Incidental pancreatic cyst Differential Neoplastic vs. inflammatory
advertisement
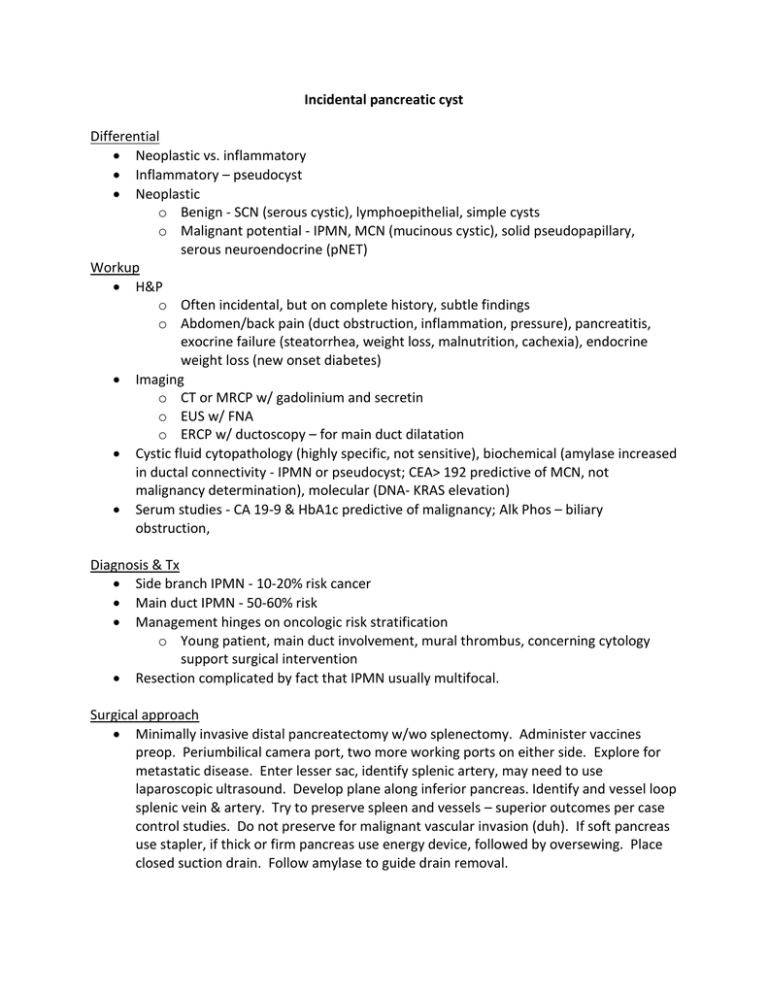
Incidental pancreatic cyst Differential Neoplastic vs. inflammatory Inflammatory – pseudocyst Neoplastic o Benign - SCN (serous cystic), lymphoepithelial, simple cysts o Malignant potential - IPMN, MCN (mucinous cystic), solid pseudopapillary, serous neuroendocrine (pNET) Workup H&P o Often incidental, but on complete history, subtle findings o Abdomen/back pain (duct obstruction, inflammation, pressure), pancreatitis, exocrine failure (steatorrhea, weight loss, malnutrition, cachexia), endocrine weight loss (new onset diabetes) Imaging o CT or MRCP w/ gadolinium and secretin o EUS w/ FNA o ERCP w/ ductoscopy – for main duct dilatation Cystic fluid cytopathology (highly specific, not sensitive), biochemical (amylase increased in ductal connectivity - IPMN or pseudocyst; CEA> 192 predictive of MCN, not malignancy determination), molecular (DNA- KRAS elevation) Serum studies - CA 19-9 & HbA1c predictive of malignancy; Alk Phos – biliary obstruction, Diagnosis & Tx Side branch IPMN - 10-20% risk cancer Main duct IPMN - 50-60% risk Management hinges on oncologic risk stratification o Young patient, main duct involvement, mural thrombus, concerning cytology support surgical intervention Resection complicated by fact that IPMN usually multifocal. Surgical approach Minimally invasive distal pancreatectomy w/wo splenectomy. Administer vaccines preop. Periumbilical camera port, two more working ports on either side. Explore for metastatic disease. Enter lesser sac, identify splenic artery, may need to use laparoscopic ultrasound. Develop plane along inferior pancreas. Identify and vessel loop splenic vein & artery. Try to preserve spleen and vessels – superior outcomes per case control studies. Do not preserve for malignant vascular invasion (duh). If soft pancreas use stapler, if thick or firm pancreas use energy device, followed by oversewing. Place closed suction drain. Follow amylase to guide drain removal. Special considerations – For positive margins in main duct IPMN: in fit patients resect more pancreas to total pancreatectomy if necessary. In unfit patients resect more if possible, but weigh risk/benefits of total pancreatectomy. In side-branch IPMN remove most threatening lesions, if positive margin/multiple lesions may leave in unfit patients/reassuring radiological characteristics. Postoperative management 15-25% pancreatic fistula rate, may present late, even after discharge. Look for tachycardia, delayed return of bowel function, abdominal pain. Long term survival dictate by status of remnant gland, pathology of primary lesion o Unifocal, low grade, radiologically -ve/+ve remnant Yearly H&P, CT/MRCP, serum studies o High grade dysplasia, +ve low grade main duct margin, new lesion in previously negative remnant At least biannual H&P, CT/MRCP, serum studies At least annual EUS-FNA w/ cytopathology to monitor recurrence or progression