The Respiratory System
advertisement

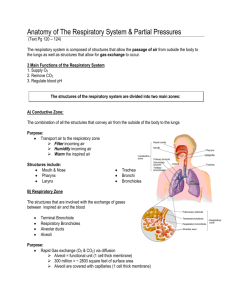
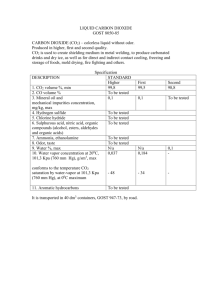
Ch. 13 The Respiratory System Copyright (c) The McGraw-Hill Companies, Inc. Permission required for reproduction or display Breath of Fresh Air • Know what is meant by ventilation and where gas exchange occurs in the lungs • Know the respiratory centers of the brain and how the control respiration • Know the various lung volumes and lung capacities • Know how gas exchange is accomplished and the factors that can affect the rate of gas exchange Respiratory System • What are some functions of the respiratory system? • Respiration as a process – Ventilation – External and internal respiration – Cellular respiration Anatomy • Principal organs – Nose, pharynx, larynx, trachea, bronchi, and lungs • Conducting division – Function only in airflow • Respiratory division – Function in gas exchange Organs of Respiratory System Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Nasal cavity Posterior nasal aperture Hard palate Soft palate Epiglottis Nostril Pharynx Larynx Esophagus Trachea Left lung Right lung Left main bronchus Lobar bronchus Segmental bronchus Pleural cavity Pleura (cut) Diaphragm Figure 22.1 Lungs • Right lung – Three lobes divided by horizontal and oblique fissures • Left lung – Two lobes divided by oblique fissure Copyright © The McGraw-Hill Companies • Pleurae – Visceral – Parietal – Pleural cavity • Pleural fluid (b) Mediastinal surface, right lung Alveoli • ~ 150 million sacs for gas exchange – Why so many? • Cells types – Squamous alveolar cells (type I) • 95% of surface, thinness allows rapid gas exchange – Great alveolar cells (type II) • Repair alveolar epithelium • Secrete surfactant – Alveolar macrophages (dust cells) • Phagocytize dust particles, bacteria, debris • Respiratory membrane Copyright © The McGraw-Hill Companies Ventilation • Respiratory cycle – Inspiration – Expiration • Respiratory muscles – Diaphragm – Intercostals – Accessory muscles of respiration • Sternocleidomastoids, scalenes, pectoralis muscles, serratus anterior, erector spinae Respiratory Muscles Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Inspiration Sternocleidomastoid (elevates sternum) Scalenes (fix or elevate ribs 1–2) External intercostals (elevate ribs 2–12, widen thoracic cavity) Pectoralis minor (cut) (elevates ribs 3–5) Forced expiration Internal intercostals, interosseous part (depress ribs 1–11, narrow thoracic cavity) Internal intercostals, intercartilaginous part (aid in elevating ribs) Diaphragm (ascends and reduces depth of thoracic cavity) Diaphragm (descends and increases depth of thoracic cavity) Rectus abdominis (depresses lower ribs, pushes diaphragm upward by compressing abdominal organs) External abdominal oblique (same effects as rectus abdominis) Figure 22.13 Neural Control of Breathing • Conscious and sub-conscious control • Three pairs of respiratory centers in reticular formation of medulla and pons – Ventral respiratory group (VRG) • Inspiratory (I) neurons • Expiratory (E) neurons – Dorsal respiratory group (DRG) • External influence of VRG • Integrating center – Central and peripheral chemoreceptors, stretch receptors, irritant receptors – Pontine respiratory group • Integrates input from higher brain centers • Influences VRG and DRG • Modifies breathing to sleep, emotional responses, exercise, other special circumstances Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Key Inputs to respiratory centers of medulla Outputs to spinal centers and respiratory muscles Output from hypothalamus, limbic system, and higher brain centers Respiratory Control Centers Pons Pontine respiratory group (PRG) Dorsal respiratory group (DRG) Central chemoreceptors Glossopharyngeal n. Ventral respiratory group (VRG) Vagus n. Medulla oblongata Intercostal nn. Spinal integrating centers Phrenic n. Diaphragm and intercostal muscles Figure 22.14 Accessory muscles of respiration Taking a Breath • Inspiration – Boyle’s law • Pressure of a gas inversely proportional to its volume at constant temp. – Charles’s law • Volume of a gas directly proportional to its temperature at constant pressure • Expiration – Passive process, elastic recoil of thoracic cage • Resistance to airflow – Diameter of bronchioles – Pulmonary compliance – Surface tension of alveoli Measurements of Ventilation • Spirometer • Dead space – Approx. 150 ml of air remain in conductive division – Alveolar ventilation rate (AVR) – volume of air used in gas exchange X breaths/min • Tidal volume (TV) – one cycle of quite breathing, about 500 ml • Inspiratory reserve volume (IRV) – amount that can be inhaled beyond TV inhalation, 3000 ml • Expiratory reserve volume (ERV) – amount that can be forcefully exhaled beyond TV exhalation, 1200 ml • Residual volume (RV) – volume of air that remains even after maximal expiration, 1300 ml Lung Volumes and Capacities Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. 6,000 Maximum possible inspiration 5,000 Lung volume (mL) 4,000 Inspiratory reserve volume Vital capacity Inspiratory capacity Tidal volume 3,000 Total lung capacity Expiratory reserve volume 2,000 1,000 0 Maximum voluntary expiration Residual volume Functional residual capacity Spirometry • Restrictive disorders – Reduce pulmonary compliance – Appear as a reduced vital capacity • Obstructive disorders – Blockage or narrowing of airway – More difficult to inhale/exhale given amount of air – Measure by forced expiratory volume (FEV) • Percentage of vital capacity that can be exhaled in a given time interval – 75-85% in 1 second for healthy adult Gas Exchange • Involves oxygen and carbon dioxide • Composition of air – 78.6% N2, 20.9% O2, .04% CO2, 0.5% H2O • Dalton’s law – total atmospheric pressure is sum of partial pressures of individual gases • Composition of gases will vary depending on where air is in the respiratory tract – Inhaled air differs from alveolar air differs from exhaled air Driving Force Behind Alveolar Exchange • Diffusion down concentration gradient – Have to consider that we are going from air to water • Henry’s law – for a given temperature, at the air-water interface the amount of gas that dissolves in the water is determined by its solubility in water and its partial pressure in air • Erythrocytes load O2 and unload CO2 • Efficiency of exchange may be affected by: – Pressure gradients, solubility, membrane thickness and area, ventilation-perfusion coupling Gas Transport • Oxygen binds to hemoglobin (98.5%) – Oxyhemoglobin (HbO2) • Carbon dioxide – Carbonic acid (90%) – Carbamino compounds (carbaminohemoglobin, HbCO2) – Dissolved gases Systemic Gas Exchange • Systemic gas exchange - the unloading of O2 and loading of CO2 at the systemic capillaries • CO2 loading – CO2 diffuses into the blood – carbonic anhydrase in RBC catalyzes • CO2 + H2O H2CO3 HCO3- + H+ – chloride shift • keeps reaction proceeding, exchanges HCO3- for Cl• H+ binds to hemoglobin • O2 unloading – H+ binding to HbO2 reduces its affinity for O2 • tends to make hemoglobin release oxygen • HbO2 arrives at systemic capillaries 97% saturated, leaves 75% saturated – – venous reserve – oxygen remaining in the blood after it passes through the capillary beds – Utilization coefficient – given up 22% of its oxygen load Systemic Gas Exchange Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Respiring tissue Capillary blood 7% Dissolved CO2 gas CO2 CO2 + plasma protein Carbamino compounds 23% CO2 HbCO2 CO2 + Hb 70% CO2 CO2 + H2O CAH H2CO3 Chloride shift Cl– HCO3– + H+ 98.5% O2 1.5% O2 HbO2+ H+ O2 + HHb Dissolved O2 gas Figure 22.24 Key Hb Hemoglobin HbCO2 HbO2 HHb CAH Carbaminohemoglobin Oxyhemoglobin Deoxyhemoglobin Carbonic anhydrase Alveolar Gas Exchange • Reactions that occur in the lungs are reverse of systemic gas exchange • CO2 unloading – As Hb loads O2 its affinity for H+ decreases, H+ dissociates from Hb and bind with HCO3• CO2 + H2O H2CO3 HCO3- + H+ – Reverse chloride shift • HCO3- diffuses back into RBC in exchange for Cl-, free CO2 generated diffuses into alveolus to be exhaled Alveolar Gas Exchange Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Alveolar air Respiratory membrane Capillary blood 7% CO2 Dissolved CO2 gas Carbamino compounds CO2 + plasma protein 23% CO2 70% CO2 CO2 + H2O CAH Chloride shift Cl- HbCO2 CO2 + Hb H2 CO3 HCO3- + H+ 98.5% O2 O2 + HHb HbO2 + H+ 1.5% O2 Dissolved O2 gas Key Hb Figure 22.25 HbCO2 HbO2 HHb CAH Hemoglobin Carbaminohemoglobin Oxyhemoglobin Deoxyhemoglobin Carbonic anhydrase Concentration Gradients of Gases Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Expired air Inspired air PO2 116 mm Hg PCO2 32 mm Hg PO2 159 mm Hg PCO2 0.3 mm Hg Alveolar gas exchange Alveolar air O2 loading PO2 104 mm Hg CO2 unloading PCO2 40 mm Hg CO2 Gas transport O2 Pulmonary circuit O2 carried from alveoli to systemic tissues CO2 carried from systemic tissues to alveoli Deoxygenated blood Oxygenated blood PO2 95 mm Hg PCO2 40 mm Hg PO2 40 mm Hg PCO2 46 mm Hg Systemic circuit Systemic gas exchange CO2 O2 O2 unloading CO2 loading Tissue fluid PO2 40 mm Hg PCO2 46 mm Hg Figure 22.19 Adjustment to the Metabolic Needs of Individual Tissues • Hemoglobin unloads O2 to match metabolic needs of different states of activity of the tissues • Four factors that adjust the rate of oxygen unloading – ambient PO2 • active tissue has PO2 ; O2 is released from Hb – temperature • active tissue has temp; promotes O2 unloading – Bohr effect • active tissue has CO2, which lowers pH of blood ; promoting O2 unloading – bisphosphoglycerate (BPG) • RBCs produce BPG which binds to Hb; O2 is unloaded • Haldane effect – rate of CO2 loading is also adjusted to varying needs of the tissues, low level of oxyhemoglobin enables the blood to transport more CO2 • body temp (fever), thyroxine, growth hormone, testosterone, and epinephrine all raise BPG and cause O2 unloading • metabolic rate requires oxygen Blood Gases and the Respiratory Rhythm • Rate and depth of breathing adjust to maintain levels of: – pH 7.35 – 7.45 – PCO2 40 mm Hg – PO2 95 mm Hg • Brainstem respiratory centers receive input from central and peripheral chemoreceptors that monitor the composition of blood and CSF • Most potent stimulus for breathing is pH, followed by CO2, and least significant is O2 Hydrogen Ions • Acidosis – blood pH lower than 7.35 • Alkalosis – blood pH higher than 7.45 • Hypocapnia – PCO2 less than 37 mm Hg (normal 37 – 43 mm Hg) • most common cause of alkalosis • Hypercapnia – PCO2 greater than 43 mm Hg • most common cause of acidosis Effects of Hydrogen Ions • Respiratory acidosis and respiratory alkalosis – pH imbalances resulting from a mismatch between the rate of pulmonary ventilation and the rate of CO2 production • Hyperventilation is a corrective homeostatic response to acidosis – “blowing off ” CO2 faster than the body produces it – pushes reaction to the left CO2 (expired) + H2O H2CO3 HCO3- + H+ – reduces H+ (reduces acid) raises blood pH towards normal • Hypoventilation is a corrective homeostatic response to alkalosis – – – – allows CO2 to accumulate in the body fluids faster than we exhale it shifts reaction to the right CO2 + H2O H2CO3 HCO3- + H+ raising the H+ concentration, lowering pH to normal Effects of Oxygen • PO2 usually has little effect on respiration • Chronic hypoxemia, PO2 less than 60 mm Hg, can significantly stimulate ventilation – Hypoxic drive – respiration driven more by low PO2 than by CO2 or pH – Emphysema, pneumonia – High elevations after several days Respiration and Exercise • Causes of increased respiration during exercise 1. When the brain sends motor commands to the muscles • Also sends this information to the respiratory centers • Increase pulmonary ventilation in anticipation of the needs of the exercising muscles 2. Exercise stimulates proprioceptors of the muscles and joints • Transmit excitatory signals to the brainstem respiratory centers • Increase breathing because they are informed that the muscles have been told to move or are actually moving • Increase in pulmonary ventilation keeps blood gas values at their normal levels in spite of the elevated O2 consumption and CO2 generation by the muscles Effect of Smoking Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Tumors (a) Healthy lung, mediastinal surface (b) Smoker's lung with carcinoma a: © The McGraw-Hill Companies/Dennis Strete, photographer; b: Biophoto Associates/Photo Researchers, Inc. Figure 22.27 a-b