The Respiratory Syst..
advertisement

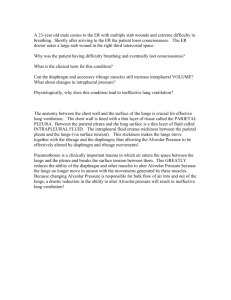
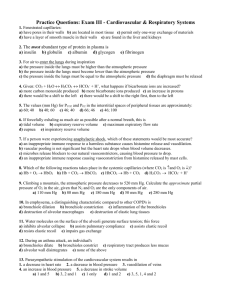
THE RESPIRATORY SYSTEM FUNCTIONS Exchange of gases (O2 & CO2) between environment and tissues. It plays a role in the regulation of pH of the extracellular fluid. MECHANICS OF BREATHING Anatomical consideration: The lungs Thoracic cage (muscles, ribs and vertebrae) Diaphragm Pleural space (visceral and parietal pleurae) Chest movement: External intercostal muscle ( anteroposterior diameter) Internal intercostal muscle ( anteroposterior diameter) Diaphragm ( vertical diameter) Inspiration: Active process volume of thoracic cavity lower the intrapleural pressure The lungs expand lowers the intra-alveolar pressure draw air into the lungs Quiet breathing: 1/10th of inspiratory muscles are active Deep breathing: increased in pulmonary ventilation 10 folds (60L/min) Expiration: Passive Relaxation of muscles of inspiration Recoil of chest wall rises of intrapleural pressure Elastic recoil of the lungs rises of intra-alveolar pressure forced air out of the lungs Accessory muscles of respiration: Accessory muscle of inspiration: sternocleidomastoid, anterior serrati and the scaleni Accessory muscle of expiration: the internal intercostal muscles and abdominal recti. Intrapleural pressure: Negative pressure vary between -2mmHg at the end of expiration to –6mmHg during inspiration. CAUSES OF THE NEGATIVE INTRAPLEURAL PRESSURE 1. The lungs Elastic recoil of the lungs tends to collapse in an inward direction The surface tension of the fluid lining the alveoli Surfactant normally reduced this surface tension It’s a lipoprotein substance secreted by type II alveolar epithelium Decrease surfactant in the newborn causes hyaline membrane disease of the newborn or (respiratory distress syndrome) 2. The chest wall Tends to recoil outward At equilibrium, there are two opposing forces lead to a negative pressure in the pleural cavity 3. Pleural capillaries and lymphatics The intrapleural space is rich in blood capillaries and lymphatics, which tend to absorb fluid from the pleural cavity adds to the negativity of intrapleural pressure Intra-alveolar (intrapulmonary) pressure Pressure within the alveoli of the lungs varies with different stages of respiratory cycle During inspiration: quiet inspiration, the pressure falls to –1mmHg but with forcible inspiration it falls to about –70mmHg During expiration: in quiet expiration, it rises to 1mmHg but during forcible expiration it rises to 100mmHg (Valsalva manoeuver) LUNG VOLUMES AND CAPACITIES Tidal volume: Is the volume of air inspired or expired at each breath. 500mL in normal quiet breathing (0.5L). Respiratory minute volume or (pulmonary ventilation): Is the volume of air breathed in or out of the lungs each minute. 500 (tidal volume) x 12 (respiratory rate) = 6000mL/min. Inspiratory reserve volume: Inspiratory capacity: The volume of air inspired by a maximal inspiratory effort after normal inspiration (3.3L). The volume of air inspired by a maximal inspiratory effort after normal expiration. Equal to the tidal volume plus the inspiratory reserve volume (3.8L). Expiratory reserve volume: The volume of air expired by a maximal expiratory effort after normal expiration (1L). Vital capacity: Residual volume: The volume expired by a maximal expiratory effort after maximal inspiration. Equal to the tidal volume plus inspiratory reserve volume plus expiratory reserve volume (4.8L). The volume of air that remains in the lung after maximal expiration. Cannot be measured by spirometer or gas meter. Increased by age and lung disease (1.2L). Functional residual capacity (FRC): The volume of air that remains in the lung after normal expiration. Cannot be measured by spirometer (2.2L). Total lung capacity: The maximal volume of air that can be accommodated in the lungs. Equal to tidal volume plus inspiratory reserve volume plus expiratory reserve volume plus residual volume (6L). Both residual volume and functional residual capacity by age while vital capacity by age. The lung volumes and capacities are lower in females (20 – 25%) than in the male. DISTRIBUTION OF PULMONARY VENTILATION Definitions Ventilation: is the process dealing with the air movement between the lung and atmospheric air Pulmonary ventilation: is the volume of air breathed in or out per minute Inspired air is distributed to distinct spaces in the lungs Anatomical dead space:Occupies the air-conducting system down to the terminal bronchioles No gas exchange Volume 150ml Respiratory zone:Occupies the space distal to the terminal bronchioles down to the alveolar sacs Gas exchange takes place Volume 350ml/min Gas exchange in the lungs (Diffusion) Exchange of gases (O2 and CO2) between the alveoli and blood FACTORS AFFECTING THE RATE OF DIFFUSION 1. Alveolar capillary membrane (ACM): Semipermeable membrane Separates alveolar air from pulmonary capillary blood Formed of several layers: Fluid film lining the alveoli Alveolar membrane Interstitial fluid Capillary wall Change in the thickness of alveolar capillary membrane will affect the rate of gas diffusion In pulmonary edema thickness of the ACM rate of diffusion During exercise thickness of ACM rate of diffusion 2. Partial pressure gradient of gases across the alveolar capillary membrane: Partial pressure of O2 in mixed venous blood 40mmHg, the P–P of O2 in alveolar air is 100mmHg. So O2 diffuses from the alveolar space to the capillary blood along partial pressure gradient of about 60mmHg P–P of CO2 in venous blood is 46mmHg, while in the alveolar air is 40mmHg, so CO2 diffuses from the capillary to the alveolar space along partial pressure gradient of about 6mmHg 3. Physical properties of gases: Solubility and M-W of gases affect the rate of diffusion CO2 is 20 times more soluble than O2 Diffusion failure affects O2 before CO2 is affected 4. Surface area: As the surface of the alveolar capillary membrane increases, the total volume of gas exchanged will be increased. The surface area of ACM = 70m2 in adult male 5. Ventilation/blood flow ratio: Ventilation/blood flow ratio = alveolar ventilation/ blood flow = 4/5 = 0.8 The bases of the lung perfused more than the apices 6. Temperature: The rate of diffusion of gases is normally dependent on temperature 7. Chemical reactions: Each 1 gram of Hb, when fully saturated, combines with 1.34ml of O2 at STP (at partial pressure of O2 of 100mmHg) O2 dissolved in 100mL of blood at O2 partial pressure of 100mmHg is 0.003 x 100 = 0.3mL 8. Diffusion capacity: CO2 has greater diffusion capacity than O2 about 20 times more (CO2 has greater solubility than O2) TRANSPORT OF OXYGEN O2 is transported in the blood in two forms:Oxyhaemoglobin > 98% 2. Dissolved oxygen < 2% 1. In arterial blood 0.003 x 100 = 0.3mL of O2 In venous blood 0.003 x 40 = 0.12mL of O2 OXYHAEMOGLOBIN Hb has great affinity for O2. It combines loosely, fast and reversibly with O2 It is the function of the P–P of O2 in relation with saturation of Hb with O2 (oxyhaemoglobin dissociation curve) Oxygen-Haemoglobin dissociation curve: The percentage saturation of Hb with O2 against partial pressure of O2 Sigmoid in shape (S-shaped) Hb has 4 haem units attached to polypeptide chains Oxygenation of one haem unit leads to changes in the configuration of the Hb molecule which increase the affinity of the 2nd unit and so on Steep rise in the percentage saturation of Hb between PO2 of 0mmHg and 75mmHg, then slow rise in the curve, becoming more or less flat at PO2 of 80mmHg or above Depends on PO2 and independent on Hb concentration At zero P–P of O2 %saturation is zero At PO2 100mmHg (arterial blood) %saturation 97% At PO2 40mmHg (venous blood) %saturation 75% It is used for measurement of O2 content in venous and arterial blood When 1gm of Hb is fully saturated with O2 it binds up to 1.34mL of O2 If Hb concentration = 150gm/L blood O2 content of arterial blood (97% saturation) = 1.34 x 150 x 97/100 = 195mL/L of blood O2 content of venous blood (75% saturation) = 1.34 x 150 x 75/100 = 150mL/L blood O2 uptake by tissues = arterio-venous difference = 195 – 150 = 45mL/L of blood Factors affecting O2-Hb dissociation curve: Shift to the right indicate lower affinity of Hb for O2 Shift to the left indicate increased affinity of Hb for O2 1. Partial pressure of carbon dioxide: PCO2 affinity of Hb for O2 and shifts the curve to the right (Bohr effect) PCO2 is high in the tissues, while it is lower in the lung 2. pH: pH ( H+ concentration) Hb affinity to O2 and shifts the curve to the right 3. Temperature: Rise of temperature also shifts the curve to the right In active tissues, heat is generated mainly due to oxidation 4. 2,3-diphosphoglycerate (2,3-DPG): 2,3-DPG is found in RBCs bound to Hb 2,3-DPG Hb affinity to O2 and shifts the curve to the right It helps the release of O2 from the tissue ( in hypoxia at high altitude) DISSOLVED OXYGEN Less than 2% It is at equilibrium with the O2 combined with Hb The dissolved O2 transferred to tissues then replaced from O2 carried by Hb It is essential for tissues that don’t have blood supply, like the cornea and cartilage Can be increased by breathing pure or hyperbaric O2 O2 is poorly soluble in blood In 100mL blood at body temperature, 0.003mL O2 dissolved at PO2 1mmHg In arterial blood 0.3mL/100mL O2 is dissolved In venous blood 0.12mL/100mL TRANSPORT OF CO2 CO2 produced by active cells diffuses by concentration gradient into the tissue fluid to reach the plasma CO2 IS TRANSPORTED BY: The plasma (this reaction proceed very slowly due to the absence of carbonic anhydrase enzyme) The red blood cells (this reaction proceed very quickly due to presence of carbonic anhydrase enzyme) In 3 forms: Dissolved 10% (0.4mL) Bicarbonate 70% (2.8mL) Carbamino compounds 20% (0.8mL) CONTROL OF VENTILATION Several mechanisms are involved which can be grouped into two main categories which are closely integrated: Nervous control mechanism Chemical control mechanism THE RESPIRATORY CENTER Composed of several groups of neurons Located in the entire length of the medulla and pons Can be divided into four major groups of neurons:Dorsal respiratory group Ventral respiratory group The apneustic center The pneumotoxic center 1. The dorsal respiratory group – located in the entire length of the dorsal aspect of the medulla. It comprises inspiratory neurons which discharge rhythmically during resting and forced inspiration, so that it is called the rhythmicity center. They are almost responsible for inspiration. 2. The ventral respiratory group – lies ventrolateral to the dorsal respiratory group along the entire length of the medulla. They are inactive during quiet breathing but they are activated during forced breathing as in exercise and they are mainly expiratory neurons with some inspiratory neurons. They are inactive at rest or passive expiration and they become activated when expiration is an active process. 3. The apneustic center – it is situated in the lower pons. It sends excitatory impulses to the dorsal respiratory groups to potentiate the inspiratory drive. It receives inhibitory impulses from the sensory vagal fibers of the Hering-Breuer inflation reflex and inhibitory impulses from the pneumotaxic center. 4. The pneumotaxic center – located in the upper pons. It transmits inhibitory impulses to the apneustic center and to the inspiratory area to switch off inspiration. NERVOUS CONTROL OF VENTILATION The rhythmicity center received impulses from: Higher brain centers Centers in the brain stem (medulla and pons) Special receptors (respiratory reflexes) The rhythmicity center sends excitatory impulses via the intercostal and phrenic nerves to the external intercostal muscles and diaphragm CHEMICAL CONTROL OF VENTILATION The rhythmicity center is affected by chemical changes in the blood via two types of chemoreceptors: Peripheral chemoreceptors Central chemoreceptors PERIPHERAL CHEMORECEPTORS Located mainly in the carotid and aortic bodies, but may be found anywhere in the circulatory system When stimulated, send excitatory impulses to the rhythmicity center (via glossopharyngeal and vagus nerves) Highly sensitive to changes in arterial PO2 and to a lesser extent to PCO2 and pH Fall of PO2, rise in PCO2 and fall of pH, stimulate the chemoreceptors to increase ventilation Normal PO2, PCO2 and pH, low grade of tonic activity in the nerves PCO2 and pH causes low tonic activity ventilation In metabolic acidosis pH causes ventilation to wash out CO2 and to bring pH to normal In metabolic alkalosis pH causes ventilation, CO2 retained in the blood to compensate CENTRAL CHEMORECEPTORS Most probably located on the ventrolateral surface of medulla oblongata (which is bathed with cerebrospinal fluid) Highly sensitive to the hydrogen ion concentration of the CSF evoked by arterial PCO2 (CO2 can freely cross the blood-brain barrier into CSF, while BBB is relatively impermeable to H+ and HCO-3 ions)