HPI continued
advertisement
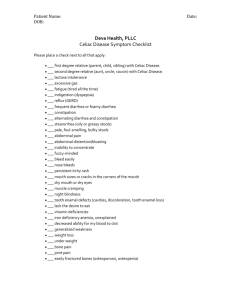
HPI 35 year old caucasian female presents to your clinic with 3 month history of diarrhea, bloating, and fatigue. What else would you like to know? HPI continued • • • • Patient states the diarrhea occurs daily, and that the stools are large and malodorous. She also states feeling embarrassed at work lately due to foul smelling gas, which has been occurring daily as well. She denies any nausea or vomiting, but notes feeling bloated daily, especially after meals. She notes losing about ten pounds since the diarrhea started, and denies any changes in diet or exercise routine. Her diet is true to her Italian roots, and consists of pasta and various meats and vegetables. Patient denies any recent travel, sick contacts, or illnesses. Medical history • Past medical history: Anorexia from age 18-22. • Past surgical history: appendectomy at age 7. • Medications: Daily multivitamin • Family History: Mother with hashimoto's thyroiditis. Father and paternal grandmother with hypertension. • Social History: Married and works as a second grade teacher. Denies smoking, alcohol, or illicit drugs. Physical Exam Vitals: Temp 98.6F, Pulse 105, Resp 20, BP 125/82 Gen: Thin appearing Caucasian female, in no acute distress. Cardio: Mildly tachycardic with regular rhythm. No murmurs, rubs, or gallops. Strong distal pulses. Abdominal Exam: Soft but mildly distended abdomen. Hyperactive bowel sounds. Moderately tender upon palpation diffusely. No organomegaly noted. Skin: Papulovesicular rash present on the extensor surfaces of both forearms. Psych: Alert and oriented to person, place, and time. Mildly anxious. What is on our differential diagnosis?? Differential Diagnosis -Irritable bowel syndrome -Inflammatory Bowel Disease -Crohn's Disease -Ulcerative Colitis -Infectious -Bacterial -Viral -Parasitic -Neoplasm -Lymphoma -Lactose Intolerance -Eating disorder relapse -Celiac Disease -What tests should we order? Labs WBC 10,000 (normal) Hgb 10.0 (low) BMP: K 3.0 (low), otherwise electrolytes within normal limits Iron Studies: -Serum iron: 40 mcg/dl (low) -Ferritin: 5 ng/ml (low) -TIBC: 600 mcg/dl (high) Fecal occult blood test: negative IgA tissue transglutaminase (tTg): 12.0 U/ml (positive) IgA endomysial antibody (EMA): present What should we do next? Upper endoscopy with small bowel biopsy Findings: -Blunting or loss of the villi -Hyperplasia of the crypts -Increased lymphocytes in the intraepithelial layer What is your diagnosis? Diagnosis: Celiac Disease -Also known as gluten-sensitive enteropathy Epidemiology -Estimated to affect 1 out of every 100-200 Americans. -Autoimmune, genetic, and environmental components -Associated with Down Syndrome, Turner Syndrome, autoimmune thyroid disease, and Type I Diabetes Pathophysiology -Gluten is a storage protein found in wheat, barley, and rye -It is broken down in the digestive system into peptides, including one called gliadin. Throughout a series of steps in predisposed patients, gliadin then can bind to antigen presenting cells in the small intestine, leading to inflammation and tissue damage unique to celiac disease. Clinical Presentation of Celiac Disease Adults o o o Usually diagnosed between 30-60 years old Most common symptoms include: diarrhea, bloating, abdominal pain, weight loss, and fatigue Other extraintestinal manifestations include: arthritis, iron deficiency anemia, dermatitis herpetiformis, and osteoporosis Children o o Usually diagnosed between 6 mo and 2 years of age, due to the introduction of cereal in this range. Common symptoms include irritability, diarrhea, failure to thrive, diarrhea, and abdominal distension Endoscopy Images of Small Intestine -Top left: Endoscopy photo of normal small intestine. -Top right: Biopsy of normal small intestine, showing numerous healthy villi -Bottom left: Endoscopy photo from a patient with celiac disease. Arrows pointing to characteristic "scalloping" of the folds of the intestinal mucosa. -Bottom right: Biopsy of small intestine with celiac disease. The villi are blunted and much less defined than the above healthy villi. Dermatitis herpetiformis -Pruritic papulovesicular rash found in roughly 10% of patients with celiac disease. -Classically, it is found on the trunk or extensor surfaces of arms and legs. -In addition to following a gluten-free diet, dapsone cream can also be prescribed to help clear the rash. -Histologically, dermatitis herpetiformis is confirmed by the characteristic IgA deposits in the subepidermal basement membrane. Treatment and Prognosis • • Following a strict gluten-free diet is the only treatment for celiac disease. The majority of patients have improvement in their symptoms if they strictly follow the dietary precautions. -Additionally by following the diet, they could potentially be decreasing the chance of more serious problems associated with celiac disease, including infertility, osteoporosis, and malignancy. • The cancer rate is higher in patients with celiac disease than in the general population. -Two of the most common types of cancer seen in patients with celiac disease include enteropathy-associated T-cell lymphoma and small intestinal adenocarcinoma. -If a patient continues to experience diarrhea, abdominal pain, or weight loss despite following the gluten-free diet, these more serious diagnoses should be in the differential.