sustained-released beta
advertisement

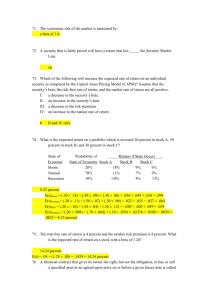
BETA BLOKERS Tintinalli's Emergency Medicine 2010 BY DR. TAYEBEH SALEHI Epidemiology common medications used in the treatment of various cardiovascular, neurologic, endocrine, ophthalmologic, and psychiatric disorders accidental and intentional toxicity is common ` The beta -blockers by decreasing calcium entry into the cell modulate the activity of myocyte and vascular smooth muscle contraction excessive beta -blockade may lead to profound pump failure, with bradycardia, decreased contractility, and hypotension. selectivity is often lost following large overdoses. Sotalol is unique among beta-blockers in its ability to block potassium channels Sotalol is class III antiarrhythmic drugs. Under normal conditions, the heart uses free fatty acids as its primary energy source, but during times of stress, it switches to using carbohydrates to maintain metabolism Inhibition of glycogenolysis and gluconeogenesis reduces the availability of carbohydrates for use by cells hypoglycemia occurs as a consequence of beta -blocker toxicity, it is actually very rare. In the presence of adequate glucose stores, euglycemia and hyperglycemia are more common than hypoglycemia. Clinical Presentation Absorption of regular-release beta -blockers occurs rapidly, often with peak effects within 1 to 4 hours sustained-release cardiac drugs, it is assumed that symptoms may be delayed >6 hours after ingestion Coingestants that alter gut function, such as opioids and anticholinergics, may affect absorption of beta -blockers and subsequent onset of symptoms. The primary organ system affected by beta-blocker toxicity is the cardiovascular system, and the hallmark of severe toxicity is bradycardia and shock. The beta -blockers with sodium channel antagonism can cause a wide-complex bradycardia, and may contribute to development of seizures (especially when the QRS interval is >100 milliseconds). sotalol ability to block potassium channels and prolong the QT interval sotalol is more often associated with ventricular dysrhythmias, includin : premature ventricular contractions bigeminy ventricular tachycardia ventricular fibrillation torsades de pointes Neurologic manifestations include depressed mental status, coma, and seizures. More lipophilic beta-blockers, such as propranolol, cause greater neurologic toxicity than the less lipophilic agents. Seizures can occur but are generally brief, and status epilepticus is rare. Diagnosis including patient history, physical examination findings, and results of basic diagnostic testing. exposures to other drugs and toxins can present with bradycardia and hypotension The 12-lead ECG and Bedside echocardiography are useful to evaluate myocardial performance in cases of undifferentiated shock. Invasive monitoring with central venous or pulmonary artery catheters may be necessary to help direct resuscitation. renal function, glucose level, oxygenation, and acid-base status Treatment General Management should be evaluated in a critical-care area of the ED with appropriate monitoring protect air way GI Decontamination ingestion of a significant quantity of beta -blockers decontamination should be considered. Activated charcoal may be of benefit if it can be given within 1 to 2 hours after ingestion. Multiple dose of activated charcoal therapy following ingestion of sustained-release - Use of ipecac syrup is not recommended Gastric lavage is not routinely used, but may be considered for life-threatening ingestions when the airway is adequately protected from aspiration. Whole-bowel irrigation may be beneficial after ingestion of a sustained-release product, If whole-bowel irrigation is used, adequate airway protection and normal GI function are important. Pharmacologic Treatment Glucagon Glucagon is a first-line agent in the treatment of acute beta – blocker induced bradycardia and hypotension. Effects from an IV bolus of glucagon are seen within 1 to 2 minutes, reach a peak in 5 to 7 minutes duration of action of 10 to 15 minutes. Due to the short duration of effect, a continuous infusion is often necessary after bolus administration. The bolus dose of glucagon is 0.05 to 0.15 milligram/kg (3 to 10 milligrams for the average 70-kg ( and can be repeated as needed. If a beneficial effect is seen from bolus, a continuous infusion 1 to 10 milligrams/h the positive inotropic and chronotropic effects of glucagon may not be maintained for a prolonged period due to possible tachyphylaxis. side effects of high-dose glucagon therapy : Nausea and vomiting esophageal sphincter relaxation Intubation prior to glucagon administration may be warranted in any patient with altered mental status to limit the risk of aspiration. Adrenergic Receptor Agonists The beta -adrenergic receptor agonists—such as norepinephrine, dopamine, epinephrine, and isoproterenol The most effective adrenergic receptor agonist may be norepinephrine due to its ability to increase heart rate and blood pressure. Hyperinsulinemia-Euglycemia Therapy insulin facilitates myocardial utilization of glucose, the desired substrate during stress This is in contrast to glucagon, epinephrine, and calcium, which promote free fatty acid utilization The initial dose is regular insulin 1 unit/kg IV bolus followed by 0.5 to 1.0 unit/kg/h continuous infusion. adverse effects from hyperinsulinemia-euglycemia therapy are hypoglycemia and hypokalemia 0.5 gram/kg bolus of glucose should accompany the initial insulin bolus in a patient whose serum glucose level is <400 milligrams/dL. Serum glucose levels should be monitored regularly: every 20 to 30 minutes until stable euglycemia is achieved, and then every 1 to 2 hours thereafter. Serum potassium levels may fall during hyperinsulinemia-euglycemia therapy. Serum potassium level should be monitored, replacement is not required unless it falls to <2.5 mEq/L (<2.5 mmol/L) or the patient has other sources of true potassium loss Atropine a muscarinic blocker, is unlikely to be effective in the management of beta blocker–induced bradycardia and hypotension, although its use is unlikely to cause harm. Calcium calcium administration is not routinely recommended in beta -blocker overdose, it may be worth considering in patients with refractory shock unresponsive to other therapies. Calcium for IV administration is available in two forms, gluconate and chloride, both in a 10% solution. Calcium chloride solution contains three times more elemental calcium than calcium gluconate solution 10% calcium gluconate 0.6 mL/kg given over 5 to 10 minutes followed by a continuous infusion of 0.6 to 1.5 mL/kg/h 10% calcium chloride 0.2 mL/kg given via central line over 5 to 10 minutes followed by a continuous infusion of 0.2 to 0.5 mL/kg/h. Ionized calcium levels should be checked every 30 minutes initially and then every 2 hours to achieve an ionized calcium level of twice the normal value. Phosphodiesterase Inhibitors such as inamrinone (formerly known as amrinone), milrinone, and enoximone These agents inhibit the breakdown of cAMP thereby maintaining intracellular calcium levels In animal models, phosphodiesterase inhibitors produce positive inotropic effects without increasing myocardial oxygen demand, but have no appreciable effect on heart rate. In the setting of a beta -blocker overdose, phosphodiesterase inhibitors are administrated as a continuous IV infusion, starting at 5 micrograms/kg/min for inamrinone 0.5 microgram/kg/min for milrinone 0.75 microgram/kg/min for enoximone Sodium Bicarbonate In a patient demonstrating a QRS interval longer than 120 to 140 milliseconds, it is reasonable to administer sodium bicarbonate The suggested dose is a rapid bolus of 2 to 3 mEq/kg, Thus, a 70-kg adult receives a bolus of 140 to 210 mEq of sodium bicarbonate, or three to four ampules (50 mL each) of 8.4% sodium bicarbonate Repeat boluses may be required to maintain the QRS interval at <120 milliseconds. Cardiac Pacing Electrical capture and restoration of blood pressure is not always successful Cardiac pacing may be most beneficial in treating torsades de pointes associated with sotalol toxaicity. Extracorporeal Elimination (Hemodialysis) acebutolol atenolol nadolol sotalol their lower protein binding, water solubility, and lower volume of distribution Extracorporeal Circulation extreme of resuscitation, intra-aortic balloon pumps have been successful when pharmacologic measures have failed to reverse cardiogenic shock Treatment of Sotalol Toxicity Inhibition of K channel and prolang QT magnesium supplementation lidocaine cardiac overdrive pacing The goal of resuscitation is to improve hemodynamics and organ perfusion cardiac ejection fraction of 50%, reduction of the QRS interval to <120 milliseconds, heart rate of >60 beats/min, systolic blood pressure of >90 mm Hg in an adult urine output of 1 to 2 mL/kg/h improved mentation Disposition and Follow-Up Patients with altered mental status, bradycardia, conduction delays, or hypotension are often managed in an intensive care unit. any patient who ingests a sustained-released beta -blocker product warrants admission and monitoring for the development of delayed toxicity Patients ingesting an overdose of regular beta -blocker tablets who remain asymptomatic and have normal vital signs for 6 hours after ingestion safe for discharge THANKS FOR YOUR ATTENTION