Chapter 27
The Reproductive
System
G.R. Pitts, J.R. Schiller, and
James F. Thompson, Ph.D.
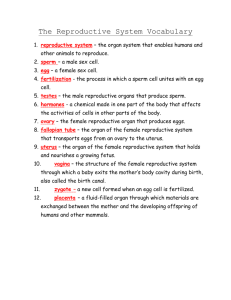
The Reproductive Systems
Reproductive
organs are grouped by function
Gonads - testes and ovaries
produce
gametes and secrete hormones
produce gametes and fluid; then discharge into
duct system indicates exocrine function
production of hormones indicates endocrine
function
Ducts
– receive, store, transport gametes
Accessory sex glands – support gametes
Supporting structures - various reproductive
functions
Males
Male Reproductive System
Testes, a system of ducts, accessory sex glands, and
several supporting structures (including the penis)
Male Reproductive System
Scrotum
2 fibrous sacs
which support and
protect the testes
Muscle
cremaster muscle
dartos muscle
Location and
temperature due to
muscle contraction
sperm production
requires temp 3 C
below body temp
involuntary muscle
contraction raises
the testes
Male Reproductive System
Testes - testicles
paired oval
glands 5 cm x
2.5 cm
development
influenced by Y
sex chromosome
and by maternal
hormonal levels
develop in
abdomen
begin descent
during the 7th
month of
development
Male Reproductive System
Surrounded by
dense connective
tissue
covered by tunica
vaginalis (serous
membrane) from
peritoneum
internal fibrous
capsule = tunica
albuginea
also forms septa
creating lobules
200-300
lobules/testicle
tunica albuginea
tunica vaginalis
Male Reproductive System
3 seminiferous tubules in each lobule (typical)
Each seminiferous tubule is lined with spermatogenic
cells in various developmental stages
Male Reproductive System
Blood-Testis Barrier prevents
immune system response to
sperm antigens
Sustentacular (Sertoli) cells
create blood-testis
barrier with tight
junctions
respond to FSH and
testosterone
phagocytize shed excess
spermatid cytoplasm
control sperm movement
and release into the
tubule lumen
secrete some nutrients
for sperm
secrete some fluid for
sperm transport
Male Reproductive System
Interstitial
endocrinocytes
(interstitial cells of
Leydig)
located between
tubules
secrete testosterone
in response to LH (=
ICTH)
Spermatogonia
undergo meiosis to
give rise to
spermatazoa
Male Reproductive System
Spermatogenesis
meiosis occurs in the
seminiferous tubules
produces haploid
spermatozoa
64-72 days in humans
Spermatogonia
Diploid stem cells
by mitosis, some remain
as viable stem cells
through out life
others undergo
developmental changes
to become primary
spermatocytes and
undergo meiosis
Male Reproductive System
Reduction division
primary spermatocytes
undergo meiosis I to
become secondary
spermatocytes (haploid)
secondary spermatocytes
undergo meiosis II to
become immature
spermatids (haploid)
Spermatids mature
morphologically into
spermatozoa = sperm cells
spermatid do not separate
their cytoplasm completely
they maintain cytoplasmic
bridges until released into
the tubule lumen
Male Reproductive System
Spermatogenesis
spermatids mature
physiologically into
spermatozoa
Requires 10-14 days for
migration to and 3-4
days for maturation in
the ductus epididymus
Older sperms are
removed gradually by
phagocytes within the
epididymus
Many sperms are
abnormal, either
morpholically,
physiologically, or
genetically
30% abnormal is
considered “normal”
Male Reproductive System
Spermatozoa
300 million/day mature
survive about 48 hrs
following ejaculation in the
female reproductive tract
structure
head
• nuclear material
• acrosome - enzymes for
penetration into egg
midpiece - site of ATP
production to power tail
tail - flagellum
Male Reproductive
System
Hormones of braintesticular axis
anterior pituitary drives
changes during puberty
controlled by GnRH from
hypothalamus
begins to secrete FSH, LH
LH – targets Interstitial
endocrinocytes
testosterone
dihydrotestosterone (DHT)
FSH - Sustentacular cells
Androgen-Binding Protein
(ABP) concentrates
androgens for spermatids
Inhibin – negative feedback
to the pituitary and
hypothalamus
Male Reproductive
System
Development
testosterone stimulates
pattern development before
birth (internal ducts)
DHT external genitals
estrogens from testes
brain development
Puberty – testosterone &
DHT stimulate enlargement
of male sex organs and
secondary sexual
characteristics
Male Reproductive System
Testosterone
secondary
-
sex characteristics:
muscular, skeletal growth
• heavier, thicker muscles and bones in men than in women
• also triggers epiphyseal closure
pubic, axillary, facial and chest hair
oil gland secretion
larynx enlargement deepening the voice
sexual
functions
male sexual behavior and aggressive behaviors
spermatogenesis
sex drive in both male and female
metabolism
- stimulates protein synthesis
“anabolic steroids” are often misused and abused
Male Reproductive System
Ducts
sperm move slowly
from the lumen of
seminiferous tubules
straight tubules
rete testis
epididymis
continuous sperm
and testicular fluid
production move
sperms along
fluid contains: H2O,
androgens,
estrogens, K+,
glutamic acid,
aspartic acid
Male Reproductive System
Epididymis
posterior border of testes
tightly coiled tube - head,
body, tail
6 m long if uncoiled
pseudostratified
columnar epithelium
microvilli provide nutrients
reabsorb testicular fluid
phagocytize degenerating
older sperm
ductus epididymis
site of sperm maturation
(10-14 days) - motility
may remain in storage for
a month, then reabsorbed
Male Reproductive System
Ductus (vas) deferens
less convoluted with a larger diameter
ascends, enters pelvic cavity through inguinal canal
loops up, over urinary bladder to end in the ampulla
Male Reproductive System
Ductus (vas)
deferens
pseudostratified
columnar
epithelium with
thick muscularis
transports sperm
from epididymis
to urethra by
peristalsis during
ejaculation
Male Reproductive System
Posterior View
Male Reproductive System
Spermatic cord:
testicular artery,
veins, lymphatic
vessels, autonomic
nerves, vas deferens,
cremaster muscle
descend with the
testes
Exit the abdominal
cavity through the
inguinal canal
Vasectomy – a
portion of each duct
is removed
Male Reproductive System
Ejaculatory Ducts
formed by ducts from seminal vesicle and ductus deferens
move sperm into prostatic urethra before ejaculation
Male Reproductive System
Urethra
terminal tract for
urinary and
reproductive
systems
3 regions:
prostatic urethra
membranous
urethra
spongy
(cavernous)
urethra
Ends at external
urethral orifice at
the bulb/glans of
the penis
Male Reproductive System
Accessory sex glands: seminal vesicles,
prostate, and bulbourethral glands
Male Reproductive System
1)
Accessory sex glands
secrete the fluid
portion of the semen
Seminal vesicles
base of urinary bladder
60% of semen
volume
secrete alkaline viscous
fluid containing:
fructose, ascorbic acid
prostaglandins
vesiculase
(coagulating enzyme)
keeps semen near
cervix while sperm
swim into cervix via
flagellar movements
Male Reproductive System
2)
Prostate
below bladder, around
urethra
secretes milky, slightly acidic
fluid with:
citrate
enzymes
• phosphatase
• fibrinolysin
prostate specific antigen
(PSA)
3)
Bulbourethral (Cowper's)
glands
beneath prostate gland at
membranous urethra
secrete:
•
•
alkaline fluid
mucus
neutralize acidic urine
Male Reproductive System
Semen - mixture of sperms and secretions
Average volume = 2.5 – 5.0 mL
50-150 million sperm/mL
below 20 million/mL infertility
Large numbers needed for successful fertilization
Slightly alkaline (pH 7.2-7.6), milky and mucoid
decreases acidity of vagina
fructose is the nutrient for sperm metabolism
prostaglandins decrease mucous viscosity and stimulate reverse
peristalsis
Contains natural antibiotic = seminalplasmin
Coagulates after ejaculation into vagina
somewhat different mechanism than blood clotting
breaks down in 5-20 minutes
Male Reproductive System
Penis
root (attachment)
body (shaft)
glans penis (head)
Male Reproductive System
Root of penis - bulb
(base of corpus
spongiosum)
Glans penis with
outer corona
Terminal slitlike
opening (external
urethral orifice)
Covering is prepuce
(foreskin)
circumcised in a
variety of societies
globally
Male Reproductive System
Body
3 cylindrical tissue masses surrounded by tunica albuginea
Dorsolateral pair, the corpora cavernosa penis
midventral corpus spongiosum penis with spongy urethra
All surrounded by fascia and skin
Each section has blood sinuses = erectile tissue
Male Reproductive System
Erection
Arteries dilate with
sexual stimulation, a
parasympathetic reflex
Large quantities of
blood enter the
sinuses
compress superficial
veins from sinuses
trapped blood
erection
Close bladder
sphincter
prevent urine flow
prevent semen
backflow
Ejaculation
Sympathetic reflex
Peristalsis
Arteries constrict, capillary
sinuses empty
Females
Female Reproductive System
Ovaries, uterine (Fallopian) tubes, uterus, vagina,
vulva, mammary glands
Female Reproductive System
Ovaries
Paired, small (pecan-sized) oval organs in the
pelvic cavity
Supported by several complex fibrous ligaments
Homologous in embryological development to the
testes
Female Reproductive System
Ovary Histology
Germinal epithelium
Tunica albuginea connective tissue
Ovarian follicles
Stroma – fibrous
connective tissue
cortex - outer dense
layer with ovarian
follicles containing
eggs = oocytes
medulla - inner
loose fibrous
connective tissue
layer containing
blood vessels
Female Reproductive System
Ovary Histology
Germinal epithelium
Primordial follicles
Ovarian follicles
Primary follicles
Secondary follicles
with antrum
formation
Vesicular (Graafian)
follicles with large
antrums
After Ovulation:
Corpus luteum
(“yellow body”)
Corpus albicans
(“white body”)
Female Reproductive System
Oogenesis
Formation of haploid
ova in the ovary
Steps
Reduction division meiosis I (haploid)
Equatorial division meiosis II
Maturation –
potential for
fertilization
Female Reproductive System
Uterine (Fallopian) tubes = oviducts
Extend laterally from uterus to transport ova by peristalsis
and cilia-generated current from the ovaries to the uterus
Structure
(1) infundibulum with fimbriae
(2) ampulla
(3) isthmus
2
1
3
Female Reproductive System
Once a month an ovarian follicle ruptures releasing
a secondary oocyte (ovulation)
Oocyte drawn into the oviduct by cilia-generated current
on the fimbriae and within the tube by cilia and peristalsis
Fertilization can occur at any time (ideally in 24 hours)
ideally in the ampulla – upper third of oviduct
becomes a zygote and then begins mitotic divisions
Unfertilized oocytes disintegrate and are swept out
Female Reproductive System
zygote
morula
blastocyst
with
trophoblast
membrane
implantation
more details
on the
stages of
embryonic
development
in the next
chapter
Female Reproductive System
Uterus
Site of menstruation, implantation, fetal development, labor
Between the urinary bladder and the rectum
Size and shape of an inverted pear
Female Reproductive System
3 parts of Uterus
1) Fundus 2) Body with 3) Isthmus
fundus
body
isthmus
Female Reproductive System
3 parts of Uterus
(cont.)
3)
Cervix
narrow portion that
opens into vagina
produces cervical
mucus; (20-60
mL/day)
•
•
more receptive to
spermatazoa at or
near ovulation
otherwise the
mucus plug keeps
microbes out
cervix, mucus
•
•
•
protect
spermatazoa
provide nutrients
role in capacitation
Cervical canal in cervix
internal os
external os
Female Reproductive System
Uterus bends between its
body and cervix
Uterus joins with the
vagina at a right angle
Female Reproductive System
Ligaments provide stability – important
especially during labor
broad ligaments
uterosacral ligaments
cardinal ligaments
round ligaments
Female Reproductive System
3 uterine layers
1)
Perimetrium
= visceral peritoneum
2)
Myometrium
3 layers of smooth muscle
•
•
thickest in fundus
thinnest in cervix
for expulsion at labor
Female Reproductive System
3 uterine layers
3)
Endometrium
highly vascular
surface layer
•
•
simple columnar
epithelium
ciliated, secretory cells
uterine (endometrial)
glands
Female Reproductive System
3 layers
3)
Endometrium
stroma (lamina
propria) of
glandular and
connective tissues
divided into 2
layers:
•
•
stratum
functionalis
(functional layer)
- shed during
menstruation
stratum
basalis (basal
layer) - gives rise
to stratum
functionalis
Female Reproductive System
Blood supply from
uterine arteries
arcuate arteries - circular
around the myometrium
radial arteries penetrate
into the myometrium with
smaller branches:
spiral
straight arterioles
• terminate in basilis
• supply materials to
regenerate functionalis
straight
spiral arterioles
• penetrate functionalis
• change during menstruation
drained by uterine veins
Female Reproductive System
Fetal expulsion =
labor and delivery
Oxytocin and
prostaglandins
regulate labor
ANS controls
contractions
Female Reproductive System
Vagina
Tubular,
fibromuscular
organ with
mucous
membrane
Between
bladder,
rectum
fornix
superiorly
attached to
uterus
recess (fornix)
forms around
the attachment
to the cervix
Several functions
passage for menstrual flow,
childbirth
receives penis and semen
Female Reproductive System
Vagina
histology
Mucosa
continuous with the uterus
non-keratinized stratified squamous epithelium and
connective tissue in folds (rugae)
• mucosal cells have large stores of glycogen
• upon decomposition produce organic acids lowers pH
dendritic (APC) cells – (source for HIV attachment --
AIDS?)
Muscularis
smooth muscle - outer circular, inner longitudinal layers
stretches to receive penis and for accommodating
childbirth
Adventitia
Vaginal
- areolar connective tissue
orifice - hymen – thin membrane
Female Reproductive System
Vulva - pudendum
Female external genitalia
this is a test
Mons pubis - anterior, adipose tissue
Labia majora
lateral skin folds with sebaceous and sudoriferous glands
homologous to scrotum
Labia minora - medial folds with sebaceous glands
Female Reproductive System
Clitoris
Anterior junction of labia majora
Small cylindrical mass of erectile tissue and nerves
Plays a role in sexual excitement
Homologous to penis; has prepuce and glans
Female Reproductive System
Vestibule
Region between
labia minora
Mostly the
vaginal orifice
Bulb of vestibule
2 elongated masses of tissue
fill with blood during sexual arousal
• narrows vaginal orifice
• increases pressure on penis
homologous to corpora spongiosum and bulb of penis
Female Reproductive System
External urethral orifice
Anterior to vaginal orifice, posterior to clitoris
Exterior opening of the urinary tract
Proximity to vagina and anus increase risk of UTI
Female Reproductive System
Accessory
glands
Paraurethral
(Skene's) glands
On either side of external urethral orifice in the vulva
Secrete mucus
Homologous to prostate gland
Greater
vestibular (Bartholin's) glands
Open in the area between hymen and labia minora
Mucus secretion during sexual intercourse
Some lesser vestibular mucous glands also present
Homologous to bulbourethral (Cowper's) gland
General Reproductive System
Perineum
Diamond
shaped area
between
thighs,
buttocks
Contains
external
genitals,
anus
Urogenital triangle
Anal triangle
anterior -
pubic
symphysis
posterior coccyx
Anterior - urogenital triangle
Posterior - anal triangle
Episiotomy – to ease labor
Female Reproductive System
Mammary Glands
Modified sudoriferous
(sweat) glands that
produce milk
Anatomy
over pectoralis major
and serratus anterior
muscles
attached to the deep
fascia
surrounded by adipose
and fibrous tissue
suspensory ligament
of breast
• runs between skin
and deep fascia
• supports breast
Female Reproductive System
Mammary Glands
Nipple
exterior pigmented projection
many closely spaced openings -
lactiferous ducts
Areola
surrounding pigmented area
sebaceous (oil) glands
Female Reproductive System
Mammary Glands
15 - 20 lobes internally
separated by adipose
tissue (which determines
breast size and shape)
separated into lobules
with milk-secreting
glands = alveoli
milk (when being
produced) passes from
alveoli secondary
ducts mammary ducts
approaching the nipple,
the mammary ducts
expand to form lactiferous
sinuses (for storage)
sinuses continue to nipple
Female Reproductive System
Mammary
Develop
Gland Development
at puberty due to estrogen, progesterone
Ducts develop, fat deposition occurs
Areola and nipple enlarge; become pigmented
Further development occurs following ovulation and
corpus luteum formation in menstrual cycle or
pregnancy
Female Reproductive System
Mammary
Gland Physiology
Primary
function is milk synthesis
Secretion and ejection together = lactation
Primary stimulus for milk production is prolactin
from the anterior pituitary
Stimuli for milk release (letdown) in response to
suckling:
oxytocin from posterior pituitary
ANS reflexes
Female Reproductive System
Breast Cancer
12% of women will have breast cancer
3.5% will die of breast cancer
Early detection is the most important aspect
Each month after a menstrual period, the breasts should be
examined for lumps, puckering of skin or nipple retraction or
discharge
Genes BRCA1 and BRCA2 linked to the 10% of hereditary
breast cancers
BR-1 is a new marker (2003), esp. for black women
But >70% of breast cancers are not associated with known
risks
http://www.time.com/time/photoessays/breast_cancer/
Female Reproductive System
Breast
Risk
Cancer
factors
family history
early onset menses and late menopause
no child or first child after age 34
previous breast cancer
exposure to ionizing radiation (x-rays)
obesity, alcohol intake, cigarette smoking
Detection
- mammogram, flattening is the key to a
sharp image
Treatment
lumpectomy (removal of tumor and surrounding tissue)
radical mastectomy (breast, pectoral muscles, axillary
lymph nodes)
Female Reproductive Cycle
Two
parts in two different areas
Ovarian
cycle - events in ovary leading to
ovulation
Menstrual (uterine) cycle - endometrial changes
Controlled
by varying levels of several
hormones from several glands
Anterior
Pituitary
Ovarian follicles
Corpus luteum
Hormones
Ovaries
target several organs
– Uterus – Breasts – CNS
Female Reproductive Cycle - Hormones
Female Reproductive Cycle
Reproductive
cycle
Normally 2435 days in
length
Anterior
Pituitary
hormones
target ovary
Ovarian
hormones
target uterus
(and breasts)
Female Reproductive Cycle
3 Phases of
Reproductive
cycle
1. Day 1-4 -
menstrual
phase
2. Day 5-14 -
preovulatory
(proliferative)
phase
3. Day 15-28 postovulatory
(secretory)
phase
1.
2.
Proliferative
3.
Secretory
Female Reproductive Cycle
Menstrual Phase
50-150 ml of discharge: tissue fluid, mucus, epithelial cells
and a small quantity of blood from the endometrium
levels of estrogen/progesterone - negative feedback
uterine spiral arteries constrict creates ischemic tissue
entire stratum functionalis sloughs off
Ovaries
FSH levels rise (from day 25 of cycle) to stimulate a few primordial
follicles to develop into primary follicles
All follicles release low levels of estrogen
By day four, ~20 develop into primary and then secondary (growing)
follicles
• granulosa cells surround oocyte
• zona pellucida forms between oocyte and the granulosa (follicular cells)
– cells secretes watery follicular fluid into antrum
– fluid forces oocyte to the follicle’s edge and fills follicular cavity
Female Reproductive Cycle
Preovulatory
Phase - lasts 6-13 days
Menstrual
and Preovulatory phase together are
known as the Follicular phase
By day 6 of the cycle, one follicle outgrows others
dominant follicle secretes & inhibin
estrogen & inhibin reduce FSH secretion • all other follicles stop growing and degenerate = atresia
estrogen levels increase due to this single follicle
Dominant
follicle matures
vesicular ovarian (Graafian) follicle (mature follicle)
forms a blister-like bulge on the surface of the ovary
Female Reproductive Cycle
Preovulatory Phase
Follicle continues to
secrete estrogen
FSH is dominant early
Close to ovulation, LH
becomes important
Estrogen stimulates
endometrial
regrowth
stratum basalis
• mitosis creates a
new stratum
functionalis
endometrial glands
redevelop
arterioles coil and
lengthen
Female Reproductive Cycle
Ovulation
LH
pulse causes rupture of vesicular = Graafian
follicle and release of oocyte into the pelvic
cavity; occurs approximately day 14
Secondary oocyte
surrounded by follicular cells, corona radiata
secondary oocyte in metaphase II
Fimbriae
become more active; cilia create
currents in peritoneal fluid to carry oocyte into
uterine tube
Estrogen causes changes in body temperature
and cervical mucus becomes less gelatinous
Female Reproductive Cycle
Ovulation
Prior to ovulation
high estrogen exerts
positive feedback on FSH,
LH
sudden surge of LH causes
release of oocyte
LH surge is measurable
Following ovulation
follicle collapses becoming
corpus hemorrhagicum
follicular cells then
enlarge, change character,
form the corpus luteum
follicular cells respond to
LH by secreting estrogen
and now progesterone
Female Reproductive Cycle
Postovulatory
Phase
Most
constant in duration, lasts for 14 days, from
ovulation to the next menses
LH stimulates corpus luteum development (luteal
phase); corpus luteum secretes increased levels
of estrogen and progesterone
Progesterone prepares endometrium to receive an
embryo (if it has developed sufficiently)
growth and coiling of endometrial glands
vascularization of surface endometrium
endometrial thickening
increased tissue fluid
secretory phase for the endometrial glands
Female Reproductive Cycle
Postovulatory
If
Phase
no fertilization
estrogen and progesterone inhibit GnRH and LH
corpus luteum degenerates (no LH) corpus albicans
levels of estrogen and progesterone
• stop endometrial development
• stimulate next menstruation
• stimulate anterior pituitary hormones to begin next cycle
If
fertilization occurs
corpus luteum maintained until the placenta takes over
maintained by hCG (human chorionic gonadotropin)
• produced by chorion (outer embryonic membrane which
becomes the bulk of the placenta)
• home pregnancy test detects hCG
placenta produces estrogen, progesterone
Female Reproductive Cycle -- Review
Female Reproductive Cycle -- Review
Physiology of Sexual Intercourse
Male Reproductive Act
Erection
may be initiated by anticipation, memory, visual
stimulation or as a reflex from physical stimulation
Parasympathetic stimulation causes vasodilation of
capillary sinuses, compression of veins erection
Lubrication
Parasympathetic impulses stimulate bulbourethral and
urethral glands
glands secrete mucus for lubrication
Physiology of Sexual Intercourse
Male Reproductive Act (cont.)
Orgasm
tactile stimulation causes ejaculation
• intense stimulation causes rhythmic sympathetic impulses
causing peristaltic contractions of ducts propelling
spermatazoa into ductus (vas) deferens urethra
• simultaneous stimulation of seminal vesicles, prostate and
bulbourethral glands add seminal fluid to the spermatazoa
• stimulation of skeletal muscle at the base of the penis triggers
rhythmic contractions to help expel semen ejaculation
sensory input including HR, BP, RR, pleasurable
sensations, along with ejaculation, define male orgasm
followed by a refractory period
Physiology of Sexual Intercourse
Female Reproductive Act
Arousal – mediated by Parasympathetic Division of ANS
stimulation of breasts, genitalia, especially the clitoris, generates
arousal
clitoris, vaginal mucosa and breasts engorge with blood
lubrication - secretion of mucus from epithelium of the cervical
mucosa
Orgasm (climax) - maximal tactile stimulation of genitalia
results in orgasm, mediated by Sympathetic Division
(ANS)
perineal muscles contract rhythmically; general increase in muscle
tension; rhythmic contractions of the uterus
engorgement of clitoris, breasts
HR, RR, BP
intense pleasurable sensations
Birth Control = Contraception
Sterilization
vasectomy
in males and tubal ligation in females
(tubes cut and sealed)
Hormonal
methods
Intrauterine devices
Barrier methods
Chemical methods
Physiological methods
Abortions
Birth Control = Contraception
Hormonal
Oral
methods
contraception – simulate “pregnant state”
generally higher in progesterone and lower in estrogen
• negative feedback inhibition of FSH, LH and GnRH
• prevents follicular development and ovulation
• also alter cervical mucous and make endometrium less
receptive to implantation
allows for regulation of length of menstrual cycles,
menstrual flow, and prevention of ovarian cysts
not good for women with clotting problems, cerebral
blood vessel damage, hypertension, liver malfunction
or heart disease
an increased risk for heart attack and stroke in women
who smoke and drink
Birth Control = Contraception
Hormonal
methods
Norplant
surgical implants under skin of progestin
prevents ovulation and thickens cervical mucus
No
male oral contraceptive currently available –
research underway
Intrauterine
Small
devices
plastic, copper or stainless steel device
inserted into uterine cavity to prevent
implantation
Danger of pelvic inflammatory disease, infertility,
and excessive menstrual bleeding and pain
Birth Control = Contraception
Barrier
methods
Condom
nonporous materials (e.g., latex) provide mechanical
barrier to sperm deposition
reliable when used correctly
both male and female versions
The only method likely to prevent STD's and reliable
when used correctly
Diaphragm
rubber dome-shaped device is placed over cervix to
stop sperm passage; often used with spermicide
toxic shock syndrome and frequent urinary tract
infections are possible with incorrect use
Birth Control = Contraception
Chemical
methods - spermicidal agents, make
vagina more inhospitable to sperm and may
prevent sperm flagellar motility
Physiological
Coitus
methods – not too reliable
interruptus (withdrawal)
Rhythm method - abstention for 3 days before
and after ovulation (estimated)
Sympto-thermal method - abstention when signs
of ovulation are present
Birth Control = Contraception
Induced
RU486
abortion
(mifepristone) – drug blocks progesterone
preventing proper endometrial development
menstruation occurs
Various surgical procedures
End Chapter 27