第 二 部 分
advertisement
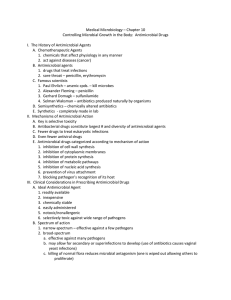
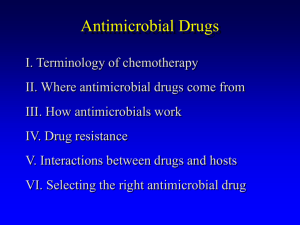
Introduction to antimicrobial agents 1. Chemotherapy,化学治疗 Definition: Use of drugs to combat infectious diseases and cancer. Antimicrobial drug (抗微生物药) Antiparasitic drug( 抗寄生虫药) Anticancer drug (抗癌药) Antimicrobial drug Antimicrobial drugs either kill microbes (microbicidal) or prevent the growth of microbes (microbistatic). Antibacterial Antiviral Antifungal Antiparasitic Antimicrobial Chemotherapy Differential toxicity: based on the concept that the drug is more toxic to the infecting organism than to the host Majority of antibiotics are based on naturally occurring compounds or may be semi-synthetic or synthetic What is the ideal antibiotic Have the appropriate spectrum of activity for the clinical setting. Have no toxicity to the host, be well tolerated. Low propensity for development of resistance. Not induce hypersensitivies in the host. What is the ideal antibiotic Have rapid and extensive tissue distribution Have a relatively long half-life. Be free of interactions with other drugs. Be convenient for administration. Be relatively inexpensive Definitions Spectrum of Activity: Narrow spectrum - drug is effective against a limited number of species Broad spectrum - drug is effective against a wide variety of species Gram negative agent Gram positive agent Anti-anaerobic activity Definitions Minimum Inhibitory Concentration (MIC) - minimum concentration of antibiotic required to inhibit the growth of the test organism. Minimum Bactericidal Concentration (MBC) - minimum concentration of antibiotic required to kill the test organism. Bacteriostatic Bactericidal Definitions Chemotherapeutic Index ( CI ): LD50/ED50 or LD5/ED95 PAE (Post antibiotic effect): the continued suppression of antibacterial growth after the administration of antibiotic has ceased and serum concentrations have fallen below the minimum inhibitory concentration . 机 体 抗菌作用 抗微生物药 耐药性 病原微生物 Five modes of antimicrobial action (i) (ii) (iii) (iv) (v) Inhibition of cell wall synthesis Disruption of cell membrane function Inhibition of protein synthesis Inhibition of nucleic acid synthesis Action as antimetabolites Peptidoglycan The glycan backbone Tetrapeptide side chain Peptidoglycan cross-bridges Targets of antimicrobial drugs ——Disruption of cell membrane function— — Cationic and alters cytoplasmic membrane Polymyxin permeability by binding to a negatively charged site in the lipopolysaccharide layer Amphotericin B Associates with ergosterol, the main component of fungal cell membranes Drugs that disrupt cell membrane function Inhibition of protein synthesis Generally work at different stages of prokaryotic mRNA translation into proteins, like initiation, elongation (including aminoacyl tRNA entry, proofreading, peptidyl transfer and ribosomal translocation) and termination.) The antibiotic only affects 70S ribosomes in the bacteria and does nothing for the 80S ribosomes in human. Inhibition of protein synthesis Macrolides Lincomycin Chloromycetin Tetracyclines Aminoglycosides bind to 50s bind to 30s Inhibition the Synthesis of metabolites Antibiotics that mimic the structure of the specific substrate that the normal substrate is replaced and don’t have contact with the enzyme which acts on a substrate to produce a certain metabolically important metabolite inside the cell. Action of sulfanilamide —— Inhibitors of nucleic acid synthesis— — Quinolones Inhibit the DNA gyrase→ Interfer with DNA replication Rifampicin Inhibits DNA-dependent RNA polymerase →mRNA↓ Antimicrobial resistance Resistance: the inability to kill or inhibit the organism with clinically achievable drug concentrations Resistance may be innate (naturally resistant) Resistance may be acquired - mutation - acquisition of foreign DNA Antimicrobial resistance Factors which may accelerate the development of resistance - inadequate levels of antibiotics at the site of infection - duration of treatment too short - overwhelming numbers of organisms - overuse / misuse of antibiotics Antimicrobial resistance General mechanisms of resistance: Inactivation / destruction of antibiotic Altered binding site Altered permeability Efflux (pumps) mechanisms Bypass of metabolic pathways Resistance gene transmission Principles of use of antibacterial agents Proper selection of an antibacterial agent is based on a number of factors. The identity of the pathogen The site of infection Pharmacokinetics (PK) Pharmacodynamics (PD) Potential toxicity Possible drug interactions, Cost, and convenience of administration. Prophylaxis for infection Prevention of Rheumatic Fever Epidemic cerebrospinal meningitis Infective endocarditis Surgery