2. What diagnoses can we make from an ECG?
advertisement

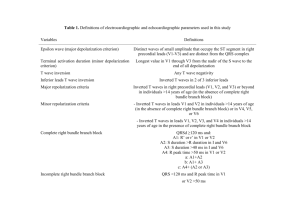
Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php 1. What does ECG stand for? Electrocardiogram 2. What diagnoses can we make from an ECG? Cardiac: 1. MI 2. Pericarditis 3. AF 4. Heart block 5. ?PE Non-cardiac: 1. Digoxin toxicity 2. Hyperkalaemia 3. Hypokalamiea 4. Hypercalcaemia 5. Hypocalcaemia 3. How many electrical leads do you need to record an ECG? Need minimum of 3 but standard is a ’12-lead’, which actually uses 10 leads Where on a patient do you attach them? V1 R sternum 4th IC space V2 L sternum 4th IC space V3 between V2 and V4 V4 5th IC space at MCL V5 5th IC space at anterior axillary line V6 level with V4 at mid-axillary line aVr right hand (aV = augmented vector) aVl left hand aVf left foot 1 dead lead right foot Lead 1, 2 and 3 show current moving between electrodes 4. What are the names of the leads on a 12 lead ECG? How can we divide them up? 5. The ECG is a graph. What is represented by the x axis? Time What does a large square represent? 0.2s What about a small square? 0.04s What is represented by the y axis? mV Isoelectric line; Q and S not always seen x 6. In the picture above, what does P represent? Atrial depolarisation Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php What does QRS represent? Ventricular depolarisation How many squares wide can it be? 0.8-0.12s normal (2-3 small squares); widened QRS >0.12s (= 3 small squares) What does T represent? Ventricular repolarisation What is x called? PR interval What does it represent? Atrial impulse through AVN, bundle of His and bundle branches (conduction delay) How long can it be? 0.12-2.0s normal; can be very long if have complete heart block! (3-5 small squares) 7. Draw a schematic representation of the conducting system of the heart. 8. What is the normal heart rate? 60-100bpm Fill in the table below Pg 84 ox handbook Causes of tachycardia >100 Sinus bradycardia: anaemia, anxiety, exercise, pain, fever, sepsis, hypovolaemia, HF, PE, pregnancy, thyrotoxicosis, beri beri, hypoxia = CO2 retention, autonomic retinopathy, sympathomimetics (caffeine, adrenaline, nicotine), CCF AF Atrial flutter Ventricular tachycardia Ventricular fibrillation? Causes of bradycardia <60 Sinus bradycardia: physical fitness, vasovagal attacks, sick sinus syndrome, acute MI (esp inferior), drugs (βblockers, digoxin, amiodarone, verapamil) hypothyroidism, hypothermia, increased ICP, cholestasis Heart block 9. What cardiac dysrhythmias do you know of? Can you add them to the table above? Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php Background info: Looks at the heart in 12 directions. 6 chest/precordial leads (V1-6) and 4 limb leads (I, II, III and aVR, aVL, aVF). Note that the four limb leads give us six directions at looking at the heart. Lead V1: R sternum 4th IC space o Shows P wave, QRS complex, ST segment o Distinguishes between R/L ventricular ectopic beats that Unipolar but originate from myocardial irritation; monitors ventricular biphasic , with arrhythmias, ST segment changes, bundle-branch block +ve and –ve Lead V2: L sternum 4th IC space deflections Lead V3: between V2 and V4 o Monitor ST segment elevation Lead V4: 5th IC space at MCL Lead V5: 5th IC space at anterior axillary line o +ve deflection o changes in ST segment and T wave Lead V6: level with V4 at mid-axillary line o +ve deflection Leads V1-6 provide a view of the horizontal plane of the heart. The opposing pole of these leads is the centre of the heart. Current travelling towards the –ve pole = waveform deflects downwards Current travelling towards a +ve pole = waveform deflects upwards Biphasic (up and down) if current travels perpendicular to the lead Lead I: provides a view of the heart that shows the current moving from R to L; +ve electrode placed on left limb/chest and –ve electrode on right arm o Produces a positive deflection Bipolar leads: o Monitors atrial rhythms and hemiblocks axes form ‘Einthoven’s Lead II: positive electrode on left leg and negative electrode on right arm triangle Arteries involved with o Produces a positive deflection readings from leads o Monitoring sinus node and atrial I aVR V1 V4 arrhythmias and MI II aVL V2 V5 Lead III: positive electrode on left leg and III aVF V3 V6 negative electrode on left arm Inferior o Changes involved with MI Circumflex Leads I-III provide a view of the frontal plane of the heart. Anterior Right ankle = neutral lead The ‘a’ leads: augmented leads aVR: positive electrode placed on right arm o Produces a negative deflection In practice, leads I, II and III are the Unipolar aVL: positive electrode on left arm same leads as aVR, aVL, aVF. (The leads ECG machine does the actual o Produces a positive deflection switching and rearranging of the aVF: positive electrode on left leg electrode designations). o Produces a positive deflection Leads aVR, aVL, aVF provide a view of the frontal plane of the heart. A lead provides a view of the heart between a positive and negative pole (along which current flows) The mean electrical axis for the heart normally lies between A plane refers to the cross-sectional perspective: frontal -30 and +90°. Less than -30° is termed a left axis deviation plane (vertical cut) provides an A-P view of heart activity, and greater than +90° is termed a right axis deviation. Axis whilst horizontal plane (transverse cut) provides either a deviations can be caused by increased cardiac muscle mass (e.g., left ventricular hypertrophy), changes in the sequence superior/inferior view of ventricular activation (e.g., conduction defects), or because of ventricular regions being incapable of being activated (e.g., infarcted tissue). Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php ***10 leads; 1 dead therefore 9 useful leads and we get 12 readings*** 10 small squares vertically = 1 mV. Flat line = no electrical activity A standard ECG is printed at 25mm/s = 25 small squares/s Direction which waves point = elec activity towards/ away from a lead Eg normal travel through the heart is a downward diagonal line from the right shoulder (SAN) to the left lower abdomen (left ventricle = more conduction). Amplitude is due to muscle mass. LHS heart is thicker so needs more elec activity = bigger peaks. Even bigger in hypertrophy! Lead AVR (right shoulder/right arm/wrist) will always see the electrical stimulus travelling away from it = waves in sinus rhythm will all point downwards; V6 will always see activity coming towards it (point up) V1 and V2 lie directly over rt ventricle V3 and V4 lie over the interventricular septum V5 and V6 lie over lt ventricle aVR V1 V4 V II aVL V2 V5 III aVF V3 V6 I I I II Rhythm strip Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php Regions of the Heart each lead refers to: AVL is on the left wrist or shoulder and looks at the upper left side of the heart. Lead l travels towards AVL creating a second high lateral lead. AVf is on the left ankle or left lower abdomen and looks at the bottom, or inferior wall, of the heart. Lead ll travels from AVr towards AVf to become a 2nd inferior lead Lead lll travels from AVL towards AVf to become a 3rd inferior lead. V2 V3 and V4 look at the front of the heart and are the anterior leads. V1 is often ignored but if changes occur in V! and V2 only, these leads are referred to as Septal leads. V5 and V6 look at the left side of the heart and are the lateral leads. The ECG below shows where these leads are when printed. • • • 12 lead connection box Right hand = red lead Left foot = green like grass Left hand = yellow like the sun 5 lead connection box ANTERIOR: – V1-V4 INFERIOR: – II, III, and AVF LEFT LATERAL: – I, AVL, V5 AND V6 Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php ECG Complex: P wave: atrial depolarisation Look at its Location: precedes QRS complex Amplitude: 2-3mm high Duration: 0.06-0.12s Configuration: usually rounded and upright Deflection: +ve/upright o Peaked, notched, enlarged P waves = atrial hypertrophy associated with COPD, pulmonary emboli, valvular disease, heart failure o Inverted P waves = retrograde/reverse conduction o Varying P waves = impulse coming from different sites (irritable atrial tissue; damage near SAN) o Absent P waves = conduction by a route other than SAN (junctional or atrial fibrillation) PR Interval: tracks atrial impulse through AVN, bundle of His and R/L bundle branches: delayed Location: from beginning of P wave to QRS complex Duration: 0.12-0.2s (3-5 small squares) o Altered impulse formation or conduction delay: AV block o Short PR: impulse originated from somewhere else other than SAN: pre-excitation syndromes, junctional arrhythmias o Prolonged PR: conduction delay through atria/AVN due to heart block or digoxin toxicity (ischaemia or conduction tissue disease) QRS complex: ventricular depolarisation (represents intraventricular contraction time); atrial repolarisation is buried in complex Location: follows PR interval Amplitude: 5-30mm Duration: 0.08-0.12s (2-3 small squares; ½ PR interval); measured from beginning of Q wave to end of S wave Configuration: Q (-ve deflection), R (+ve deflection), S (-ve deflection); may not always see waves Deflection: +ve in leads I, II, III, aVL, aVF and V4-6; -ve in aVR and V1-3 o If no P wave, then impulse may have originated in ventricles = ventricular arrhythmia o Deep and wide Q waves (Q amplitude is 25% of R wave, or duration > 0.04s) = MI o Notched R wave = bundle-branch block o Widened QRS complex (>0.12s) = ventricular conduction delay o Missing QRS complex = AV block or ventricular standstill o Note that in older adult ECGs, PR, QRS and QT intervals are often increased, whilst amplitude of QRS is decreased and there’s a shift of the QRS complex to the left Q wave = septal depolarisation and previous MI so not present in 20yo; Whilst the electrical stimulus passes through the bundle of His, and before it separates down the two bundle branches, it starts to depolarise the septum from left to right. This is only a small amount of conduction (hence the Q wave is less than 2 small squares), and it travels in the opposite direction to the main conduction (right to left) so the Q wave points in the opposite direction to the large QRS complex. R wave = electrical stimulus passing through bulk of ventricular walls. Thick walls = more cells = more electricity needed = bigger wave produced Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php S wave = Purkinje fibres depolarisation; travels in the opposite direction to the large R wave because Purkinje fibres spread throughout the ventricles from top to bottom and then back up through the walls of the ventricles. ST segment: end of ventricular conduction/depolarisation and beginning of ventricular recovery/repolarisation The point that marks the end of the QRS complex and beginning of the ST segment = J point Location: extends from S wave to beginning of wave Deflection: usually isoelectric (flat with baseline) o Elevated (1mm above baseline) = MI or pericarditis o Depressed (0.5mm below baseline) = myocardial ischaemia or digoxin toxicity T wave: ventricular repolaristation (specifically repolarisation of AVN and bundle branches) Location: follows S wave Amplitude: 0.5mm in leads I, II, and III, and up to 10mm in precordial leads Configuration: typically round and smooth Deflection: upright in leads I, II, V3-6; inverted in aVR; variable in the rest o T wave may be bumpy because P wave is hidden within it (note that T wave = relative refractory period and cells are extra sensitive to extra stimuli) o Tall, inverted or pointy ‘tented’ = MI or hyperkalaemia o Inverted in leads I, II, V3-6 may = MI o Heavily notched or pointed T waves = pericarditis QT Interval: measures ventricular depolarisation and repolarisation; time varies with HR (faster HR = shorter QT) Location: extends from beginning of QRS complex to end of T wave Duration: varies according to age, sex and HR; usually 0.36-0.44s; should not be greater than half the distance between consecutive R waves when rhythm is regular. o Prolonged QT = relative refractory period is longer = increases the risk of life-threatening arrhythmia known as torsades de points o Class IA antiarrythmics o Congenital conduction defect present in certain families o Short QT = digoxin toxicity of hypercalcaemia U wave: recovery period of the Purkinje or ventricular conduction fibres; not always present Location: follows T wave Configuration: typically upright and rounded Deflection: upright o If prominent, may = hypercalcaemia, hypokalaemia, digoxin toxicity Interference on an ECG: 1. Muscle Tremor Muscle tremor is something that can occur for a number of reasons, such as: Shivering due to cold Rigors Parkinsons disease 2. Electrical Interference Another disturbance emanating directly from the surrounding environment is electrical interference. The ECG machine is designed to pick up electrical activity within the heart but it will pick up electrical activity from nearby machinery, such as: Pumps, TV, Drills, Machinery Correct problems and repeat ECG Comfort of the patient, Turn machines off, Drugs to control symptoms, Warm the patient, Talk to the workmen Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php 3. Artefact Artefact is the name given to disturbances in rhythm monitoring caused by movement of the electrodes.(see below) Correct problems and repeat ECG If the electrodes have been in place for a prolonged period of time, the moist inner pad can dry up and the connection becomes poor. Sometimes the weight of the leads can pull the electrode away from the skin and contact is lost intermittently, such as when the patient leans or roles over. Sometimes the electrode has come away from the skin and is stuck to an item of clothing Sometimes, the patient is fiddling with the electrodes Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php # of small block HR Analysing an ECG: 1. Patient details Name, DOB, NHS number 2. Check ECG details Date taken, any chest pain at the time, patient uncooperative and moving etc CHECK OLD ECG for chronic changes (old MI, known bundle block) 3. Rate: 25 small squares=5 large blocks/second (ie 1 small square = 0.04s); <3 blocks = sinus tachycardia; > 5 blocks = sinus bradycardia (sinus = 60-100) Three ways: 10x method: especially if rhythm is irregular. ECG paper is marked in increments of 3 seconds (15 large boxes); obtain a 6 second strip, count the P waves and multiply by 10 for atrial contraction rate (and R waves for ventricular contraction rate) 1,500 method: 1500 small squares = 1 min; divide 1,500 by the number o f small squares 300 method: same as for 1,500 method but 300 large blocks = 1 min 4. Rhythm: Regular/irregular? Paper and pencil method: For atrial rhythm use P-P intervals For ventricular rhythm use R-R intervals (or Q wave if R wave not present) Place ECG on a flat surface; position the straight edge of a piece of paper on the baseline; mark two consecutive R-R intervals and compare to successive R waves. If the distance is the same, then the rhythm is regular, if not, then it is irregular. 5 (1 large block) 6 7 8 9 10 (2 large blocks) 11 12 13 14 15 (3 large blocks) 16 17 18 19 20 (4 large blocks) 21 22 23 24 25 (5 large blocks) 26 27 28 29 30 (6 large blocks) 31 32 33 34 35 (7 large blocks) 36 37 38 39 40 (8 large blocks) 300 250 214 187 166 150 136 125 115 107 100 94 88 83 79 75 71 68 65 63 60 58 56 54 52 50 48 47 45 44 43 41 40 39 38 37 5. Axis A) Quick method: Left axis deviation (<-30°): leads I and III are ‘leaving each other’ Due to left ventricular hypertrophy (due to hypertension or MI for example) = conduction system problems Right axis deviation (>+90°): leads I and III are ‘reaching each other’ Hypertrophy = more muscle mass Due to right ventricular hypertrophy (due to pul oedema putting back Dilation = increased size but not muscle pressure on the R heart = cor pulmonale) = lung problems mass (ie HF) so no change on ECG B) Longer method: look at leads I, II, III, aVf: do +ve deflection - -ve deflection for each lead and use a pencil to plot each result in mm in this diagram 6. P wave (unlikely in 3rd year OSCE) best seen in lead 2 and V1 Is there a p wave? Yes = sinus rhythm or conduction problem o Is there 1 P wave/QRS complex? If no = heart block o Tall? Right atrial hypertrophy due to tricuspid stenosis o Broad? Left atrial hypertrophy due to mitral stenosis (may not be seen as pt may have AF too!) No = arrhythmia or hidden…is the pattern regular? Is the QRS complex wide? Skip to QRS 7. Duration of PR Interval Count # of small squares between start of P wave and start of QRS complex; multiply by 0.04s Is the duration within 0.12-0.2s? (3-5 small squares). Is it constant? If no, then will be heart block 8. Q wave = 1st –ve deflection Normally: not present or <1square Larger >1-2 small squares = previous MI Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php 9. Duration of QRS Complex End of PR interval to end of S wave; beginning and end of QRS complex and multiply by 0.04s Is duration between 0.08 an 0.12s (2-3 small squares)? Are all complexes same size and shape? Does a QRS complex appear after every P wave? pattern Irregular pattern Is it wide: > 0.12s (3 small squares) = VT or VF Normal QRS Regular SVT or atrial flutter AF o Is the pattern regular? Wide QRS VT VF Are there R and R’ waves? o left BBB = WiLLiaM o right BBB = MaRRoW Is it tall? (V1 or V2; whichever is biggest overall)+(V5 or V6; whichever is biggest overall) o Yes if >35 small squares = LVH due to hypertension, aortic stenosis, HOCM (in athletes) 10. ST segment – can not be seen if bundle branch block Elevated: artery occluded, plaque, clot, arrhythmias, areas downstream will die; acute MI (in any lead) or pericarditis; treat with clot blusters (streptokinase; old) or primary angioplasty Depressed: artery critically narrowed; cardiac ischaemia or acute coronary syndrome (eg non ST-elevation MI) or unstable angina). Treat with GTN spray, aspirin, O2, clopidogrel, angiogram, ?stent Distribution of infarct/ischaemia? Inferior (leads 1, 2, aVf); anterior (V1-4); lateral (leads 1, aVl, V5-6) NB. If see elevation in some leads, may see depression in the rest a. Changes to the ECG during MI process: normal ECG – then ST elevation (merges with T wave) = having an MI – T waves inverted = 12-14hrs after MI – T wave inversion increases, Q wave increases = MI 1 week ago – back to normal ECG but Q wave present = MI ages ago MI: need 2 out of 3 for diagnosis Ischaemia Increased troponin (partial MI) Use V2-6 Chest pain ST depression ST elevation (full thickness MI) T wave flattening/inversion Increased troponin 11. Evaluate T Waves Are T waves present? Do the T waves have the same deflection as the QRS complex? Tall/tented (no set value – judgement call): hyperkalaemia (3.5-5.1 normal; >6 = massively dangerous); artificially raised via sample waiting a long time to be processed, haemolysed sample? Do ECG to confirm with tented T waves. Do ABG as this gives an immediate reading too. Repeat bloods. Inverted: MI; ischaemia also (but not bad enough to cause ST depression) Flattened: MI, ischaemia 12. Determine duration of QT Interval (not for 3rd year OSCE) Count # of small squares between beginning of QRS complex and end of T wave; multiply by 0.04s Is the duration between 0.36-0.44s? (>10 small squares/2 large = problem) Congenital problem: long QT syndrome => ventricular arrhythmias => die suddenly; so screen family Electrolytes: hypokalaemic, hypo Ca2+, hypo Mg2+ (Mg and Ca usually change together) Drug side effects? Eg statin + pneumonia + clarithromycin = usually stop statin as may prolong QT interval 13. Check aVR: should be –ve; if not, ECG taken badly so request another one 14. Summary NB. A pacemaker usually sits in the right ventricle but may sit in left if there’s a septal defect Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php Conditions: Arrhythmias: due to Conduction system: left bundle branches into two smaller ones in ventricle (anterior, posterior), then Purkinje fibres are given off Heart itself Conduction system: When you look at an ECG, always look for P waves. If you can’t see any, it is most likely an arrhythmia. Is there a p wave? Yes = sinus rhythm or conduction problem No = arrhythmia or hidden…is the pattern regular? Is the QRS complex wide? 1. Is it Sinus Rhythm? To ascertain whether a rhythm is sinus or not you need to be able to identify key features. There must always be a p wave. The P wave should be a rounded shape Each P wave should be the same shape Each P wave should be followed by a QRS The P-R interval should be 3-5 small squares (<0.2s) and constant The rhythm should be regular. You do not need to be able to recognise a "T wave" for it to be sinus rhythm. Many abnormalities obscure the t wave. Suffice to say, if the patient is alive then the ventricles are definitely repolarising. 2. Sinus Arrhythmia Sinus Arrhythmia, or "regularly irregular" sinus rhythm, is a variation on sinus rhythm where the P-P interval (the distance between consecutive P waves) varies by more than 10%. It can be naturally occurring or due to heart damage. Causes can be: Respiratory-where the P-P interval lengthens and shortens with inspiration and expiration. Non-respiratory - where the process occurs seemingly for no reason. Sometimes seen in association with Complete Heart Block. Sinus arrhythmia is not commonly seen but the same evaluation procedure is used: Is there a P wave? Is each P wave the same shape? Is each P wave followed by a QRS complex? Is the P-R interval between 3-5 small squares? Is the rhythm regular? If the answer to the first four questions is "yes", but the answer to the last is "no" then you have sinus arrhythmia. 3. Sinus bradycardia: R-R intervals constant and regular All waveforms are present, and there is 1 P-wave to each QRS complex The rate is <60bpm but not usually <40bpm Patients usually asymptomatic and no treatment is required Bradycardia causes: sinus, athletes, meds (β-blockers, digoxin, Ca2+ channel blockers), when asleep 4. Sinus tachycardia: R-R intervals constant and regular Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php All waveforms are present, and there is 1 P-wave to each QRS complex Rate is > 100bpm, but not usually > 130bpm at rest Patient is usually asymptomatic. Tachycardia causes: exercise, low BP (eg haemorrhage/hypocolaemia), MI, CCF, hypoxia, stress, drugs, caffeine The passage of conduction through the heart in both sinus tachycardia and sinus bradycardia is exactly the same as in sinus rhythm. 5. Heart Block 1. 1st degree: PR interval prolonged as held up at AVN but steady; HR same; if asymptomatic, do nothing; early sign that other problems may develop such as a 2nd degree block! 2. 2nd degree: dropped QRS a. Mobitz type 1/Wenckebach: PR interval increases on each systole, then QRS dropped; possibly affect HR b. Mobitz type 2: Prolonged QT, constant: p-p-QRS (a 2:1 2nd degree heart block); p-p-p-QRS (a 3:1 2nd degree heart block); HR will decrease as a result, and may be SOB, fatigue, angina; treatment is to use a pacemaker rd 3. 3 degree: complete a. Regular p waves and QRS waves, but they are not co-ordinated with each other; ventricles rely on own pacemaker cells (ventricular pulse = ~30-40/min) ?hypotensive and HR decreases (and QRS complex may be wide too as pacemaker cells may be in left ventricle so left ventricle will contract before the right ventricle) 4. Bundle Branch Block – left or right BBB Left BBB: impulse travels down right bundle so right ventricle contracts before left Right BBB: impulse travels down left bundle so left ventricle contracts before right QRS is wide with secondary waves: cause an ‘M’ or ‘W’ shape: look at leads V1 and V6: If see W in V1 and M in V6 = wiLLiam = left BBB If see M in V1 and W in V6 = marrow = right BBB Arrhythmias: in the heart itself: When you look at an ECG, always look for P waves. If you can’t see any, it is most likely an arrhythmia. Is there a p wave? Yes = sinus rhythm or conduction problem No = arrhythmia or hidden…is the pattern regular? Is the QRS complex wide? Regular pattern Irregular pattern Normal QRS SVT or atrial flutter AF Wide QRS VT VF 5. AF No P wave; irregular irregular; often tachycardia To put back into sinus rhythm = two methods 1. Cardiovert: a. drugs: amiodarone or digoxin b. DC electric shock 2. Induce a bradycardia using a Β-blocker: metoprolol 6. Atrial Flutter Atria flutter at ~300/min; ventricles can only beat at ~220/min In 2:1 (atrial contraction: ventricle contraction) conduction, HR = 150/min. can also have 3:1 and 4:1. Hence ECG looks ‘sawtooth’ Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php Adenosine slows the HR so a flutter may become visible. If slower…see flutter wave 7. Supraventricular tachycardia (SVT) Due to an accessory pathway from the AVN HR usually 150-180/min and so look very much like sinus tachycardia or atrial flutter (Think: why does your pt have a sinus tachycardia of 150 if they’re lying in the bed?! Anxiety = ~110/min; sepsis = ~120/min; exercise = ~150/min…normally need to do serious exercise for HR to be that high…so unlikely to be sinus tachycardia of atrial flutter!) What to do: adenosine (decreases HR and causes a mini-MI, then the heart begins in sinus rhythm again; if atrial flutter, it’d go back to being a fast atrial flutter). Carotid sinus massage may also decrease HR as does pinch your nose and blowing through your ears, both working by increasing vagal tone and so decreasing HR. 8. Ventricular fibrillation A mess; no discernable pattern. Must be able to recognise immediately as it requires shocking the pt. the pt looks dead and will not be in VF if they are sat upright in their chair (a lead may have fallen off instead). 9. Ventricular ectopics: • VEs alternating with a normal QRS is called bigeminy Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php 10. Ventricular tachycardia: • VT is just a series of regular fast ectopics from a ventricular pacemaker 11. Defibrillator spike A vertical line before the QRS complex ALS information: Shockable rhythms = ventricular fibrillation and pulseless ventricular tachycardia Non-shockable rhythms = pulseless electrical activity and asystole Reversible causes of unconscious and not breathing person that must be ruled out before stopping CPR Hypoxia Hypovolaemia/haemorrhage Hypo/hyperkalaemia/hypocalcaemia (metabolic) Hypothermia – suspect in any pt who has drowned Toxicity/toxins Thrombosis – coronary or pulmonary – give thrombolytic drug; may need to continue CPR >90mins Tamponade – cardiac – typical signs = distended neck veins and hypotension Tension pneumothorax Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php Practise on spotting rhythms: Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php Practise on everything: Electrocardiogram (ECG) http://www.cvphysiology.com/Arrhythmias/A016.htm or ECGmadesimple.com or http://www.ecglibrary.com/ecghome.html http://www.nottingham.ac.uk/nursing/practice/resources/cardiology/function/5_12_lead_placement.php