Yeast - WordPress.com
advertisement

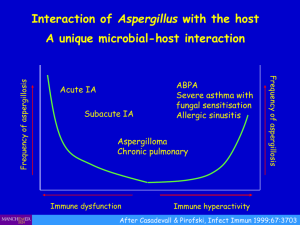
Clinical Spectrum of some Mycotic Agents. MOLDS YEAST -Candida -Cryptococcus -Malassezia furfur -Aspergillus -Mucorales -Dermotophytes DIMORPHIC FUNGI -Sporothrix shenckii (Sporotrichosis) -Histoplasma capsulatum (histoplasmosis) -Coccidioides immitis (coccidioidomycosis ) Candida Gram positive, oval, budding yeast. Opportunistic pathogen Types: C. tropicalis C. parapsilosis C. glabata Principal pathogen: Candida albicans Predisposing factor: 1. At extreme of age 2. During pregnancy 3. Debilitated/immunosuppressed patients 4. Diabetes Mellitus 5. Use of broad spectrum antibiotics 6. Treatment with steroids (include inhale steroids) Infections: Superficial infections Deep infections Lab Diagnosis: Specimens: According to the site of infections M.V: Yeast cells appear as oval gram positive budding yeast with pseudohyphae Culture: SDA (Sabouraud Dextrose Agar) inhibit bacterial growth Some specialized (chromogenic) agars: for easy differentiation. Biochemical Reaction: Germ tube formation: Most true C. albicans produce true hyphae when incubated for 2-3h in human serum. Chlamydospores formation on cornmeal agar Sugar fermentation & assimilation Treatment: Topical antifungal (superficial infections) Oral/Parentral= immunosuppressed patients Cryptococcus neoformans From: Cryptococcus Opportunistic pathogens Most infections occur @ IMMUNOCOMPRIMISED patients <HIV patients mostly> Encapsulated yeast Widely in nature: Dried pigeon droppings Soil contaminated with bird droppings Pathogenesis: Fungus was inhaled & the lungs are principal portal of entry Meningitis (acute/chronic): Clinical manifestation Lab Diagnosis: Specimens: CSF, blood, sputum M.V: CSF: Mounted in India Ink encapsulated budding yeasts appear surrounded by large gelatinous capsule Culture: SDA: gives mucoid colonies of typical capsulated yeast. Also give diagnostic brown pigments on bird seed (Niger seed) media Biochemical Reaction: Urease: Positve Serological reaction: Detection of cryptococcal capsular antigen in CSF/serum using anticapsular antibodies <latex agglutination> Treatment: 𝐴𝑚𝑝ℎ𝑜𝑡𝑒𝑟𝑖𝑐𝑖𝑛 𝐵 𝑜𝑟 𝑓𝑙𝑢𝑛𝑎𝑧𝑜𝑙𝑒 + 𝐹𝑙𝑢𝑐𝑦𝑡𝑜𝑠𝑖𝑛𝑒 -antifungal *can pass BBB* Malassezia furfur Lipophillic yeast (part of normal flora) Cause common, mild superficial infections: Pityriasis versicolor Potentially disfiguring skin condition Development of numerous brown scaly patches, hypopigmentation of skin Treatment: (sorry…tak sempat salin from lecturer) Aspergillus Species: A. fumigatus A. niger A. flavus Pathogenesis: Opportunistic organism Risk factors: (…sorry tak sempat salin…) Allergic aspergillosis Hypersensitivity reaction to the inhalation of Aspergillus spores Asthma-like symptoms Formation of mucus plug which may contain Aspergillus mycelium Aspergilloma Fungus ball that usually occurs in patients with pre-existing lung cavities Invasive pulmonary aspergillosis Rapidly & progressive & life threatening infection Lab diagnosis: a. Specimen: Sputum b. M.V: Long branching hyphal strands dichotomously branch) may be seen in sputum (direct examination) After digestion with 10% KOH Allergic aspergillosis Invasive aspergillosis: result is negative *need lung biopsy and it’s important* c. Culture: Grows steadily on routine culture media <SDA without cycloheximide…why did they use that? Because the cycloheximide will inhibit the aspergillus> d. Serological reaction: Detection of high level of Asperfillosis Antibodies in serum *it will increase with aspergillomas* e. Radiological: invasive aspergillus f. Histologically: made by deep tissue biopsies/sterile body Treatment: Pulmonary aspergillosis: Steroids Aspergillomas: surgical excision (manage hemoptysis) Invasive: high-dose systemic antifungal therapy Dermotophytes Filamentous fungi that cause superficial infection of keratinized structures 3 types: a) Trichophyton b) Epidermophyton c) Microsporum Natural reservoir: Humans: anthropophilic Animals: zoophilic Soil: geophilic Human infections: E. floccosum T. rubrum T. mentagrophytes T. tonsurans (anthropophilic) M. canis (zoophilic) Pathogenesis: Clinical picture: ring worm/tinea According (anatomically) to site Lab diagnosis a. Specimen: skin scales, nail/hair covered with 10% KOH b. MV: branching hypha & spores c. Culture: Dermatophytes grow readily on routine media *SDA + Cycloheximide & Chloraphenicole Treatment: Difficult & long courses Antifungal drugs (orally) I. Griseofulvin II. Itraconazole Sporotricosis Infection on subcutaneous tissue Occurs within 3 months of a contaminated inoculation injury (arms/hands) Painless nodules develops at site injury Further lesions develop along lymphatic channels Treatment: Oral itraconazole Saturated potassium iodide solution Histoplasmosis Species: Histoplasma capsulatum: Dimorphic fungus Causes: Asymptomatic infection/only mild self-limiting chest infection More pulmonary infection occurs <resembles TB> Treatment: Amphotericin B/Itraconazole Coccidioidomycosis Species: Coccidioides immitis Found: soil in SW of USA & some parts of Central & SA Infection occur: Inhalation of airborn spores (anthroconidia) from environment Endospores: Patient sputum (highly infectious) Similar to Histoplasmosis *no yeast form *it is highly infectious