitis
Primary biliary cirrhosis
Rheumatoid arthritis
Celiac disease
Type 1 diabetes
Systemic lupus erythematosus
Multiple sclerosis
Asthma
Fold enrichment
10.1
10.1
9.9
9.9
8.1
7.6
13.7
13.4
12.2
11.6
10.8
Jostins et al. Nature 2012
Rapid rise in IBD suggests environment is critical
Genes
Environment
Rise of IBD in the East
2-3 fold increase in IBD incidence in past 10-20 years in several Asian countries
Mirrors increase seen in Western countries 50 years ago
More UC, although CD rapidly increasing
Only 3-10% report family history of IBD
Far outweighs what can be explained by new genetic mutations
Migration studies
Higher rates of IBD in Asians in Western Europe, Australia, Northern
America
Second generation Asian migrants in Leicestershire had UC rates comparable to Caucasian British
Disease is as if not more severe, more likely to affect men, and less likely to affect outside the gut
Why the increase in Asia
Westernisation of lifestyle
•Diet
•Hygiene
•Infection
Medication
• Aspirin
• NSAIDS
• Oral
Contraception
• Antibiotics
Lifestyle
• Smoking
• Diet
• Low Exercise
• Stress
Environmental factors
Early
Environment
• Emergency
Caesarian
• Breastfeeding
Health
• Childhood illness
• Gastrointestinal infection
• Atypical
Mycobacterium
• Appendicectomy
Diet
Read made meals
Polyunsaturated fats
High sugar
Low vegetable
Low fruit
Low fibre
Problems interpreting data on environmental factors
Correlation not cause and effect
Results vary between studies
Each factor conveys a relatively modest risk
Risk factors often not avoidable
Important to avoid guilt or blame
The Microbiome
100 trillion bacteria within gut
10x more cells than human body
Complex ecosystem
Implicated in health of all other organs
• Cardiovascular disease
• Depression
• Obesity
• Inflammatory Bowel Disease
HMP Nature 2013
• Significant variation between individuals re taxa / species
• BUT – key metabolic pathways are VERY stable in health
What influences composition of microbiota?
Genetics
Race
Early environment
Smoking
Diet
Antibiotics
Infection
Method of delivery
The microbiota influence mucosal immune development and homeostasis – disturbance may contribute to development of IBD.
Dysbiosis in Crohn’s Disease – incl ↓ diversity
Increased in CD
Sokol et al PNAS 2009
Decreased in CD
Gevers et al Cell Host and Microbe 2014
Is the bacterial dysbiosis secondary to bacteriophage ‘bloom’?
What functional elements are being transferred?
What impact on host immunity?
Norman et al. Cell 2015
The Microbiota and IBD
• Unclear whether changes happen before or after disease develops
• Cause or correlation?
Can we change the microbiota?
• Yes!
• Dietary change from vegan to exclusively meat and dairy changes microbiota substantially in days
• Some changes associated with meat diet were same as those associated with
IBD
• Smoking cessation changes microbiota
• However
• Once IBD has developed, prebiotics, probiotics and faecal transplant not yet shown to be a cure
Epigenetics
Epigenetics: programmed regulation of gene expression in response to environmental factors
Epigenetic changes associated with CD and UC have been found in gut biopsies and blood
Twin studies underway to further investigate
Conclusion:
• Anyone can get IBD
• Increased risks
• Genetic susceptibility
• Environmental triggers
• Dysbiosis of microbiota
• Epigenetic change
• Why important to understand?
• Prevention
• Prediction and early diagnosis
• Novel targets for treatment
The Jesse and Thomas TAM Family
Foundation
UK IBD Genetics
Consortium