Physical properties
advertisement

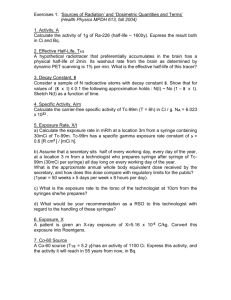
RDIOPHARMACY Diagnostic Nuclear Medicine Nuclear Medicine is the branch of medicine concerned with the use of radionuclides in the study and the diagnosis of diseases. •The radionuclides are used for: 1–the assessment of organ function, 2–the detection of disease, 3–the treatment of some diseases and 4–the monitoring of the effects of treatment The importance of Nuclear Medicine •It provides: 1–physiological information not available from other imaging modalities 2–diagnostic information of pathological processes before the outset of structural changes in an organ •It uses very small amounts of radioactive material (radiopharmaceutical) that is introduced into the body and acts as a tracer Information obtained using nuclear medicine techniques is more comprehensive than other imaging procedures because it demonstrates organ function not just structure •The result is that many diseases and cancers may be diagnosed much earlier Nuclear medicine vs. other modality – γ rays are used for imaging – β rays are used for therapy in nuclear medicine – Nuclear medicine shows the functions of the organs and less anatomic information – Computed tomography, magnetic resonance, ultra sonography and plain films show the anatomy of the organs and less of the functions What is radiopharmacy? It is a science which deals with the preparation and dispensing of radiopharmaceuticals(RFs) (radiolabel drugs) What are RFs? Rfs are radiolabel drugs that are used for diagnosis and treatment Characteristics of RPs •The mass amount administered is low •No intrinsic pharmacological effect •For diagnostic use –No disturb physiologic parameter •For therapeutic use –Radiation produced the desired therapy Tow kinds of RPs 1-Diagnostic RPs 2-Therapeutic RPS Diagnostic RPs Physical properties •For physical properties of the radionuclide must be considered: 1.Physical half life 2.Decay mode 3.Emitted photon energies 4.Availability Physical properties Physical half life •The half life is the time required to reach ½of undecayed atoms at 0 time (Tc-99m 6 hours, I-131 8 day) •Too-long lived RF: unnecessary body irradiation occurs Physical properties Photon energy •The sensitivity and the resolution of the gamma camera system depends on photon energy •The energy must be high enough that it escapes the body without being attenuated and must be also low enough to be detected by the crystal •The gamma camera electronics detect radiation in the 60-400keV •The ideal energy should be in the range of 100-200keV Physical properties Decay mode •Imaging procedures require an electromagnetic photon (x or γ ray) •The emitted photon must be high abundance and be monoenergetic •β and α rays are not detected •For diagnostic use a pure γ emitting decay mode would be desirable Physical properties Availability •The most readily available radionuclide is Tc-99m pertechnetate •Tc-99m is eluted from a Mo-99/Tc-99m generator •The parent Mo-99m decays with a half life of 66 hours resulting in a shorter lived (6 hours) daughter (Tc-99m) •A new generator is purchased once a week and supplies all the Tc-99m needed for that week Radiopharmacy Biological properties •The ideal RP should do the following –Localize rapidly and exclusively in the organ of interest –Localize more in pathologic tissue –Be metabolically and pharmacologically inert –Have no side effects –Clear rapidly from background tissue –Be rapidly excreted after the study is completed Biological properties Mechanism of localization •Functional: –Passive transfer (diffusion) Tc-99m DTPA –Active transport or uptake (I-131 in thyroid –Metabolic trapping (F-18FDG) –Receptor binding (In-111 pentetreotide) –Antibody binding (Tc-99m arcitumomab) Biological properties Mechanism of localization •Mechanical –Capillary blockage (Tc-99m MAA) –Phagocytosis(Tc-99m sulfur colloid) –Sequestration (heat denatured Tc-99m RBCsfor spleen –Compartmental space localization (In-111 DTPA for CSF flow –Abnormal extravasations (Tc-99m IDA in bile leaks) Biological properties Route of administration •The route of administration often determine the localization characteristic of RFs – IV is the main route --Lung ventilation can be studied by inhalation of an aerosol or gas –Different biodistributions and kinetics can be obtain by selecting the route of administration Biological properties Target uptake •The RF with a better uptake is a superior imaging agent (target to nontarget ratio) •The rate of uptake is also important –The thyroid can be imaged at 20 min with Tc-99m pertechnetate , but 4-6 hours with I-123 NaI Biological properties RF excretion •The RF must clear from blood and background tissue to achieve high contrast •The major excretion routes are –Kidneys (glomerular filtrations) –GI tract –Hepatobiliary route Chemical properties •Ease of preparation and availability •Tc-99m-based RFs from ready to use commercial reagent kits •Stability and expiration –The best Tc-99m kit formulation give products that are stable at least 6 hours after preparation •Stabilized bone scan kits are preferable to non-stabilized kits Thank you and Good Luck Prof. Dr. Omar Shebl Zahra SKELETAL IMAGING Bone Scan(Scintigraphy) Bone scan: A technique to create images of bones on a computer screen or on film. A small amount of radioactive material is injected and travels through the bloodstream. It collects in the bones, especially in abnormal areas of the bones, and is detected by Gamma Camera. Bone scans are used for the detection and monitoring of disorders affecting the bones, including cancer, infections, and fractures. Bone scanning is also helpful in evaluating joint diseases. A bone scan is a test used to detect areas of the bones that are undergoing rapid turnover due to damage to the bone or new bone formation. Skeletal - imaging agents Overview Tc-99m labelled bone agents are useful in the detection of bone lesions that are associated with high metabolic activity such as tumours, metabolic disorders, and infections of the bone. The imaging advantages of Tc-99m, coupled with the sensitivity of bone agent localization in skeletal bone hydroxyapatite matrix, allows for detection of bone pathology before evidence is shown by conventional x- rays. Tc-99m bone agents. There are many different forms of Tc-99m bone agents, with minor differences in their individual chemical structure. Currently used bone-imaging agents are based on either the P—C—P diphosphonate structure, including Tc-99m medronate disodium (MDP) and Tc-99m oxidronate. Or (in the past) the inorganic P—O—P phosphate structure, such as Tc-99m pyrophosphate. These bone agents exist as: sterile ,pyrogen free radiopharmaceuticals ready for IV injection after reconstitution (labelling) with Tc-99m pertechnetate. -. Technetium Tc 99m Medronate (MDP) Physical properties (1) All of the Tc-99m bone- imaging agents are susceptible to radiological decomposition with re-oxidation of the Tc-99m to a higher valence state. These agents sometimes include antioxidants (e.g. , ascorbic acid) in their formulation to improve their in vitro stability. (2) They should be stored at room temperature before and after reconstitution. Bio-distribution It is believed that the localization of the diphosphonates occurs by chemisorptions onto the hydroxyapatite mineral matrix of skeletal bone with uptake related to bone metabolic activity and bone blood flow. Administration and dosage IV, 20 mCi (740 MBq) CLINICAL PHARMACOLOGY During the initial 24 hours following intravenous injection of technetium Tc-99m medronate, about 50 percent of the dose is retained in the skeleton, and about 50 percent is excreted in the urine. A minimum amount of uptake has been observed in soft-tissue organs, most notably the kidneys. Clearance of radioactivity from the blood is quite rapid, with about 10 percent of the injected dose remaining at one hour, and less than 5 and 2 percent at two and four hours, respectively. The rapid blood clearance (T 1/2 38 to 75 minutes) provides bone to non-osseous tissue ratios(target to non target ratio) favouring early imaging. Following intravenous administration of Tc- 99m MDP , skeletal uptake occurs as a function of blood flow to bone and bone efficiency in extracting the complex. Deposition of radioactivity in bone is rapid and appears to be related to osteogenic activity as well as the afore mentioned skeletal blood perfusion , skeletal uptake is bilaterally uniform, with larger concentrations in the axial structure and in the long bones. Increased accumulation of radioactivity may be seen, generally, in any bone disease state in which there is increased oestrogenic activity or a localized increase in osseous blood perfusion. Adverse Reactions Adverse reactions have not been reported that are specifically attributable to the use of technetium (99mTc) MDP. This is also noted with most radiopharmaceuticals used in nuclear medicine studies. Allergic dermatological manifestations (erythema) have been infrequently reported with other similar agents. Radiation Dosimetry The effective half-life was assumed to be the physical half-life for all calculated values. The estimated radiation absorbed doses to an average patient (70 kg) from an intravenous injection of a maximum dose of 740 MBq (20 mCi) of technetium Tc 99m MDP. How to calculate dosage based on body weight? We never use pounds in medicine - it's always kilograms. The first thing you need to do is convert the patient's weight from pounds to kg. (Divide by 2.2) Then you multiply the dose (given in dose per kg) by the weight in kg. Example: Pt weighs 154 pounds. Divide by 2.2 = 70 kg Dose of 2.5 mg/kg: 2.5 x 70 = 175 mg Dose Calculation in Nuclear Medicine Adult dose are designed for 70 kg body weight Pediatric dose = adult dose x body weight in kg / 70 Thank you and Good Luck Prof. Dr. Omar Shebl Zahra