Gardening can affect your lungs- Aspergillus
advertisement

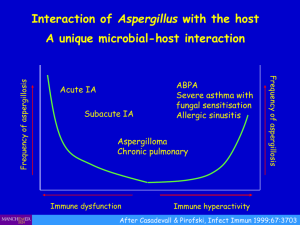
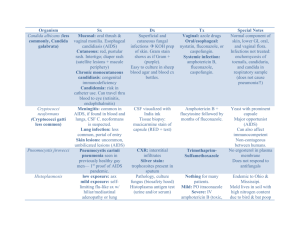
Gardening can affect your lungs - Aspergillus ARDS in an immunocompetent patient N. Jung1§, S. Mronga1, S. Schroth1, T. Vassiliou2, F. Sommer3, E. Walthers4, C. Aepinus5, A. Jerrentrup1, C. Vogelmeier1, A. Holland1*, AR Koczulla1* 1 Department of Medicine, Pulmonary and Critical Care Medicine, University Medical Center Giessen and Marburg, Philipps-University Marburg, Member of the German Center for Lung Research (DZL), Marburg, Germany 2 Department of Anesthesiology and Critical Care Medicine, Marburg, Germany 3 Department Institute for Medical Microbiology and Hygiene, Marburg, Germany 4 Department of Diagnostic and Interventional Radiology, Marburg, Germany 5 Department Institute for Virology, Marburg, Germany * Both authors contributed equally to this work § Corresponding author Email addresses: NJ: jungnin@med.uni-marburg.de SM: mronga@med.uni-marburg.de SS: schroth@med.uni-marburg.de TV: Timon.Vassiliou@med.uni-marburg.de FS: sommerf@med.uni-marburg.de EW: walthers@med.uni-marburg.de CA: aepinus@staff.uni-marburg.de AJ: jerrentr@med.uni-marburg.de CV: vogelmei@med.uni-marburg.de AH: holland@med.uni-marburg.de ARK: koczulla@med.uni-marburg.de Abstract Background Acute aspergillosis infection in immuncompetent patients is rare. This is the first published case of a survived aspergillus sepsis enlisting early veno-venous bypassing and early antifungal treatment. Case Presentation We describe the course of a severe aspergillosis sepsis of an immunocompetent 54-year-old woman after plant mulch dispersion leading to pulmonary failure and subsequently to sepsis with multiorganic failure. In light of the severe course of the disease, with necessity to treat the ARDS with a veno-venous extracorporal support (ECMO), the typical history and one published case report dealing with aspergillosis after plant mulch dispersion, antimycotic systemic treatment was given with voriconazole, although no final microbiological proof was available. The patient recovered and ECMO was discontinued after 1 week. After 7 days of antifungal treatment, aspergillus was no longer detectable. Conclusions Doctors should be aware that signs of sepsis after gardening may be caused by aspergillus inhalation, and early antimycotic therapy should be discussed. Background Russell et al. hypothesized that there might be a possible correlation[1] between gardening and serious damage to your health, based on the case of a man who had dispersed rotting tree and plant mulch in his garden, and who had developed an ARDS probably caused by Aspergillus fumigatus. According to his history, clouds of dust had engulfed him. The patient died on the ECMO. There was a similar patient in our hospital ten year ago, who died after dispersing rotting tree and plant mulch in the garden. This was the background for the presented case. Case Presentation A 54-year-old female patient presented at the Emergency Department of a local hospital reporting cough with respiratory distress. The patient denied active smoking and alcohol use, and had no allergies. The patient had passive cigarette smoke exposure from her husband for several years. Auscultation of the lung revealed a crackling noise. Laboratory examination showed that absolute white blood cell count was 12·2 109/l, C-reactive protein (CRP) was 190 mg/l, and procalcitonine (PCT) was 0·17 µg/l. The chest radiograph showed bilateral lung infiltrates. Therefore, the diagnosis of community-acquired pneumonia was made. The treatment with cefuroxime that had been started by the general practitioner three days earlier was changed to moxifloxacine (400mg/d) and piperacillin/ tazobactame (18g/d). Because of respiratory failure, non-invasive ventilation was started. Two days later, there was no improvement in the respiratory situation, so the patient was sent to our tertiary center. The patient had no history of immunosuppressive disease or treatment. Blood tests for HIV, hepatitis and screening for chronic autoimmune disorder were negative. The laboratory examination showed that absolute white blood cells were 24·0 109/l. Laboratory examinations revealed neutrophilia, but also lymphopenia with an elevated T4:T8 ratio (4·69). In addition, CRP was distinctly elevated (341mg/l), PCT was 0·4 µg/l, and the erythrocytes sedimentation rate was 70 mm/h. Electrocardiogram and echocardiogram did not show pathological signs. The respiratory failure was refractory to non-invasive ventilation and required intubation with controlled mechanical ventilation. The initial Horowitz Index was 56 mmHg. The CT scan showed bilateral diffuse interstitial infiltrates (Fig. 1), so all criteria for ARDS were satisfied[2]. Bronchoscopic examination showed unspecific inflamed mucosal lining. Bronchoscopic samples were taken and sent to the microbiology department. A broad- spectrum antibiotic therapy was started with meropenem (3g/d) and levofloxacine (1g/d). The initial microbiological tests of the blood samples and the bronchoalveolar lavage fluid (BALF) did not show any bacterial growth. The patient´s circulation destabilised. Due to a hypotensive condition, vasoactive support with norepinephrine (maximum 0·6µg/kg/min) and dobutamine (maximum 4·6µg/kg/min) was required, so all criteria for septic shock were fulfilled[3]. No significant improvement of gas exchanges was achieved (Horowitz Index 77mmHg). Consequently, ECMO with a venovenous bypass was implanted. The treatment of ARDS was further supported with methylprednisolone infusion[4]. Due to renal failure, it was necessary to start continuous veno-venous hemofiltration. Since no explanation could be given for the critical course, the family was asked again about special activities of the patient within the last few days prior to admission. The relatives reported that the patient had been digging up the garden, using non-fermented tree bark, which dispersed a large amount of dust two days before the symptoms developed. Without initial proof, we started empirical antifugal treatment with voriconazole (300mg/d), based on clinical course and a case report indicating aspergillus infection after using non-fermented tree bark.[1] Further lab reports subsequently displayed positive results for Aspergillus fumigatus IgG 255U/ml, Aspergillus fumigatus IgM 79 U/ml, and the galactomannan test was positive (aspergillus antigen: 4·6). Microbiological examination of the BALF revealed growth of Aspergillus fumigatus fungus hyphae (Fig. 2). No bacteria were cultures from the BALF. Because of the increasing azole resistance to Aspergillus fumigatus across Europe and the critical course of the patient, we also started the therapy with caspofungin (50mg/d) one day after initiating antifugal therapy with voriconazole. The patient responded to the therapy immediately with dramatic clinical improvement. We were able to reduce the catecholamine support, and the extracorporal support could be discontinued on day 7. The patient was successfully weaned from the ventilator two days later. On day 7 of antifugal treatment, aspergillus antigen was no longer detectable. A CT scan showed a partial resolution with residual areas and a partial consolidation in the basal segments of both lobes. The patient was discharged to rehabilitation 19 days after admission. Discussion To our knowledge this is the first case of an A. fumigatus sepsis after plant mulch dispersion. Aspergillus spores are often found on decaying plant matter. The inhalation of aspergillus spores can result in allergic broncho-pulmonary aspergillosis, pulmonary aspergilloma, or pulmonary aspergillosis. Sepsis seems to be very seldom. The published case[1] and our cases did not have immunosuppression, but all had epithelial alteration due to smoking, passive smoking (like our patient), or recurrent bronchitis. Perhaps these factors cause damage to the epithelium that predisposes for Aspergillosis fumigatus or could increase susceptibility. It has been reported that, for example, marihuana smoking is associated with aspergillosis. Chronic respiratory disease like COPD also increases the susceptibility of getting aspergillosis[5]. One might speculate that the extreme exposure to aspergillus caused an acute respiratory failure due to an acute hypersensitivity reaction, but the clinical course is extremely unusual. The clinical symptoms started two days after the exposure. The discontinuation caused no clinical amelioration. To our knowledge, no case of hypersensitivity pneumonitis is described that leads to mechanical ventilation. The aspergillus antibodies and microbiological examination support the assumption that the sepsis responded to the antimycotic therapy, and we could not observe an acute hypersensitivity reaction, which responded to the steroid treatment. Conclusions From our perspective, it was the combination of early antimycosic treatment (although we had no confirmation of the aspergillosis at that point of time), and lung replacement therapy by veno-venous ECMO that made it possible to save our patient. Doctors should be aware that signs of sepsis after gardening may be caused by aspergillus inhalation and early antimycotic therapy should be discussed. Competing interests The author(s) declare that they have no competing interests. Author’s contribution SM, SS, AJ, TV took care of the patient in the intensive care unit. EW analyzed and interpreted our patient's radiological data. FS and CA performed microbiological and virological analyses. NJ, CV, AH, RK took care of the patient in the intensive care unit, performed the literature review and drafted the manuscript. All authors read and approved the final manuscript. Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal. References 1. 2. 3. 4. 5. Russell K, Broadbridge C, Murray S, Waghorn D, Mahoney A: Gardening can seriously damage your health. Lancet 2008, 371(9629):2056. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS, Force ADT: Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012, 307(23):2526-2533. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R et al: Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 2013, 39(2):165228. Marik PE, Meduri GU, Rocco PR, Annane D: Glucocorticoid treatment in acute lung injury and acute respiratory distress syndrome. Crit Care Clin 2011, 27(3):589-607. Zmeili OS, Soubani AO: Pulmonary aspergillosis: a clinical update. QJM 2007, 100(6):317334. Figures Figure 1 CT scan showing (A) initial bilateral diffuse interstitial infiltrate and (B) the partial resolution with residual areas and a partial consolidation in the basal segments after starting treatment. Figure 2 Shows microscopy of Aspergillus fumigatus (A), displays Aspergillus fumigatus growth on nutrient agar (B).