04-Lecture of endocrine system (Updated 28 April)
advertisement

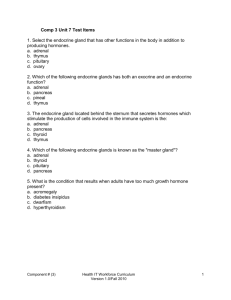
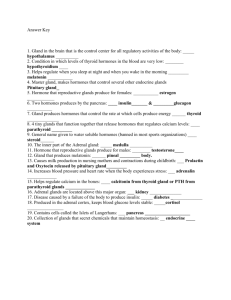
Endocrine glands (cells) Hormone secreting cells or glands. May be in a form of scattered cells as enteroendocrine cells of GIT.OR in a form of gland as pituitary and thyroid glands. Endocrine glands have cells that arranged in columns or cords separated by fenestrated blood capillaries EXCEPT thyroid gland in which cells are arranged to form follicles. Hypophysis (pituitary gland) •Development of Hypophysis (pituitary gland) Hypophsis (pituitary gland) It develops from 2 different tissues: 1-Ectodermal epithelial tissue: of the roof of the developing mouth---Rathke’s pouch giving Adenohypophsis (Anterior pituitary). 2-Ectodermal neural tissue of dienchephalon---Neurohypophsis (Posterior pituitary). Parts of hypophsis 1-Adenohypophysis 2Neurohypophysis a-Pars distalis. a-Pars nervosa. b-Pars tuberalis. b-Infundibulum. c-Pars intermedia. c- Median eminence. Blood supply and control of secretion Superior hypophseal arteries supply the pars tuberalis and the infundibulum and give primary capillary plexus in the median eminence. Inferior arteries supply the pars nervosa and send few branches to the ant. lobe The hypophseal portal system of veins delivers neurosecretory hormones from the primary capillary plexus of the median eminence to the secondary capillary plexus of the pars distalis. These hypothalamic hormones stimulate or inhibit the secretion of cells of pars distalis. Pars nervosa (Neurohypophsis) Does not contain secretory cells. • Does not contain cell bodies of neurons. • Is rich in unmyelinated nerve axons. • Is rich in fenestrated blood capillaries. • Contains Herring bodies that contain vasopressin (ADH) & oxytocin H. that are secreted by hypothalamus (. • Contains supporting glial cells called pituicytes. • Adenohypophysis (anterior pituitary) • Pars intermedia : Contains cysts full of colloid &lined with cuboidal epith.It may contain cords of basophils that secrete MSH. • Pars tuberalis : It surrounds the hypopheseal • (neural)stalk of neurohypophysis Most of its cells are basophilic gonadotropic cells that arranged in cords separated by blood capillaries and portal system • • Pars distalis : 1-Chromophobes: Have no affinity to stain. Are small pale cells. Undifferentiated cells. 2-Chromophils: Have an affinity to the stain. They are 2 groups: I-Acidophils include a- Somatotrophs that secrete somatotropin or growth H b-Mammotrophs that secrete mammotropin or prolactin H. II-Basophils include a-Thyrotrophs that secrete TSH. b-Corticotrophs that secrete ACTH. c-Gonadotrophs that secrete 2 types of hormones: -FSH in females it stimulates follicular maturation. In males it stimulate spermatogenesis. -LH in females it stimulates ovulation. In males it stimulate Lyedig cells(interstitial cells) to secrete testosterone. Anterior pituitary (Adenohypophsis) Medical application Pituitary benign tumors. Effects of pituitary Hormones on the mammary gland. Prolactin---stimulate milk formation. Oxytocin---stimulate milk ejection Parathyroid glands They are 4 glands on the post.of thyroid gland. Each gland has its capsule and thin septae. The parenchyma is formed of chief cells, oxyphil cells, blood capillaries and adipose tissue (in adults). Chief cells are slightly eosinophilic, rich in rER and secrete parathyroid hormone ( bl.calcium). Oxyphil cells are, arranged in groups or clusters, deep eosinophilic (rich in mitochondria and glycogen) and of unknown function (inactivated chief cells). Thyroid & parathyroid glands Parathyroid gland Post. lobe of pituitary Ant. lobe of pituitary Parathyroid gland Thyroid gland Is covered by CT.capsule that sends septae to divide it into lobules. Its parenchyma is formed of follicles that are separated by reticular fibers, parafollicular cells and fenestrated blood capillaries. The follicles are formed of follicular cells (squamous to columnar) & contain colloid. Follicular cells are basophilic, and rich in RER, mitochondria and apically located lysosomes. Parafollicular cells secrete calcitonin (decreases Bl.Calcium level). Thyroid follicles and parafollicular cells (clear cells) Follicular cells Parafollicularcell Suprarenal (adrenal) glands It has a thick capsule that sends septae. Suprarenal cortex (80% of the gland) produces mineralocorticoids, glucocorticoids (cortisol and corticosterone), and androgens. The cortex is regulated by ACTH of ant. Pituitary and angiotensin II. Suprarenal medulla produces epinephrine and norepinephrine and is regulated by the sympathetic nervous system. The cortex is rich in fenestrated (without diaphragm) sinusoidal capillaries. The medulla receives a dual blood supply: a. from cortical arteries and b. from cortical capillary beds. Adrenal gland It is formed of: I. Cortex that is composed of: A-Zona glomerulosa. B-Zona fasiculata. C-Zona reticularis. II.Medulla Adrenal gland Adrenal cortex: zona glomerulosa *Is formed of cords and clusters of small columnar cells that are rich in SER and mitochondria. *Produces Aldosterone hormone that affect renal distal tubules. Adrenal cortex: zona fasiculata (spongiocytes) *It is the intermediate and the largest layer of the cortex. *It is formed of columns of large polyhedral cells that are separated by longitudinal sinusoidal capillaries. *It cells are rich in lipids so they appear empty (spongiocytes). *Its cells are rich in mitochondria (tubular cristae),SER and lipofucin pigment. *Its cells secrete glucocoticoids. *It is regulated by ACTH of pituitary. Adrenal cortex:zona reticularis. *It is the innermost layer of adrenal cortex. *It is formed of anastomosing cords of deep acidophilic cells. *Its cells contains few lipofucin and lipid droplets. *The cells secrete androgens. Medulla of adrenal gland *It the central portion of the adrenal gland. *It is completely invested with adrenal cortex (not separated from it by CT. septa) *It is formed of: 1. Chromaffin cells that contains granules of catecholamine as that of sympathetic NS.(They produce epinephrine and norepinephrine). They stain deep brown with chromic salts. 2. Sympathetic ganglion cells scattered in CT. Relay on chromaffin cells. Adrenal gland Thyroid gland