Statement from the Growth Hormone Research Society
advertisement

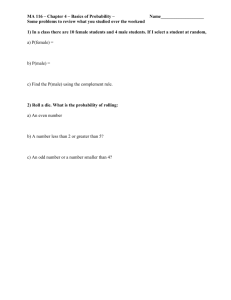
Keswick Safety Presentation-final2.ppt 6-19-00 Statement from the Growth Hormone Research Society Keswick Hall Charlottesville, Virginia May 7 - 10, 2000 Critical Evaluation of the Safety of Recombinant Human Growth Hormone Administration • Background • Epidemiological and experimental data used to assess relationships of GH, IGF-I and cancer risk • Safety aspects – GH therapy in children – GH replacement in adults – Pharmacological GH treatment in adults • Closing remarks Participants Robert Baxter Raymond Hintz Akira Shimatsu Bengt Åke Bengtsson Jörgen Isgaard Peter H. Sönksen Sandra L. Blethen Gudmundur Johannsson Peter Stein Werner F. Blum Jens Otto Lunde Jørgensen Christian J. Strasburger Bjorn Carlsson Anne-Marie Kappelgaard Elisabeth Svanberg Lena Carlsson Irene Langbakke Anthony Swerdlow Paul V. Carroll Derek LeRoith Katsuhiko Tachibana Jens Sandahl Christiansen Barbara Lippe Hiroaki Takahashi Peter E. Clayton Saul N. Malozowski Jukka Takala David R. Clemmons Thomas Maneatis Toshiaki Tanaka Pinchas Cohen John P. Monson Michael O. Thorner Christopher T. Cowell Yoshikazu Nishi Greet van den Berghe Gordon B. Cutler Michael N. Pollak A.J. van der Lely Judith E. Fradkin Iain Robinson Patrick Wilton Joseph M. Gertner Ron Rosenfeld Douglas Yee Sue Hankinson Daniel E. Salazar Background • Lessons learned since recombinant human GH was introduced to the market in 1985 • Unprecedented level of scrutiny has lasted more than 15 years because – Jacob Creutzfeld disease relationship to pituitary-derived GH – Potential association between GH and leukemia – GH was the second recombinant protein brought to market Epidemiological and experimental data used to assess relationships of GH, IGF-I and cancer risk Epidemiological Data Active acromegaly, a disease characterized by raised serum GH, IGF-I, and IGFBP-3 levels has been reported to be associated with • increased incidence of colonic neoplasia, although conflicting data exist • no increased incidence of breast or prostate cancers Epidemiological Data Recent epidemiological surveys, including case-control, as well as follow-up designs report • Serum IGF-I levels in upper normal range may be associated with increased risk of developing prostate cancer and breast cancer in premenopausal, but not postmenopausal women • High IGF-I and low IGFBP-3 levels in serum may be associated with increased risk of these two tumors, as well as risk of colon cancer • High serum IGFBP-3 levels alone have also been related to reduced cancer risk Epidemiological Data Consensus regarding background information • A cause-effect relationship between serum IGF-I and development of cancer has not been demonstrated • Serum IGF-I levels may be affected by additional factors other than GH status, including nutrition Experimental Data Studies in vitro and in animal models • Most cells, including cancer cells, possess IGF-I receptors and respond to IGF-I with increased growth • IGF binding proteins (IGFBP) and IGFBP proteases also modulate cell growth, and over expression of IGF-I receptors induces tumor formation in animal models • No evidence that systemic administration of IGF-I to animals stimulates tumor formation, although it can increase growth of some established tumors Experimental Data Studies in vitro and in animal models No studies have evaluated direct (IGF-independent) effects of GH on tumor formation • In GH transgenic animals, specific activation of GH receptors with concomitant elevations in circulating IGF-I did not result in breast, colon or prostate tumor formation Epidemiological Data GH Replacement and Cancer Risk • No data to suggest that IGF-I and IGFBP-3 modulate cancer risk in GH-treated patients • Patients with previous malignancies or history of radiation therapy carry significant risk for recurrence and second malignancy • Recommend measurement of serum IGF-I levels in patients receiving GH treatment; place of regular IGFBP-3 monitoring is not defined • Recommend that IGF-I level be maintained within appropriate age- and gender-related normal range in GH-deficient adults during long-term therapy Epidemiological Data Regulatory Aspects • Current labeling for GH states that active malignancy is a contraindication for GH treatment. There are, however, no data to support this labeling. • Current knowledge does not warrant additional warning about cancer risk in the product label. Safety - GH Therapy in Children Recombinant human GH has been used in an estimated 50,000 children. • Significant adverse drug reactions rare • Large international databases have been useful in quantifying adverse events, and hence, addressing safety issues • Extended follow-up into adulthood of children who have discontinued GH treatment would be ideal - this may only be achievable in subset of patients Safety - GH Therapy in Children Malignancy Risk Children receiving GH, who have had a malignancy, account for approximately 20% of patients enrolled in international databases. • Existing evidence does not indicate that GH treatment will increase tumor recurrence in those successfully treated for their primary lesion • In patients who have been rendered GH deficient by tumor and/or its treatment, timing of initiation of GH treatment must be decided on basis of individual case, once tumor treatment is completed and condition is in remission Safety - GH Therapy in Children Malignancy Risk All subjects who have had a malignancy and received treatment for it are at risk for a second malignancy. • No evidence that GH treatment increases risk of this process based on limited data available • No evidence that de-novo cancer and leukemia are increased in GH recipients • In view of continuing evolution of oncology treatments, ongoing surveillance of GH recipients with appropriate age-related controls is important Safety - GH Therapy in Children Malignancy Risk Certain patient groups who receive GH treatment carry an intrinsic risk of developing malignancies, including those with Neurofibromatosis type 1, Fanconi anemia, Downs and Bloom syndromes. • Although no evidence that GH replacement poses increased cancer risk, we recommend that such children be carefully monitored with regard to tumor formation Safety - GH Therapy in Children Benign Intracranial Hypertension • Has been reported in 1/1000 children receiving GH treatment; may be underestimate • Headache in children on GH treatment should be carefully evaluated • Fundoscopic examination should be performed before initiation of GH treatment and repeated when clinically indicated Safety - GH Therapy in Children Glucose Metabolism • Reduction of insulin sensitivity is physiologic effect of GH, however, glucose homeostasis is maintained in vast majority of patients • Most available surveillance data do not demonstrate increased incidence of diabetes, either type 1 or type 2, associated with GH treatment • There are, however, subgroups of patients inherently at risk of developing diabetes - these should be carefully monitored Safety - GH Therapy in Children Glucose Metabolism • Diabetes mellitus is not contraindication to GH treatment in children • Diabetic care should follow standard clinical practice Safety - GH Therapy in Children Skeletal Disorders • Some underlying disorders that are treated with GH therapy can be associated with slipped capital femoral epiphysis, scoliosis and avascular necrosis • No evidence these conditions are caused by GH treatment; however, scoliosis may be exacerbated when growth is accelerated Safety - GH Therapy in Children Interaction with Other Hormones • No compelling evidence that GH treatment has any adverse effect on pubertal development and gonadal function • GH can affect metabolism of thyroid hormones and cortisol Safety - GH Therapy in Children GH Treatment and Intercurrent Illness • No data to support discontinuation of GH replacement treatment during illness • Risk of hypoglycemia should be considered in children with GH deficiency who discontinue GH treatment Safety - GH Therapy in Children Issues related to GH treatment in patients with non-GH deficient disorders • Monitoring glucose homeostasis in Turner syndrome and glucose homeostasis and lipid profiles in chronic renal failure should be undertaken at intervals determined by standard clinical practice • In patients with chronic renal failure treated with GH who receive renal transplant, assessment of graft function and surveillance for development of malignancy should be carried out according to routine nephrology guidelines Safety - GH Replacement in Adults Glucose Metabolism • Prevalence of diabetes mellitus (DM) increased in hypopituitary adults • Metabolic actions of GH include insulin antagonism • THUS, recommend that glucose metabolism be assessed in all patients before and during GH replacement • DM (or impaired glucose tolerance) not a contraindication to GH replacement; care of diabetes in GH-replaced adults should follow standard guidelines, but intensified monitoring of metabolic control is advocated in early phase of GH replacement of such patients Safety - GH Replacement in Adults Glucose Metabolism • Eye examination is indicated in case of overt diabetes and should be conducted in accordance with standard guidelines • Stable background retinopathy should not lead to discontinuation of GH replacement • Development of pre-proliferative changes and presence of proliferative retinopathy are contraindications to GH replacement Safety - GH Replacement in Adults Fluid Retention • Symptoms related to fluid retention may be encountered especially in early phase of GH replacement • This partly reflects a GH-induced, dose-dependent normalization of tissue hydration • Monitoring of hydration during GH replacement should include body weight measurement, patient interview and clinical examination Safety - GH Replacement in Adults Fluid Retention • In the case of persistent symptoms attributable to fluid retention, reduction of GH dose should be considered • Increased awareness of such symptoms and signs are recommended in patients with congestive heart failure Safety - GH Replacement in Adults Interaction with Other Hormones • Growth hormone increases extrathyroidal conversion of T4 to T3 - thyroid function should be monitored in all patients • GH may decrease serum total cortisol concentrations by decreasing circulating cortisol binding globulin Safety - GH Replacement in Adults Interaction with Other Hormones • Even though clinical implications for these observations are uncertain, increased awareness of glucocorticoid status is recommended in all patients • Possibility that overt ACTH insufficiency may be unmasked during GH replacement (as a result of inhibition of 11bHSD1) should be considered Safety - GH Replacement in Adults Heart Function and Lipoproteins • Increased prevalence of cardiovascular disease in active acromegaly cannot be extrapolated to GH-replaced hypopituitary adult • Monitoring of cardiovascular function should follow standard of care for normal population Safety - GH Replacement in Adults Heart Function and Lipoproteins GH replacement in adults is known to increase serum levels of lipoprotein(a). • Clinical implications - if any - are uncertain and should be weighed against beneficial effects of GH replacement on other cardiovascular risk factors • Measurement of lipoprotein(a) not recommended as standard procedure in hypopituitary patients Safety - GH Replacement in Adults Cancer risk and Tumor Recurrence • Increased incidence of certain malignancies has been reported in hypopituitary adults, but no evidence that it is associated with GH replacement • Current recommendations for cancer prevention and early detection in general population should be implemented in GHtreated hypopituitary adult Safety - GH Replacement in Adults Cancer Risk and Tumor Recurrence • To date no evidence to suspect that GH replacement influences recurrence rate or regrowth of pituitary/peripituitary neoplasms • Standard clinical practice requires regular pituitary imaging in patients with history of pituitary pathology • Baseline imaging study recommended in all patients before instituting GH replacement therapy Safety - Pharmacological GH Treatment in Adults ICU Trials • Power of placebo-controlled trials has been demonstrated with intensive care unit (ICU) studies, which showed that mortality was doubled in severely ill patients treated with high doses of GH • These studies have refuted clinical practice beliefs that high-dose GH is beneficial in this situation Safety - Pharmacological GH Treatment in Adults ICU Trials • Two placebo-controlled clinical trials (522 ICU patients) demonstrated that mortality increased from 19% (placebo-treated) to 42% (GH-treated) • Prolonged stay ICU patients following complications from open heart or abdominal surgery, multiple accidental trauma or those with acute respiratory failure were included Safety - Pharmacological GH Treatment in Adults ICU Trials • Supraphysiological doses of GH (5.3-8 mg or 0.07-0.13mg/kg per day) were administered • Most common causes of death were multi-organ failure, septic shock and uncontrolled infections • Baseline patient characteristics, severity of illness and diagnostic category did not explain increased mortality Safety - Pharmacological GH Treatment in Adults • Any GH treatment, other than replacement in those who have GH deficiency, should be considered as pharmacological • In specific conditions where pharmacological GH treatment is being considered, standard safety data should be collected and protocols for new drug development should be followed • Detrimental outcome of high dose GH treatment in ICU patients cannot be extrapolated to other conditions, which may potentially benefit from GH treatment Safety - Pharmacological GH Treatment in Adults • At present, not recommended that pharmacological GH treatment be initiated in adult ICU patients • In patients receiving pharmacological (in contrast to replacement) GH treatment, cessation of GH treatment should be considered when patient is critically ill • ICU trials should not discourage new studies of GH treatment in groups who may benefit from GH • Pharmacological doses used in such trials should be minimum effective dose for relevant endpoint Safety - Pharmacological GH Treatment in Adults GH levels and critical illness • GH-IGF system is dysregulated in critical illness • Not known whether this has effect on outcome in such patients, nor whether GH-deficient adults, including those receiving replacement therapy, are at higher risk for adverse outcomes when critically ill Safety - Pharmacological GH Treatment in Adults GH levels and critical illness • GH deficiency in adults and children, however, is frequently part of a more extensive pituitary deficiency including adrenocortical deficiency, which should be considered during critical illness in such patients • No data to support discontinuation of appropriate GH replacement in patients receiving intensive care treatment for critical illness, or during period of less severe illness or in relation to surgery Closing Remarks • Extensive data collected on large numbers of children and adults treated with GH indicate that, for current approved indications, GH is safe • Nevertheless, this workshop highlighted a number of areas where ongoing surveillance of long-term safety of GH replacement is important (cancer – glucose homeostasis – high dose pharmacological GH treatment) – Appropriately designed follow-up studies using adequate epidemiological tools and untreated controls are required