Surgical Asepsis
advertisement

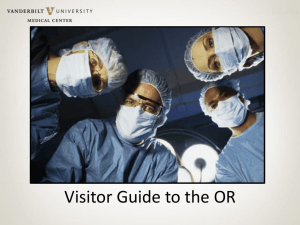
Surgical Asepsis Surgical asepsis differs from medical asepsis. Medical asepsis is defined as any practice that helps reduce the number and spread of microorganisms. Surgical asepsis is defined as the complete removal of microorganisms and their spores from the surface of an object. The practice of surgical asepsis begins with cleaning the object in question using the principles of medical asepsis followed by a sterilization process Which procedures require surgical aseptic technique? • Any medical procedure that involves penetration of the body tissues (invasive procedure) • Major & minor surgeries • Tracheotomy care • Dressing change • Catheterization of the urinary bladder Myelogram (penetration of the body tissue) http://www.youtube.com/watch?v=GhklmY OQ5Es Minor surgery http://www.youtube.com/watch?v=2kM7wK LHTX8&feature=related Tracheostomy care http://www.youtube.com/watch?v=6lKHOtA im28&feature=related Dressing care http://www.youtube.com/watch?v=bBa9HL 4mHa4&feature=related The Environment and Surgical Asepsis • Creating an environment in a surgical suite or special procedure room, to avoid any possible infection to the patient. • Proper attire (scrubs, cap, mask, gloves, shoe covers) • Awareness!!!! Proper Attire OSHA Protocols • Shoes must be comfortable with closed heel and toe and not cloth covered. Cloth-covered shoes may allow blood, body fluids, and other liquids to permeate. Cloth-covered shoes will not protect the feet should a heavy object fall on them. • Personal hygiene must be meticulous. A shower should be taken shortly before beginning a work day in the operating room or special procedure area. • Jewelry, long or artificial fingernails, and nail polish are prohibited. Jewelry harbors microorganisms as do long, polished, or artificial nails. • Any body piercing jewelry must be removed as it may become loose and fall onto the sterile field. • All persons who expect to proceed from the unrestricted zone into the semi-restricted zone must go to the dressing area, don a scrub suit, and tuck the blouse of the suit into the pants or wear a scrub blouse that fits close to the body. • All hair, beards, or mustaches must be covered with a surgical cap and mask. Hair must be confined as it sheds microorganisms with movement • Shoe covers must be placed over shoes to reduce contamination and to protect shoes from coming in contact with blood and body fluids. • Before proceeding into Zone 3, all persons must scrub hands and arms for medical asepsis. It is believed that bare skin may shed microorganisms. In many institutions, all who are not scrubbed for the surgical procedure must wear a scrub jacket to cover bare arms. • Before entering a room where a surgical procedure is in progress, a mask must be donned. The masks worn in the OR must be single, highfiltration masks Zones •Zone 1: An unrestricted zone: persons may enter in street clothing. •Zone 2: A semi-restricted zone: only persons dressed in scrub dress with hair covered and shoes covered may enter. •Zone 3: A restricted zone: only persons wearing scrub dress, shoe covers, and masks are allowed to be present. If a surgical procedure is in progress, the doors to this area are kept closed, and only persons directly involved in the procedure may be present. Those directly involved in the operation are dressed in sterile gowns and sterile gloves. They are often referred to as “being scrubbed.” Most Common Causes of Contamination • • • • The use of contaminated instruments Contaminated gloves Wet or damp sterile field Microorganisms blown onto a surgical site. Special Precautions • Ventilation ducts must have special filters. • Airflow in the OR should be unidirectional. • Air pressure in the OR should be greater than in the outside corridors. • Humidity is to be controlled to prevent static electricity. • OR doors should remain closed as much as possible. The Surgical Team • • • • • • • Surgeon Surgical assistant Nurses Physician assistant (PA) Anesthesiologist Nurse anesthetist Radiologic Technologist Anesthesiologist Surgical assistant Surgical Tech Duties Your duties as a surgical technologist will be to always maintain a clean and sterile environment for the doctors and nurses to perform necessary surgeries properly. You will be in charge of scrubbing in and keeping instruments sterile and organized. You may be asked to assist by handing instruments to the physicians. You will also have to have knowledge of surgical machines, such as laser and suction machines. You will be in charge of prepping a patient before and after surgery. All of this you will learn in the classroom as well as hands on. Surgical technologists play a very important role in the operating room OR Nurse For patients of operative or invasive procedures, the operating room nurse's jobs and duties will consist of education, preparation and coordination of patient care. O.R. or perioperative registered nurses are responsible for maintaining the sterile conditions in the operating room and monitoring patients during the operation. They are also responsible for continued care during and after the procedure X-ray in OR http://www.youtube.com/watch?v=4LUQHq y1ilc http://www.youtube.com/watch?v=HFNGc_ YFmBQ&feature=related Methods of Sterilization and Disinfection • Removal of microorganisms and their spores must be complete, or the article is not sterile. • Disinfection • To remove as many micoorganisms as possible from a surface by physical or chemical means. • Articles or surfaces that cannot be sterilized in the OR or special procedure room must be disinfected. Disinfectant Status Use Alcohols (70% or 90%) (intermediatelevel) bactericidal, tuberculocidal, fungicidal, and virucidal to disinfect thermometers, medication vials, etc. Glutaraldehyde (high-level) broad antimicrobial range, fungicidal and virucidal to disinfect endoscopes, thermometers, and rubber items Chlorine Compounds (dilution of 1:50 is high-level) concentrations of 1000 ppm inactivate bacterial spores to disinfect countertops, floors, other surfaces Orthophthalaldehyde (high-level) bactericidal, virucidal, fungicidal, tuberculocidal in 12 minutes at room temperature to clean and process endoscopes Hydrogen Peroxide (low-level) 6% solutions effective against some bacteria, fungi, and viruses may be used to clean work surfaces, not widely used in health care settings Iodine and Iodophors (intermediatelevel) vegetative bactericidal, M. tuberculosis, most viruses and fungi, no sporicidal capability may be used as disinfectant or antiseptic Phenolics (intermediate- or low-level) most formulations are tuberculocidal, bactericidal, virucidal, and fungicidal have toxic effects, used as environmental not sporicidal disinfectants Quaternary Ammonium Compounds not recommended for high-, intermediate- or low-level disinfection cleaning agents for noncritical surfaces Physical methods of disinfecting are boiling in water and ultraviolet irradiation. Boiling may be used as a means of disinfection if no other method is available; however, many spores are able to resist the heat of boiling (212°F or 100°C) for many hours. To increase the effectiveness of boiling, sodium carbonate may be added to the water in quantity to make a 2% solution. If an object is to be disinfected by boiling and sodium carbonate is added to the water, it should be boiled for 15 minutes. If sodium carbonate is not added, boiling time should be 30 minutes. http://www.youtube.com/watch?v=pZSX_x Ollio&feature=related http://www.youtube.com/watch?v=ySmmXd9CUs Table 5-2 Methods of Sterilization Steam Under Pressure: Item are double-wrapped and placed in an autoclave. Autoclaves are manufactured to sterilize by gravity displacement and dynamic air removal. High-speed sterilizers or flash sterilization is an abbreviated gravity displacement method. Chemical Sterilization: Referred to as low-temperature sterilization. A maximum temperature of 54° C to 60° C of gaseous sterilization is used. An antimicrobial and sporicidal agent must be used. Ethylene Oxide: Used for items that cannot withstand moisture and high temperatures. All items sterilized in this manner must be cleansed and dried since water united with ethylene oxide forms ethylene glycol, which cannot be eliminated by aeration and is toxic. http://www.youtube.com/watch?v=Z9Y9QLj Egks&feature=related If the sterility of an item is questionable, it is not to be considered sterile. •Once a sterile field has been prepared, it must not be left unattended as it may become contaminated and presumed to be sterile. •An unsterile person does not reach across a sterile field. •A sterile person does not lean over an unsterile area. •A sterile field ends at the level of the tabletop or at the waist of the sterile person's gown. •Anything that drops below the tabletop or sterile person's waistline is no longer sterile and may not be brought up to the sterile tabletop. The only parts of the sterile gown considered sterile are the areas from the waist to the shoulders in front and the sleeves from 2 inches above the elbow to the cuffs. •The cuffs of the sterile gown are considered non-sterile because they collect moisture. Cuffs must always be covered by sterile gloves. •The edges of a sterile wrapper are not considered sterile and must not touch a sterile object. •Sterile drapes are placed by a sterile person. The sterile person places the drapes on the area closest to him first to protect his sterile gown. •A sterile person must remain within the sterile area. He must not lean on tables or against the wall. •If one sterile person must pass another, they must pass back-to-back. •The sterile person faces the sterile field and keeps sterile gloves above the waist in front of his chest. The sterile person must avoid touching any area of his body. •Any sterile material or pack that becomes damp or wet is considered unsterile. •Any objects that are wet with disinfectant solution and are to be placed on a sterile field must be placed on a folded sterile towel for the moisture to be absorbed. •A wet area on a sterile field must be covered with several thicknesses of sterile toweling or an impervious drape. •When pouring sterile solution, place the lid face upward and do not touch the inside of the lid or the lip of the flask. Pour off a small amount of solution before the remainder is poured into the sterile container. When a sterile solution is to be poured into a container on a sterile field, the container is placed at the edge of the sterile field by the sterile person Opening sterile pack http://www.youtube.com/watch?v=oBvLnLd WGBE&feature=related Passing sterile object to a sterile person Putting an object in the sterile field Transferring a sterile object Sterile scrub, gowning and gloving http://www.youtube.com/watch?v=AZVbh5i HXlE&feature=related The radiographer is responsible for protecting himself and all persons in the OR and special procedure areas from radiation. He is also expected to be knowledgeable concerning the areas that are sterile. He must protect sterile areas and the patient from contamination in the process of his duties X-ray equipment in OR • Mobile C-arm Ceiling mounted C-arm http://www.youtube.com/watch?v=Jz31Li9 MM_E The radiographer is responsible for making certain that any radiographic equipment used during a sterile procedure is clean and dustfree before use. • Overhead units must be cleaned with a disinfectant solution, and portable radiographic machines and image receptors to be used must be cleaned with a disinfectant solution. • Sterile technique must be maintained for all items and persons involved in the invasive procedure. • If possible, place image receptors and take scout films before draping the patient for the procedure. • If the image receptors must be placed after the procedure is begun, the radiographer may pass the image receptor to the scrub nurse who receives the image receptor in a sterile plastic bag and places it at the radiographer's direction. • If the radiographer places the image receptor himself, the surgical team must make room for him. He may place the image receptor by raising the sterile drapes touching only the inside of the drape, or the circulating nurse may lift the drapes and assist in placing the cassette into the image receptor holder •If multiple images are to be taken, all personnel who are not scrubbed must leave the OR if at all possible. The scrubbed members of the team must wear protective radiation apparel. They may also step behind protective lead-lined screens. •When hands are directly exposed to radiation, leaded sterile gloves as well as all other protective equipment must be worn. •Pregnant female personnel should not be present in the OR when radiographic imaging is in progress. •The radiographer must wear his radiation detection badge on the outside of the lead apron and under the sterile gown during imaging procedures. The badge must be checked at prescribed intervals. •During imaging, all unnecessary instruments must be removed from the operative field and a sterile drape must be placed over the open incision Skin Preparation for Sterile Procedures • Skin prep – the purpose of a skin prep is to remove as many microorganisms as possible by mechanical and chemical means to reduce the potential of infection. • There are two aspects to skin preparation for a sterile procedure: • Mechanical • Chemical Chemical Method of Skin Preparation • The area to be penetrated should be cleaned with an antiseptic solution. • Once you start to clean the area of interest, do this in a circular motion beginning in the center and working outward. • Do not cross anything over the area that has been prepped. • Sterile technique is maintained during the skin prep for sterile procedures! Draping for Sterile Procedure • After the skin has been prepared, place sterile drapes around the area of interest. • Must be handled as little as possible • They must not be flipped or fanned • Disposable sterile cloth towel are mainly used, however, a fenestrated drape may be used. • Place them so that they are within the limits of the area prepared • They are folded so that they overlap and the folds face the operative site. http://www.youtube.com/watch?v=WUbqry DgQ40&feature=fvw Removing and Reapplying Dressings • You must not remove or reapply dressing without a physicians order. • All dressings must be treated as if they are contaminated, because drainage from wounds may harbor pathogenic microorganisms. http://www.youtube.com/watch?v=pJebrgG UYSQ&feature=related