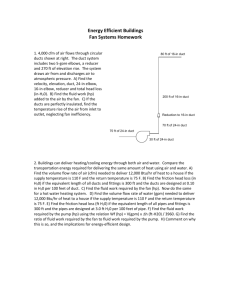
Congenital Heart Disease
advertisement
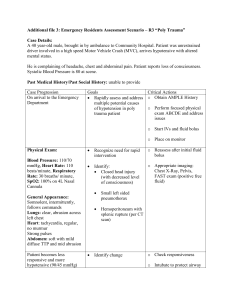
1 Duct Dependant Congenital Heart Disease – Anaesthetic Principles Communication is key – ensure Consultant Paediatrician, Anaesthetist and PICU all involved. Background These babies depend on maintaining a patent ductus arteriosus to sustain adequate systemic perfusion. They present at or shortly after birth as the duct starts to close. Keys to management depend on supportive treatment, maintaining duct patency and close early liaison with PICU/Cardiology. Some of the babies with low oxygenation and/or persistent severe shock may need emergency atrial septostomy and hence transfer to cardiovascular surgical centre is time critical. Suspect if: Clinical presentation first few days of life May have been suggested on ante-natal US scanning Difficulty feeding secondary to breathlessness Cyanosis unresponsive to supplemental oxygen Weak or absent femoral pulses Hepatomegaly A murmur (but absence does not exclude diagnosis) Airway & Breathing May require intubation if Recurrent apnoeas Shock Respiratory failure N.B. All induction agents will drop cardiac output to some extent therefore ensure adequate IV acess and fluid boluses ready to give. Post intubation ensure Paralysed and ETT strapped securely Aim to ventilate in air. (Oxygen acts to close the duct). Supplemental oxygen may be required to keep SpO2 75-80% CXR (Check ETT position and evidence of cardiac failure e.g. cardiomegaly Monitor pre-ductal (right hand) and post-ductal (either foot) oxygen saturations. Ver. 1. Nov 2014 2 Circulation Ensure 2 x IV access (umbilical vein cannulation may be an option paediatricians may be able to help) Treat hypotension with 10ml/kg of isotonic solution and evaluate response to further fluid boluses. If hypotension persists after 20 mls/kg of fluid bolus, start dopamine infusion initially (can go peripherally) or adrenaline as 2nd line (ideally centrally or IO) Commence dinoprostone infusion (PGE2) at 5-10ng/kg/min (see Cardiff drug calculator) to maintain duct patency. Side effects include: o Apnoeas (likely to require intubation) o Hypotension o Fever N.B. Do not use Prostacyclin, Epoprostenol or Flolan – these are all pulmonary vasodilators and DO NOT maintain ductal patency Other Check blood glucose regularly (due to risk of hypoglycaemia) Ensure 12 lead ECG is performed Start empirical antibiotics (Cefotaxime and Amoxicillin) after blood culture, as one of the differential diagnosis for cyanosis and shock in newborns is sepsis with Persistent Pulmonary Hypertension. Ver. 1. Nov 2014