Exhibit A – New StarPanel Views
advertisement

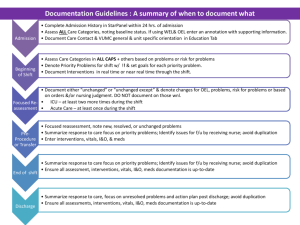
Nursing Documentation Re-Design FAQ: How can I view Inpatient Nursing documentation in StarPanel? What data has changed? Most of the changes to Nursing Documentation will not impact team views of key nursing data. The work focused on standardizing and streamlining documentation (Peds and Adults). It should effectively communicate the “patient story” and meet regulatory requirements. For the Sept 15 pilot release on pediatrics 8A/8B/8C and adult 8N/8S: No change o No changes to trended numeric data (Vital Signs, I&O) and devices (Vents, VAD, etc.) o No new changes to the Nursing admission history o No changes to current practice and/or policies (what & how often) – but changes to documentation Modified charting by exception by Care Category (Neuro, Pain, Activity/Musculoskeletal, Psych, etc.) using WNL, WEL, OEL, or a specific problem. Definitions: HED View o o o o WNL – Within normal limits. Meets standard, published criteria for developmental age. WNL requires no further documentation except: RASS SCORE, BRADEN (Pressure Ulcer Risk), and FALL RISK STATUS are required q shift WEL – Within expected limits. Doesn’t meet criteria for WNL, but is normal or a new normal for the patient. WEL requires x1 documentation of the patients baseline (Musculoskeletal = WEL Amputee x 10yrs). OEL – Outside expected limits - Does not meet criteria for WNL, WEL or Problem (see definition). OEL level requires supportive findings and focused re-assessment (RASS=1). Only abnormal findings are charted unless part of Risk Scale criteria (i.e. Glascow Coma Scale). Nursing Problems –A nursing problem is a significant focus of the nursing plan of care (e.g. Incision, Pressure Ulcer, Confusion, CO alt, Violence, etc.). Problem requires supportive findings, goals and focused reassessment. Those with a significance flag (red) are shift priority problems. Documenting re-assessment “unchanged” (within the nurse’s shift) if there was no change in the patient condition. This should allow condition changes to standout. Example, for q1h neuro-vascular checks – you would see all the initial values and then “unchanged” q1h documented if no changes. Simplified interventions and patient education Care Plan changes o Nursing Summary & Plan Priorities & Goal status are now Response to Care/Recommendations o Focus on Discharge Readiness New StarPanel views (see attachments): o Updated plan of care in OPC, Team Summary, and Integrated Presence; o 3 Customizable Flowsheets: NSG_DATA+, NSG_CARE, NSG_PLAN Updated: 3/19/2016 10:31 PM by Ariosto Nursing Documentation Re-Design Documentation Reflects Standards of Care Baseline Assessment: On admission, establish a baseline against which to evaluate changes in patient physiological, functional, developmental and behavioral health status. This includes pertinent medical, procedural and medication history as well as home medical equipment, therapies and duration of therapy. Initiate high risk screening as warranted/ required (influenza, sleep apnea, nutrition, abuse, pregnancy risk, lactation). Special populations require additional screening (e.g. OB, neonate, psych). Note significant conditions and devices present on admission (e.g. pressure ulcer, CVC) not already noted. Any cultural/religious consideration should be noted if relevant. Initiate individualized care plan. Shift/Assigned Caregiver Change Assessment: Assessments (including devices) shall be performed at a minimum, every shift, with change in level of care or more often if instability or risk exist for all inpatients (adult, peds, acute, critical). Additional assessments may be required. Focused Assessment: Abnormal, unexpected findings or patients with significant risk of problems may merit further assessment and intervention. Interventions include monitoring, treatment as ordered and those within scope of practice, patient and family education referrals/escalation as warranted. Findings of risk will dictate the frequency of the focused assessment. Devices: Any line, tube, appliance, equipment connected to the patient for monitoring or treatment of illness or injury. Devices are assessed per policy or practice guidelines including (1) patient’s response to current level of device support; (2) setting check; and (3) proper functioning of equipment. Updated: 3/19/2016 10:31 PM by Ariosto Nursing Documentation Re-Design Exhibit A – New StarPanel Views Available from FLOWS & Actions Menu (after there is 24 hrs of documentation) 1 FLOWSHEET NAME NSG_DATA+ 2 NSG_CARE 3 NSG_PLAN NURSING CONTENT Trendable Data: All Vital signs (non-invasive, invasive) Pain# and Scale Height, Length, Weight Risk Section: Total Score/Status: Braden, Fall, PEWS, GCS, etc. I&O, IV Drips Device data (Vents, ICP, VAD, etc.) Assessments & Supporting S&S Interventions Excludes VS,I&O,IV Drips, Device data RESPONSE TO CARE/RECOMMENDATIONS Communication/Event Note(s) Discharge Plan of Care Reviewed DISCHARGE READINESS Discharge Problems Needing Follow-up Goals ASSESSMENT/PROBLEMS Care Contacts EDUCATION & ENGAGEMENT + = includes some respiratory therapy data Other Documentation: (4) Admin Hx (StarForm), (5) Vascular Access (graph), (6) Wounds/Drains/Tubes (graph) use the current StarPanel Views. These 6 views represent all of HED documentation and key Starforms. Updated: 3/19/2016 10:31 PM by Ariosto Nursing Documentation Re-Design You can customize to show only the fields that are important to your view, or capture all that is documented 1. Nursing Data+ Trendable Data: All Vital signs (non-invasive, invasive) Pain# and Scale Height, Length, Weight Risk Section: Total Score/Status: Braden, Fall, PEWS, GCS, etc.. I&O, IV Drips Device data (Vents, ICP, VAD, etc.) 2. Nursing Care Assessments & Supporting S&S Interventions Excludes VS,I&O,IV Drips, Device data 3. Nursing Plan RESPONSE TO CARE/RECOMMENDATIONS, Communication/Event Note(s) DISCHARGE READINESS & Discharge Problems Needing Follow-up ASSESSMENT/PROBLEMS & Goals EDUCATION & ENGAGEMENT + Care Contacts Updated: 3/19/2016 10:31 PM by Ariosto Nursing Documentation Re-Design Exhibit B - Care Plan changes in OPC, Team Summary, and Integrated Presence CURRENT CARE PLAN VIEW in OPC, Team Summary, Integrated Presence NEW CARE PLAN No Pathway and Phase Nursing Plan (last 24hr HED) Response to Care/Recommendations (date/time): Replaces Nursing Summary, Plan Priorities, Goal Status (see below) Communication/Event Note(s) (date/time): All significant communications or events narrated here Goals: (date/time) Replaces short term goals Priority Problems: Vent wean impairment; Restraint injury risk Other Problems: DISCHARGE READINESS: Resource Constraints, Knowledge deficit, Non-Adherent….. Discharge problems needing follow-up: Unable to afford meds (Joe Smith, MSW is working on this) Updated: 3/19/2016 10:31 PM by Ariosto Nursing Documentation Re-Design Exhibit C - WNL DEFINITIONS FAQ – What is our standards of care for assessments and WNL documentation? ADM/BASELINE HISTORY + Pain Pain screen Neuro Hx Neurologic condition or procedure & meds Mental status hx -Sensory Assessment: Baseline visual & auditory function Cardiac Hx Cardiac condition procedure or devices Vascular/Perfusion Hx peripheral vascular disease, edema or pulselessness in extremity Respiratory Hx respiratory condition Screen: Flu, Sleep apnea Home resp devices (CPAP, vent, trach) Gastrointestinal Hx GI condition or procedure Bowel routine Urinary/Renal Hx Urinary/Renal condition or procedure; Bladder routine Reproductive Hx Pregnancy, LMP; Lactation, Pregnscreen Skin Hx of skin conditions Presence of pressure ulcer on admission Activity/Musculoskeletal Hx Musculoskeletal conditions or procedures Need for patient assistive devices and transfer assistive devices STANDARD ASSESSMENT ALL PTS EVERY SHIFT Assessment Pain using age/situation appropriate assessment Assessment Mental status, level of consciousness, basic motor function Speech Assessment BP, Heart rate, rhythm, heart sounds Assessment Capillary refill, edema, peripheral pulses Assessment Breathing pattern & effort, breathsounds, airway status, presence & character of secretions Assessment Abdominal appearance, bowel sounds, bowel movement Assessment Adequate urinary output & character. Assessment Assessment Skin color, appearance, condition and pressure ulcer risk screen. I Assessment Activity level, mobility, positioning DOCUMENT ASSESSMENT WNL IF: No WNL defined – use pain scale =WNL if = Alert & Calm, Oriented x4 (person, place, time, situation); Developmentally appropriate speech; No gross motor deficits =WNL if = BP within expected range for age; Expected heart rate for age; Regular rhythm; No abnormal hearts sounds =WNL if = Extremities warm with absence of pallor and cyanosis Equal palpable peripheral pulses (2-3+); Capillary refill time less than 2 to 3 seconds; Absence of edema =WNL if = Expected rate and depth of breathing for age Absence of dyspnea; Clear, no adventitious breath sounds Oximetry results within baseline range; Arterial blood gas values within baseline range ; Minimal cough; Minimal clear secretions; Patent airway; =WNL if = Bowel movements within own usual pattern and consistency without difficulty; Normal bowel sounds present in all quadrants; Abdomen soft, non-distended, non-tender =WNL if = Urinary Continence – age appropriate; Voids without difficulty and at normal intervals; Adequate urinary output No distention; Clear straw to amber colored urine =WNL if tbd =WNL if = Healthy oral mucous membrane ; Absence of pallor or cyanosis; Absence of redness and irritation (incl IV site checks); No skin breakdown; Braden PU risk score >16 =WNL if = No or minimal mobility limitations (not on bedrest/chairfast restrictions); Uses usual assistive devices safely (WEL). No c/o severe fatigue, generalized weakness or sleep deprivation Updated: 3/19/2016 10:31 PM by Ariosto Nursing Documentation Re-Design Nutrition Hx Nutritional conditions Weight Hx Devices (dentures,) Lactation Fluid & Electrolytes Hx of fluid or electrolyte imbalance Safety/Falls Hx of Behavioral Health problems, Hx of substance use/abuse (tobacco, alcohol, drugs),Hx of injury or falls, Abuse screen, Hx of violence to self / others Medications Medication list Self-Care/ADL ADL Infection/Metabolic Hx thermoregulatory, Immune or Endocrine disorders. Allergy Hx – drug , food, environment Psycho-Social Hx Behavioral health condition. Hx of nonadherence to prescribed medical regimen; use of community services Cultural considerations. Advance directives, Assessment Nutritional appearance, diet, general food intake pattern & diet tolerance =WNL if Excellent or Adequate Nutrition (Braden); Not NPO; Weight does not require intervention such as- nutritional restriction or supplementals; Normal BUN and serum albumin. Assessment =WNL if Electrolytes within normal range Balanced I&O Assessment Evaluate risk for injury from environment, equipment, and patient condition =WNL if Low fall risk score (Morse) No signs of tobacco, alcohol, or illicit drug use No aggressive or self-injurious or impulsive behavior Assessment Evaluate medication indications, patient response and risks Assessment Participation/ability for selfcare Assessment Basic vital signs glucose levels =WNL if No high risk meds, chemo, or radiation (per policy) No more than 6 scheduled meds Assessment Evaluate patient and support systems, mood, behavior, coping, adherence to plan, engagement and ability to participate in care as age and developmentally appropriate. =WNL if Participating in plan of care as prescribed Appears to be coping with condition and care No evidence of dysfunctional family and support systems No behavioral health concerns affecting plan of care. =WNL if Is willing and able to participate in self-care activities such as feeding, grooming, hygiene and toileting. =WNL if No S&S of Infection ; Normothermic No glucose, endocrine, or immunologic disorder Updated: 3/19/2016 10:31 PM by Ariosto