Hemolytic Anemias due to Other Intracorpuscular Defects
advertisement

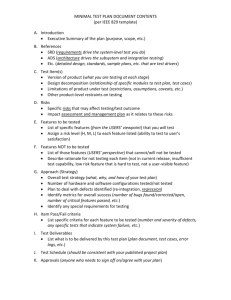
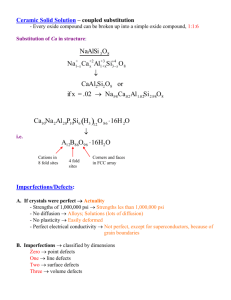
HEMOLYTIC ANEMIAS DUE TO OTHER INTRACORPUSCULAR DEFECTS What is intrinsically wrong with this RBC? OTHER INTRACORPUSCULAR DEFECTS Hereditary membrane defects – abnormalities in the constituent membrane proteins or lipids may alter the function and/or flexibility, shape, or stability of the membrane leading to hemolysis, most of which is extravascular via the spleen. INTRACORPUSCULAR DEFECTS Hereditary spherocytosis (HS) This is a group of heterogenous disorders which usually have an autosomal dominant inheritance (deletion in short arm of chromosome 8). The specific defect is a disorder of vertical protein interactions, most often characterized by a deficiency of spectrin. The deficiency may be a primary deficiency in spectrin or a secondary deficiency due to defective attachment of the cytoskeleton to the lipid bilayer. Deficiencies in band 3, ankyrin and protein 4.2 have also been found MEMBRANE DEFECT IN HS INTRACORPUSCULAR DEFECTS The net result of the skeletal defect is increased membrane instability and progressive membrane loss. This leads to a cell with a decreased surface to volume ratio and spherocytes with decreased flexibility and increased viscosity which all leads to extravascular hemolysis. The cells may also be more permeable to sodium and this eventually leads to decreased potassium and water and increased cell viscosity which also contributes to splenic culling. Clinical manifestations: Jaundice, mild to severe anemia, and an enlarged spleen. INTRACORPUSCULAR DEFECTS May have gallstones from the increased bilirubin. The MCHC is increased (greater than 36%). The peripheral smear shows spherocytes and polychromasia There is increased osmotic fragility The autohemolysis test is positive. In this test RBCs are incubated in their own plasma for 48 hours at 370 C and the amount of hemolysis is determined. Normal is .2-2%. With hereditary spherocytosis, the hemolysis is 5-25% at 24 hours, and 75% at 48 hours. The hemolysis will decrease when glucose is added for making ATP to pump out excess Na. OSMOTIC FRAGILITY TEST Fresh blood Incubated blood HEREDITARY SPHEROCYTOSIS INTRACORPUSCULAR DEFECTS Therapy = splenectomy Hereditary elliptocytosis (HE) This disease usually has an autosomal dominant inheritance Several subgroups which vary in the degree of hemolysis and clinical severity are found. There appears to be a spectrin dimer-dimer association problem. Decreased amounts of protein 4.1 have also been found The defect in the membrane cytoskeleton that results causes the abnormal shape (elliptocytes or ovalocytes). MEMBRANE DEFECT IN HE INTRACORPUSCULAR DEFECTS In the heterozygote form the weakened skeleton results in cells being permanently deformed when subjected to the sheer stress of the microcirculation (this is transient in normal RBCs). The cells have a nearly normal life span. In the homozygote state (and with some heterozygote variants) there is severe weakening of the cytoskeleton and membrane fragmentation occurs in addition to the formation of elliptocytes. This is called a hemolytic variant. Clinical manifestations: For the heterozygote it is usually a mild, compensated anemia with elliptocytes and polychromasia. The osmotic fragility and autohemolysis tests are normal. In the homozygous state (rare), there is marked poikilocytosis with elliptocytes and fragmented cells. There is increased osmotic fragility and autohemolysis. HEREDITARY ELLIPTOCYTOSIS HE – HEMOLYTIC VARIANT INTRACORPUSCULAR DEFECTS Therapy - splenectomy in hemolytic variants Hereditary pyropoikilocytosis (HPP) This is a rare autosomal recessive disorder with unstable spectrin leading to an unstable membrane cytoskeleton that undergoes sheer stress in the microvasculature described above for homozygous elliptocytosis. HPP cells actually have two spectrin defects, one from each parent. There is a deficiency of alpha spectrin from one parent. There is a mutant spectrin that prevents selfassociation of heterodimers from the other parent MEMBRANE DEFECT IN HPP INTRACORPUSCULAR DEFECTS This leads to a severe hemolytic anemia and marked poikilocytosis with budding cells, fragments, microspherocytes, and elliptocytes. The cells are thermally unstable and fragment at 45-460 C, whereas normal cells fragment at 490 C. There is increased osmotic fragility and autohemolysis. PYROPOIKILOCYTOSIS HPP AFTER HEATING INTRACORPUSCULAR DEFECTS Disorders of membrane cation permeability Hereditary stomatocytosis (stoma= mouth) In this disorder the RBC is abnormally permeable to sodium and potassium. The net gain of sodium is more than the net loss of potassium. Therefore water rushes in and the RBCs are swollen and less deformable and are culled in the spleen. The anemia may be mild to moderate with polychromasia. Stomatocytes (RBCS with slit-like or mouth-like areas of central pallor) are seen There is increased osmotic fragility and autohemolysis. HEREDITARY STOMATOCYTOSIS INTRACORPUSCULAR DEFECTS Hereditary xerocytosis In this disorder there is a net loss of potassium that exceeds the net gain of sodium resulting in a dehydrated cell as water rushes out. This leads to increased cytoplasmic viscosity, decreased deformability, and culling in the spleen. There is decreased osmotic fragility because of the net loss of water. Abnormal membrane lipid composition Spur cell anamia This is an acquired disorder associated with severe hepatocellular disease which causes an increases in serum lipoproteins, leading to an excess of RBC membrane cholesterol. This results in a moderate to severe hemolytic anemia with acanthocytes, leptocytes, echinocytes, and spherocytes. HEREDITARY XEROCYTOSIS SPUR CELL ANEMIA INTRACORPUSCULAR DEFECTS Abetalipoproteinemia (hereditary acanthocytosis) This is a rare autosomal recessive disorder characterized by an absence of serum lipoprotein, low serum cholesterol, low triglyceride, and low phospholipid with an increased cholesterol to phospholipid ratio. Acanthocytes may be seen, but there is usually no anemia associated with this disorder. Acquired membrane defects Paroxysmal nocturnal hemoglobinuria INTRACORPUSCULAR DEFECTS This disease is characterized by an RBC membrane that is abnormally sensitive to complement mediated lysis (WBCs and platlets are also affected). There is a classic pattern of irregular intravascular hemolysis and nocturnal hemoglobinuria. The condition is exacerbated during sleep when CO2 levels rise and the pH drops. It is believed to be caused by an abnormal clone of stem cells (idiopathic or due to marrow damage). All of the cell lines lack several anchored membrane proteins and this makes them abnormally sensitive to the complement mediated lysis (C3b can bind). Lack GPI (glycophosphatidylinositol) anchoring protein This can lead to peripheral pancytopenia PNH DEFECT INTRACORPUSCULAR DEFECTS Clinical findings: The classic presentation is of hemoglobinuria in the first morning urine specimen. The intravascular hemolysis that occurs during sleep may also be triggered by infection, surgery, or drugs. Most patients also have hemosiderinuria. Abdominal and back pain and headaches occur due to thrombosis of the abnormal platlets Lab findings: The peripheral smear shows pancytopenia with a normochromic, normocytic anemia and increased reticulocytes. The bone marrow is hyperplastic. The sucrose hemolysis and Ham's tests are positive and there is decreased leukocyte alkaline phosphatase in the granulocytes INTRACORPUSCULAR DEFECTS Treatment: Transfusions with washed cells Anticoagulants for venous thrombosis Hereditary enzyme deficiencies Glucose -6-phosphate dehydrogenase deficiency This is the most common red cell enzyme disorder. The enzyme is carried on the X chromosome. There are many different isoenzymes, and only a few of them have decreased enzyme activity. G6PD catalyzes the first step in the pentose phosphate pathway in a coupled reaction in which NADPH is made. NADPH is needed for glutathione reduction: G6PD ACTIVITY INTRACORPUSCULAR DEFECTS GSH protects the hemoglobin from oxidative denaturation to Heinz bodies. Normally G6PD activity is highest in young cells and decreases as the cell ages. Therefore, there are no problems until the cell starts to age. When a cell with an enzyme with decreased activity ages, the net result is Heinz body formation. The Heinz bodies attach to the RBC membrane, and this leads to increased membrane permeability and rigidity and removal by the spleen. Under normal conditions the bone marrow can compensate for the decreased RBC survival. INTRACORPUSCULAR DEFECTS However, when the individual is under acute oxidative stress ( drugs, fava beans in some cases, infection and being a newborn) this can result in membrane damage and lead to acute intravascular hemolysis. There is a decreased RBC count and hemoglobin, increased reticulocytes, bite cells, hemoglobinuria, and jaundice. Heinz bodies may be visualized by supravital staining. Diagnosis is by demonstrating decreased enzyme activity. Therapy is to avoid exposure to oxidant drugs and to give transfusions during a hemolytic episode. G6PD DEFICIENCY (HEINZ BODY ANEMIA) HEINZ BODIES INTRACORPUSCULAR DEFECTS Pyruvate kinase deficiency There are many different mutants of this enzyme that is part of the Embden-Meyerhoff pathway: INTRACORPUSCULAR DEFECTS Cells with PK deficiency fail to make enough ATP to maintain normal RBC function and therefore, they have a decreased survival time. Heterozygous individuals are clinically normal and homozygous individuals have a hemolytic anemia. Diagnosis is by assay for enzyme function. On the peripheral smear, the cells are dehydrated due to potassium loss. PK DEFICIENCY