Safety Attitude Questionnaire: Unit

Welcome to the Leadership for Safety Webinar
Safety Attitude Questionnaire:
Unit-Level Results on Teamwork and Non-Punitive
Response to Error
The webinar will be starting momentarily…
If you are having technical difficulties please contact 202-495-3356 or ltiscornia@naph.org
Chat Box
Please use the Chat Box on the webinar screen to type your question or comment at any time.
NOW: Use the Chat Box to sign in.
Enter your organization and names of all people in the room.
Agenda for Today’s Webinar
• Unit-level COS results from San Francisco General
Hospital, and UT Tyler
• Unit by unit COS data, resilience, and readiness for change
• Run chart “poster session”
• Next month’s focus: Just Culture – How to know whether to hold an individual to account for a safety mishap.
Who is on Today’s Call?
Sue Currin, MS, RN
Jim Reinertsen, MD
Bart Hill, MD, MPA
St. Luke’s Treasure Valley
St. Luke’s Regional Medical Center
St. Luke’s Meridian Medical Center
Cook County Health & Hospitals System
John H. Stroger, Jr. Hospital
Provident Hospital San Francisco General Hospital and Trauma Center
Contra Costa Regional Med. Center
Alameda County Medical Center
Santa Clara Valley Health and Hospital System
San Mateo Medical Center
Truman Medical Centers
TMC- Hospital Hill
TMC- Lakewood
Los Angeles County Department of Health Services
Harbor-UCLA Med Center
LAC+USC Healthcare Network
Rancho Los Amigos National
Rehab. Center
Regional Medical Center at Memphis
Kimberly Horton, DHA,
MSN, FNP, RN, FACHE
Maricopa Medical Center
UT-Health Science Center at Tyler
Univ. Medical Center of El Paso
Harris County Health System
Ben Taub General
LBJ Hospital
Quentin Mease
LSU-HCSD
Interim
Bogalusa
Alfred Connors, MD
MetroHealth
Thomas Holton, MS, RN
David Coultas, MD, FACP
Jill Steinbruegge, MD, PhD
Bianca Perez, PhD
Arielle Gorstein
Leadership Summit staff
Guest speakers on today’s call
University of Texas – Tyler
Comparative Results By Unit
Teamwork Across Units
Unit 1 2012
1. Hospital units do not coordinate well with each other.
Database
Your
Hospital
36
33
Database
2. There is good cooperation among hospital units that need to work together.
3. It is often unpleasant to work with staff from other hospital units.
Your
Hospital
Database
Your
Hospital
4. Hospital units work well together to provide the best care for patients.
Database
Your
Hospital
Teamwork Within Units
1. People support one another in this unit.
Database
Your
Hospital
2. When a lot of work needs to be done quickly, we work together as a team to get the work done.
Database
Your
Hospital
48
33
50
58
58
58
Unit 1 2012
84
92
86
3. In this unit, people treat each other with respect.
Database
Your
Hospital
4. When one area in this unit gets really busy, others help out.
Database
Your
Hospital
Nonpunitive Response to Error
1. Staff feel like their mistakes are held against them.
Database
Your
Hospital
2. When an event is reported, it feels like the person is being written up, not the problem.
Database
Your
Hospital
3. Staff worry that mistakes they make are kept in their personnel file.
Database
Your
Hospital
85
74
77
67
69
Unit 1 2012
43
58
38
62
28
31
Unit 1 2010
36
45
46
55
49
45
56
64
Unit 1 2010
84
73
86
73
74
50
67
36
Unit 1 2010
43
36
38
36
27
36
Difference
-12
-22
13
-6
Difference
19
12
27
33
Difference
22
26
-5
Unit 2
2012
Unit 2
2010 Difference Unit 3 2012 Unit 3 2010 Difference Unit 4 2012 Unit 4 2010 Difference Unit 5 2012 Unit 5 2010 Difference
43
33
39
55 -22
44
35
43
14 21
48
100
46
60 40
41
75
39
65 10
57
56
63
53
64
62
-8
58
50
61
56
43
60
7
63
80
64
60
80
64
0
55
75
56
54
52
55
23
75
66
73
63
2 47
66
53
65
-6 80
71
80
69
0 92
65
71
63
21
63
Unit 2
2012
89
36 27
Unit 2
2010
89
Difference
57 47
Unit 3 2012
85
Unit 3 2010
84
10 100 100 0 92 62 30
Difference Unit 4 2012
92
Unit 4 2010
92
Difference Unit 5 2012
83
Unit 5 2010
83
Difference
100
90
100
90
0 82
81
81
81
1 100
90
100
89
0 100
86
78
86
22
100
80
100
80
0 85
77
75
76
10 100
88
100
87
0 100
73
87
73
13
33
43
33
31
100
77
100
77
0 85
64
75
62
10 100
77
100
75
0 100
65
74
65
26
67
Unit 2
2012
46
67
Unit 2
2010
46
0
Difference
52 56
Unit 3 2012
46
Unit 3 2010
46
-4 100 100 0 100 52 48
Difference Unit 4 2012
64
Unit 4 2010
64
Difference Unit 5 2012
48
Unit 5 2010
49
Difference
-12 13 -20 11 45
41
27
30
6
38
44
45
32
25
42
6
31
39
80
62
40
52
100
61
60
50
-20
50
46
50
35
39
46
43
34
7
25 18 7 15 6 9 80 20 60 42 48 -6
Unit by Unit COS data, Resilience, and Readiness for Change
7
9
From Bryan Sexton
Key Domain One: Teamwork
Driven by Answers to Six Questions
1.
Nurse input is well received in this clinical area.
2.
In this clinical area, it is difficult to speak up if I perceive a problem with patient care.
3.
Disagreements in this clinical area are resolved appropriately (i.e., not who is right, but what is best for the patient).
4.
I have the support I need from other personnel to care for patients.
5.
It is easy for personnel here to ask questions when there is something that they do not understand.
6.
The physicians and nurses here work together as a well-coordinated team.
10
A poor teamwork score (less than 60% reporting positive teamwork)…
• Results from persistent interpersonal dysfunction on the unit
• Predicts operational outcomes e.g. staff turnover, delays, etc.
Needs a specific leadership response: If teamwork score is low, find out which of the questions is dragging the score down and address that issue specifically
Key Domain Two: Safety Climate
Determined by scores on seven questions:
1. I would feel safe being treated here as a patient.
2. Medical errors are handled appropriately in this clinical area.
3. I know the proper channels to direct questions regarding patient safety in this clinical area.
4. I receive appropriate feedback about my performance.
5. In this clinical area, it is difficult to discuss errors.
6. I am encouraged by my colleagues to report any patient safety concerns
I may have.
7. The culture in this clinical area makes it easy to learn from the errors of others.
Poor safety climate scores (<60%)…
• Predict poor clinical outcomes, and high staff injury rates
• Result from perceived lack of commitment to safety by leadership
• Leadership response: demonstrate eagerness to learn about safety problems, and willingness to do something about them
Key Support Domain: Resilience (Burnout)
Determined by scores on four questions:
1.
I feel fatigued when I get up in the morning and a have to face another day on the job
2.
I feel burned out from my work
3.
I feel frustrated by my job
4.
I feel I am working too hard on my job
Leadership Response:
For units with HIGH resilience, you can go ahead with a new initiative even if safety or teamwork scores are low (but you will need to address the specifics of why these scores are low)
For units with low resilience AND low teamwork/safety climate scores, you must first deal with the burnout issues before you can hope to accomplish
ANY change initiative.
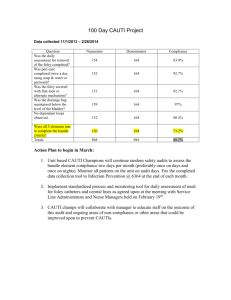
The MetroHealth System
Run charts for 2010, 2011, 2012 for
VAP, CLBSI, and CAUTI
10
0
ICU
Non-ICU
40
30
20
60
Catheter Related Bloodstream Infections (CLBSI),
2010 to 2012
2.91*
2.58* *infections per 1000 catheter days
50
2010
14
40
2011
23
28
1.86*
2012
10
25
16
Total Hospital Acquired Catheter Related Bloodstream Infections
(ICU and non-ICU, 2010 to 2012)
15
14
13
12
11
10
9
8
7
4
3
6
5
2
1
0
2
0
4 4 4
14
0
4
1
8 8
4
1
5
3 3
5
2 2
1
8
7
5
3
6
2
4 4
3
9
1
2
6
1
2
1 1
3
17
40
30
20
60
50
10
0
VAP
Ventilator Associated Pneumonia (VAP)
2010 to 2012
4.81*
4.69*
*pneumonias per 1000 ventilator days
4.14*
2010
51
2011
51
2012
35
18
8
7
6
5
4 4
3
2
1
0
1
2
5 5
7 7
5
4
7
Ventilator Associated Pneumonia
2011 to 2012
3
1
7
5
4
5
6
5
3
6
5
2
0
3
2
3
7
1
3
4
3 3
4 4
1
10
Jul-10
11
Jul-11
12
Aug-12
19
180
160
140
120
100
80
60
40
20
0
CAUTI
Catheter Associated Urinary Tract Infection (CAUTI)
2010 to 2012
8.71*
2010
167
4.12*
2011
119
*infections per 1000 catheter days
3.11*
2012
76
20
40
Catheter Associated Urinary Tract Infections (CAUTI)
(ICU and non-ICU)
Change in CAUTI definition
36
35
33
30
25
20 20
27
26
23
29
31 31
24
28
23
19
16 16
15
10
5
7
13
11
6
10
8
7
10 10
7
4
7
6
3
4
8
5
3
4
9
0
0 1 2
21
250
200
150
100
50
0
Total BSI, VAP, UTI
2011 to 2012
51
51
118
2011
CAUTI CLBSI VAP
34% reduction
2011 to 2012
35
35
75
2012
Total BSI, VAP and CAUTI
2011 to 2012
40
35
34
30
25
20
15
10
5
0
16
22
25
15
18
23
30
16
13
18
13
14
17
26
22
7
16
12
17
9
12
13
Total VAP, CLBSI, & CAUTI Linear (Total VAP, CLBSI, & CAUTI)
23
Next Month:
Tuesday February 12 th 8am PT/9am MT/10am CT/ 11am ET
Just Culture
1. Have a brief conversation with the chief nurse, or the head of HR, and ask the following questions:
Did we initiate disciplinary action against any staff member (nurse, pharmacist, physician, nursing assistant…) because of a safety mishap in the last year?
If yes…by what method did we decide that this was a problem with the individual? What is our method for determining individual culpability for safety mishaps?
2. Be prepared to discuss what you’ve learned about your organization and how it decides when to hold people to account for their safety behaviors.
Just Culture Algorithm, HR protocols, or other document