Eis_-_Opioid_Analgesics
advertisement

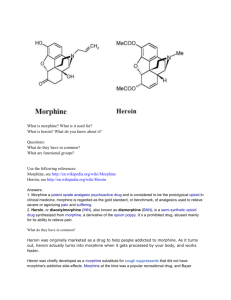
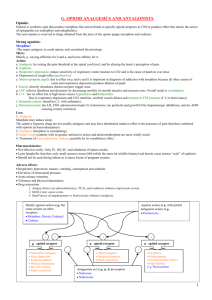
Eisenberg – Opioid Analgesics – NS Exam 2 Uses Pain relief - dull, visceral pain Antitussive effects Treatment of diarrhea Acute pulmonary edema Morphine & codeine Origin o Phenanthrenes - morphine, codeine, thebaine o Benzylisoquinolines - papaverine and noscapine Structural comparisons o Morphine OH o Heroine OCOCH3 deacetylated morphine – crosses BBB 2.5 x faster o Codeine OCH3 o Nalorphine OH o Naltrexone OH Pharmacological effects o Mechanism of action - opioid receptors Specific opioid receptors in brain and spinal cord - binding sites. Why? Endorphins! Endogenous ligands ß-endorphin – likes all kinds of receptors leu/met-enkephalin dynorphin Neuronal mechanisms are slowly being worked out - possible mechanism Spinal sites – pain pathways o Close voltage-gated Ca++ channels to prevent presynaptic neurotransmitter release o Hyperpolarizing post-synaptic membranes by opening K+ channels Brainstem GABA normally inhibits pain inhibitory neurons Opioids activate pain inhibitory neurons indirectly by inhibiting GABA activity results in enhanced inhibition of nociceptive processing in the dorsal horn Supraspinal sites exogenous μ-opioids may cause the release of endogenous agents endogenous agents may act at ∂ and k-binding sites this may result in a change in pain threshold – imp in terminal pts There are 7 transmembrane regions and g-protein coupled activity o Sequence similarities between types of receptors differences in the amino terminus region and the 2nd and 3rd extracellular loops suggesting specificity in ligand binding binding to transmembrane domains is responsible for high affinity binding Exogenous ligands Name recognition Effects on various systems o CNS Analgesia dull, visceral pain changes in the pain threshold codeine has a ceiling effect & there has limitations for more severe pain Behavior - euphoria, sedation o o o o o o o dopamine at the nucleus accumbens pleasure patients receiving opiates for acute pain show significantly less euphoria Miosis - μ/k effect (parasympathetic effect on the pupil) – heroin addicts always have this Respiratory depression - depression of neurogenic, pCO2, pO2 drives Chemoreceptor trigger zone Causes vomiting!! until tolerance develops Apomorthing-dopaminergic agonist Probably a vestibular component because ambulation aggravates this antitussive effects lowers the seizure threshold hypothermia endocrine increases ADH decreases ACTH, LH, PIF, and TSH when given chronically (no sex crazed heroin addicts) Cardiovascular system In the healthy, supine patient, there is little effect on HR, BP, or the myocardium Orthostatic (change in posture) hypotension histamine release - may cause flushing and itching of the blush area direct morphine effect on the blood vessels and through the central vasomotor centers hypotension is a particular problem if there is reduced blood volume Cerebral circulation lowered respiration may increase pCO2 and result in cerebral vasodilation and CSF pressure -may aggravate a head injury Useful in MI or in patients with pulmonary edema due to acute left ventricular failure pain relief peripheral vasodilation is an advantage here – lowers the work load of the heart R side heart weakness – not pumping adequately leg swelling L side heart weakness backup is in lung which is why ppl take diuretics Gastrointestinal system Increased tone: spastic paralysis ( constipation) and decreased peristalsis a direct and central action of opioids severe constipation - treatment for diarrhea treat with a laxative etc Increased biliary tract pressure meperidine is a better choice for renal colic Genito-urinary system Spasm of the ureter Reduced urine production due to ADH release - μ effect Sexual activity is depressed depression of hypothalamo-pituitary-gonadal axis Labor may be retarded and the neonate depressed - little fetal blood-brain barrier to morphine addicted neonate – have to wean them with opium Immune function Generally suppressive - a μ -effect Chronic effects Apparently no long-term pathology due to opioids Tolerance (cross-tolerance) pharmacodynamic: mechanisms behind dev of tolerance – change in neuronal system metabolic does not occur uniformly to all effects Dependence (cross-dependence) o o o withdrawal effects – neurons change to accommodate presence of opioids over time so that they function normally in presence of this drug. When take opioid away they decomensate! a NON-ISSUE in the terminally ill Mechanisms for tolerance/dependence Dysfunction between the opiate receptor and the G-protein complex so the opioid is less effective A change in the NMDA receptor action - a learning phenomenon involving the interaction between pre- and post-synaptic events antagonism of the receptor with ketamine prevents tolerance development Uncoupling of the μ/Δ dual receptor complex - complex appears necessary opioid action Tolerance to chronic effects: Something new on the horizon - an opiate pain-reliever without tolerance and physical dependence? Using a μ-agonist and a Δ-antagonist provides pain relief without tolerance/dependence mice without Δ-opioid receptors don’t show tolerance/dependence Drug combinations are being developed for trials Absorption, distribution, metabolism, excretion o Absorption is rapid by all parenteral routes morphine - 15-49% is available when given orally - first pass metabolism codeine - 70% available, much higher oral/parenteral ration o Blood-brain-barrier is significant for morphine heroin (diacetyl-morphine) crosses o Metabolic breakdown conjugation occurs mainly in the liver heroin is deacetylated after passage into the brain - converted to morphine o Most is excreted in 24 hours Side/toxic effects o Common: dizziness, dysphoria, nausea, vomiting, constipation, o Possible: biliary colic o Allergic reactions o Hypotensive reactions an antihistamine is sometimes included in a vial for IM administration o Respiratory problems caution - pre-existing conditions o Opioid overdose – naloxone, nalmefene (longer acting) Drug interactions o tricyclic antidepressants, phenothiazines, and barbiturates enhance respiration depression Tramadol - Ultram o A synthetic codeine analog approved for mild to moderate pain, used in Europe for many years o Mechanisms binds weakly to μ-opioid receptors inhibits biogenic amine reuptake enhances serotonergic neurotransmission o Good orally, active half-life of drug and one metabolite is 5-9 hrs.. o Causes less nausea and constipation than morphine o Morphine was still rated superior o CNS side effects: nausea, dizziness, constipation, sedation, and headache Associated with seizures, contraindicated where there is a history of epilepsy o No more effective than codeine with aspirin/acetaminophen, and expensive o Since pain relief may be independent of opioid receptors, it may be useful in chronic neuropathic pain o Post-marketing survey shows an abuse liability o A metabolite of tramadol has μ-agonist activity and will substitute for morphine to prevent withdrawal o High doses (200-400mg) are required for this effect Methadone and prophoxyphene o Methadone (DOLOPHINE) properties and uses good oral long-acting analgesic - currently expanding in use extended duration of action (8+ hrs) withdrawal effects are less severe - useful in heroin detoxification well absorbed by all routes side effects are similar to morphine tolerance develops more slowly LAAM - long-acting, recently approved methadone analog (2-3 day dosing) o Prophoxyphene (DARVON) properties and uses dextro form has analgesic activity about half as potent as codeine for analgesia well absorbed by all routes toxic doses produce CNS and respiratory depression abuse potential is lower than codeine - pleasurable effects are different Meperidine (Demerol) and analogs o Comparison with morphine good oral/parenteral ratio shorter duration of action 2-4 hrs o Pharmacologic actions CNS actions are similar to morphine equivalent analgesia shorter duration CV effects antimuscarinic effects may cause tachycardia negative inotropic effect has been reported Smooth muscle effects less constipation (diphenoxylate and loperamide are commonly used) less spasm of the biliary tract and ureter Absorption, fate, and excretion Absorption is rapid by all routes Metabolism occurs mainly in the liver 60% is excreted in the urine Side/toxic effects Side effects are like morphine plus atropine-like effects Normeperidine accumulation causes seizures o when given in high doses o in patients with renal compromise o responsible for the gravitation from meperidine to morphine in the ER Drug interactions tricyclic antidepressants, phenothiazines, and barbiturates enhance respiration depression CNS excitation with MAO inhibitors - probably due to an increase of normeperidine Therapeutic uses Indications are similar to morphine for analgesia Fentanyl and analogs (sufentanil, alfentanil, and remifentanil) are used for short-term anesthesia and for chronic treatment in the terminally ill o patches or lollipops are newer approaches to maintain adequate blood levels o new buccal tablet for “breakthrough” pain acts very rapidly Opioid antagonists Properties of naloxone, naltrexone, and nalmefene o pretreatment prevents the action of the agonist o administration of antagonist in a chronic user will precipitate withdrawal Used in heroin overdose - naloxone (t.= 1-2 hrs.), naltrexone and nalmefene (t.≈10 hrs.) Naltrexone (oral) is available to prevent a relapse into drug-taking behavior in high risk patients mu-receptor antagonist that doesn’t cross BBB o Methylnaltrexone (Relistor) for pts getting pallitave care given sc every other day reduces constipation – produces GI side effects: abd pain, flatulence, diarrhea o Alvimopan (entereg) to relieve postop ileus (bowel obstruction b/c peristalsis stops) floow partial large or small bowl resection Partial agonists Effects depend on administration o agonist effects when given alone o antagonist properties when administered after an opioid agonist Differential actions on specific opioid receptors Nalorphine o Effects k-opioid effects - analgesia, miosis, respiratory depression, dysphoria when given primarily precipitate withdrawal in chronic users when given secondarily because it blocks mu-receptors o Used to diagnose physical dependence Pentazocine (TALWIN) o May increase HR and BP o Uses and effects good oral, low level analgesic drug of choice if addiction problem exists does not substitute for other opioids to sustain dependence may precipitate withdrawal in chronic abusers oral form is combined with naloxone to prevent dependence relapse> Newer partial agonists o Butorphanol (STADOL) actions are similar to pentazocine (increase in HR and BP) morphine is preferred in patients with cardiac problems for moderate to severe pain low abuse/dependence liability better for acute rather than chronic pain causes dysphoria and has limited potency o Nalbuphine (NUBAINE) also has shown some success as an analgesic causes dysphoria and has limited potency abrupt removal will result in characteristic withdrawal signs may precipitate withdrawal in an individual already taking a low dose of morphine no cardiovascular stimulation as with pentazocine and no hypotension as with morphine o Buprenorphine (BUPRENEX) can be used as an analgesic because of μ-agonist activity will antagonize the action of morphine if given secondarily because of high μ-agonist affinity but low intrinsic activity it can serve as a good substitute in heroin maintenance has been found to be useful in reducing craving for heroin or cocaine during the withdrawal period -a major advance in treatment now available in combination with naloxone – SUBOXONE Antitussive agents Codeine or an analog Dextromethorphan o d-isomer of methoxylated levorphanol Benzonatate o a polyglycol derivative related to procaine o may act on cough or stretch receptors in the lung, and by a central mechanism Therapeutic use of opioids Guidelines o what is the biggest recent advance in pain treatment? - pain level is now a routine vital sign o administration for pain, cough or diarrhea is only symptomatic treatment o adequate post-operative pain treatment yields a better outcome o concern for dependence development is overdone - surveys suggest undermedication (especially true of children) o chronic use is undesirable o alternative treatments for chronic pain conditions should be sought o dependence in the terminally ill should NOT be a consideration good maintenance doses provide for smaller step increases patient-controlled medication Selecting a drug o for moderate pain choose codeine good orally- sustained-release forms of morphine and oxycodone are available often combined with aspirin or acetaminophen o meperidine is the drug of choice for biliary/renal colic o select a short-acting drug when required for diagnostic procedures o methadone is widely used as a substitute for heroin o naloxone or nalmefene i.v. to reverse respiratory depression in opioid overdose o dyspnea due to left ventricular failure is relieved by morphine o loperamide or diphenoxylate for diarrhea