Chronic and invasive aspergillosis
advertisement

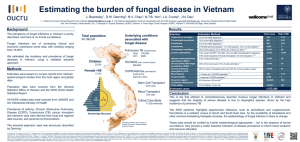
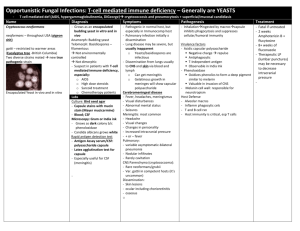
Interaction of Aspergillus with the host Acute IA Subacute IA ABPA Severe asthma with fungal sensitisation Allergic sinusitis Aspergilloma Chronic pulmonary Immune dysfunction Frequency of aspergillosis Frequency of aspergillosis A unique microbial-host interaction Immune hyperactivity . After Casadevall & Pirofski, Infect Immun 1999;67:3703 Size of fungal disease problem globally 1. Invasive aspergillosis - ? 70,000 cases/year in EU, >5M at risk; new problems COPD, ICU etc - ~50% mortality 2. Candidaemia in UK – 2,000 cases, rising, many more at risk, ~40% mortality 3. Cryptococcal meningitis - ~1M worldwide annually 4. Chronic pulmonary aspergillosis after TB – 1.1M cases prevalence 5. Chronic pulmonary aspergillosis total - ~3M 6. Asthma 197M in adults, of which ~10-20% severe, UK and USA have very high prevalence rates 7. Allergic bronchopulmonary aspergillosis in asthma - ~3M worldwide (2.1% of adults with asthma) 8. Severe asthma with fungal sensitisation - ~13M worldwide (33% of 20% (severe only)) CLASSIFICATION OF ASPERGILLOSIS Airways/nasal exposure to airborne Aspergillus Persistence without disease - colonisation of the airways or nose/sinuses Invasive aspergillosis • Acute (<1 month course) • Subacute/chronic necrotising (1-3 months) Chronic aspergillosis (>3 months) • Chronic cavitary pulmonary • Aspergilloma of lung • Chronic fibrosing pulmonary • Chronic invasive sinusitis • Maxillary (sinus) aspergilloma Allergic • Allergic bronchopulmonary (ABPA) • Extrinsic allergic (broncho)alveolitis (EAA) • Asthma with fungal sensitisation • Allergic Aspergillus sinusitis (eosinophilic fungal rhinosinusitis) Risk factors for invasive aspergillosis Major • Neutropenia (+ monocytopenia) • Corticosteroid treatment Minor • CD4penia • Inherited immunodeficiency (ie CGD) • Lung or sinus damage/disease • Severe liver disease • Exposure to high inocula Risk of acquisition (and pace of progression) Examples of at-risk patients and pace of progression 25% 20% 15% 10% 5% Degree of immunocompromise Where in the hospital does invasive aspergillosis occur? Cornillet et al, Clin Infect Dis 2006;43:577 Risk factors for invasive aspergillosis in AIDS Stage of AIDS CDC Group II CDC Group IV Neutropenia <1000 x 106/L Corticosteroid therapy Prior pulmonary infection 4 (1%) 289 (72%) 92/202 (46%) 79/202 (39%) 124/169 (73%) Khoo & Denning, Clin Infect Dis 1994; 19 (S1) 541 Lymphoma and corticosteroids 4 days later www.aspergillus.org.uk CT scan showing nodules with halo – lung cancer and neutropenia Aspergillus, IPA and COPD ~ 22% of Aspergillus in COPD = invasive aspergillosis Guinea et al, Clin Microbiol Infect 2010;16:870 Aspergillus, IPA and COPD Guinea et al, Clin Microbiol Infect 2010;16:870 Aspergillus, IPA and COPD Clues to the diagnosis of IA • GOLD stage 3 or 4. • Excess wheezing (consider tracheobronchitis) • Worsening infiltrates in an ‘exacerbation’ (66%) • Bilateral infiltrates (55%) • Culture of Aspergillus • High corticosteroid exposure recently • Do NOT expect fever (38%), chest pain or haemoptysis Guinea et al, Clin Microbiol Infect 2010;16:870 Invasive aspergillosis in COPD Bulpa, Clin Infect Dis 2007;30:782 Invasive aspergillosis in ICU 127 of 1850 (6.9%) consecutive medical ICU admissions with IA or colonisation (micro/histol). 89/127 (70%) did not have haematological malignancy 67/89 proven/probable IA, 33 of 67 (50%) COPD Meersemann et al, Am J Resp Med Crit Care 2004;170:621. Radiology completely unhelpful in suspecting the diagnosis Meersseman, Clin Infect Dis 2007;45:205 Risk factors for invasive aspergillosis in ICU Meersseman, Clin Infect Dis 2007;45:205 Invasive aspergillosis in ICU Aspergillus detected, no infection N = 89 Invasive aspergillosis + treatment N = 73 Invasive aspergillosis no treatment N = 12 Vandewoude et al, Critical Care 2006;10:R31. Invasive Aspergillosis in Children in the USA in 2000 Incidence of 437 cases per 100,000 immunocompromised children MORTALITY RATES Disease Acute Leukemia (ALL) Patients with Patients without Invasive Aspergillosis Invasive Aspergillosis Relative Risk (151,537 children) (666 children) of Death 1% 21% 14.9 Acute Leukemia (AML) 3% 20% 5.0 Brain Tumor 2% 69% 21.6 Bone Marrow Transplant 8% 44% 3.8 Zaoutis TE, et al. Pediatrics 2006;117:e711 Pseudomembranous Aspergillus tracheobronchitis Wheezing 4 days before death, immunocompromised Tait, Thorax 1993;48: 1285 Pseudomembranous Aspergillus tracheobronchitis Pseudomembranous Aspergillus tracheobronchitis with IPA in COPD Bulpa Eur Resp J 2007;30:782 Myelodysplasia with clinical evidence of acute invasive fungal rhinosinusitis after chemotherapy – biopsy showed hyphal invasion of bone Pre-treatment 6 months later after initial caspofungin then voriconazole www.aspergillus.org.uk Cultures for Aspergillus from sputum and BAL Bacteriological media inferior to fungal media – 32% higher yield on fungal media Yield in IA from BAL and sputum ~30% Cultures take 1-10 days to grow + time to identification Horvath & Dummer, Am J Med 1996;100:171 Modalities for early diagnosis of invasive aspergillosis • • • • CT scanning Microscopy Antigen (blood or respiratory fluid) [PCR (blood or respiratory fluid)] Pediatric Galactomannan • Prospective study from 1995-1998 • GM > 1.5 in at least two sequential samples Adult Pediatric – Sensitivity 88.6% 100% – Specificity 97.5% 89.9% – 450 adult allogeneic HSCT patients (3883 samples) – 347 children with hematologic malignancies (2376 samples) • False-positive antigenemia – Adult patients 2.5% (10/406) – Pediatric patients 10.1% (34/338) Sulahian Cancer 2001;91:311. Pediatric GM in Oncology Patients • St. Jude & NCI – 56 pediatric oncology patients – 39 pts without IA; 17 pts with proven/probable IA – Most done retrospectively (frozen samples) • At least one GM positive in 11/17 patients with IA (sensitivity 65.7%) • False-positive rate 1% (all ≤ 0.8) (per sample) • At least one false-positive in 12.8% patients • Piperacillin-tazobactam was not used in any patients in this study • No association with accuracy and patient age Hayden R Pediatr Infect Dis J 2008;27:815 Unequivocal ‘Halo sign’ surrounding a nodule Halo Small vessel angioinvasion Herbrecht, Denning et al, NEJM 2002;347:408-15. IPA www.aspergillus.org.uk Pulmonary nodules a useful feature if invasive pulmonary aspergillosis CT features in 48 CTs of which 17 IPA Halo Nodules Masses IPA 13/17 14/17 6/17 Other 0/31 11/31 2/31 Kami, Mycoses 2002;45:287-94. Microscopy Fluorescent brighteners such as Calcufluor white, Blankophor increase sensitivity and speed Ruchel R, www.aspergillus.org.uk/images Cultures for Aspergillus from sputum and BAL Yield in IA from BAL and sputum ~30% Bacteriological media inferior to fungal media – 32% higher yield on fungal media Horvath & Dummer, Am J Med 1996;100:171-8. Aspergillus Antigen in BAL • 13/17 (76%) in acute leukaemia with CT abnormality • 20/20 (100%) in haem-onc pts with IPA • 37/49 (76%) in HSCT & haem-onc with IPA • 6 of 11 (55%) immunocompromised (8 of 11 +ve by PCR) • 5/20 (25%) in suspected IFIs • 17/17 (100%) in neutropenic patients before antifungal Rx, 0% after 3d antifungal therapy Becker, Br J Haem 2003;121:448; Sanguinetti, JCM 2003;41:3922; Musher, JCM 2004;42:5517. Diagnosis of IPA in leukaemia using blood PCR 130 haematology patients Itraconazole prophylaxis for AML and HSCT Fluconazole prophylaxis for others (ALL, lymphoma etc) EORTC/MSG criteria applied 2x weekly sampling Barnes et al, J Clin Pathol 2009;62:64 Diagnosis of IPA in leukaemia using blood PCR and Aspergillus antigen (EIA) Barnes et al, J Clin Pathol 2009;62:64 Chronic pulmonary aspergillosis Infection of the lung by Aspergillus Single fungal ball or aspergilloma in a preexisting cavity Simple (single) aspergilloma Patient RK Haempotysis, nil else Positive Aspergillus antibodies in blood Lobectomy Wythenshawe Hospital Simple (single) aspergilloma Patient NM August 2006 May 2009 Community acquired pneumonia requiring ICU care New cough Positive Aspergillus antibodies in blood Lobectomy Wythenshawe Hospital Chronic pulmonary aspergillosis Infection of the lung by Aspergillus Single fungal ball or aspergilloma in a preexisting cavity Invasive aspergillosis /community acquired infection Chronic cavitary pulmonary aspergillosis +/- fungal ball Chronic fibrosing pulmonary aspergillosis +/- fungal ball ‘Multicavity’ disease is the hallmark of chronic cavitary pulmonary aspergillosis (CCPA) + Aspergillus IgG antibodies (precipitins) + symptoms Wythenshawe Hospital Chronic cavitary pulmonary aspergillosis (CCPA) – sputum production Aspergillus cultures positive in CCPA in 10-40% of cases only Wythenshawe Hospital Chronic cavitary pulmonary aspergillosis (CCPA) – coughing up blood (haemoptysis) Wythenshawe Hospital Underlying diseases in patients with CPA (%) Classical tuberculosis Atypical tuberculosis ABPA COPD/emphysema Pneumothorax Lung cancer survivor Pneumonia Sarcoidosis (stage II/III) Thoracic surgery Rheumatoid arthritis Asthma / SAFS Ankylosing spondylitis None Smith, Eur Resp J 2010 In press Frequency of chronic pulmonary aspergillosis after TB 25-33% of patients with TB are left with a cavity ~10% of all cases of pulmonary TB get CPA Anonymous. Tubercle 1970;51:227; Sonnenberg et al, Lancet 2001;358:1687 Global CPA cases per region related to TB 5 year prevalence estimates Denning, Pleuvry & Cole, Bull WHO 2011 in press Chronic pulmonary aspergillosis Chronic cavitary pulmonary aspergillosis complicating ABPA Chronic cavitary pulmonary aspergillosis with bilateral aspergillomas complicating sarcoidosis www.aspergillus.org.uk ABPA and development of CPA 1985 1981 2002 1995 1993 www.aspergillus.org.uk Bronchoscopy in an ABPA patient on no treatment UHSM, unpublished Bronchoscopy in an ABPA patient on no treatment BAL Abundant mixed inflammatory cells with ciliated columnar cells and a few fungal hyphae, in keeping with Aspergillus. A few Charcot leyden crystals. No maligant cells. UHSM, unpublished Routine versus high volume culture versus real time PCR for Aspergillus Aspergillus positive samples (%) Aspergillus culture MycAssay Aspergillus real time Routine High volume PCR Sample n Pre-bronch sputum 4 0 4 (100) 4 (100) Post-bronch sputum 4 0 1 (25) 4 (100) First trap aspiration 3 0 2 (67) 3 (100) First BAL (10-20mL) 5 0 0 4 (80) Second BAL (10-50mL 5 0 0 4 (80) Fraczek, ECCMID Abstract submitted Molecular detection of Aspergillus spp. in sputum Laboratory result Culture positive for A. fumigatus qPCR positive for Aspergillus spp ABPA CPA Normals 0/19 7/42 (16.7%) 0/11 15/19 (78.9%) 30/42 (71.4%) 4/11 (36.4%) Denning et al. Clin Infect Dis 2011; Colonisation in ‘normal’ lungs 22 of 30 (73%) grew a fungus in both lung samples taken 10/30 (33%) grew >1 species Lass-Florl et al, Br J Haematol 1999;104:745 Antifungal therapy IDSA guidelines. Walsh et al. Clin Infect Dis 2008;46:327 Time to initial response with posaconazole therapy 6 months 12 months Mean 95% confidence interval Felton et al. Clin Infect Dis 2010. In press. www.aspergillus.org.uk