CASE REPORT Dr Veselinka Djurisic - Institute for
advertisement

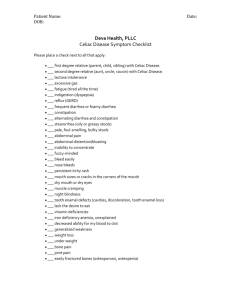
• Female infant, 8 month old; • Admitted to hospital due to: – Diarrhoea; – Metabolic disbalance; – With sings of enteropathy. History of Present Illness • 15 min before admission to hospital present with sudden abdominal cramping, cyanosis of limbs, she was lethargic, with drooping head. • Day before admision, she was sleepless, agitated, inconolably crying, with non bilious, non-projectile vomiting (4 times/day), and she had 10 regular stools. • 9 days before she was addmited to hospital due to vomiting, diarrhoea and high fever. Personal hystory: • Third child from regular pragnancy and term delivery completed with caesarean section. • Birth weight: 2830 g; Birth length: 53 cm; AS 9 • Breastfeeded 3 mo, after that continued adapted milk formula, 1 month later started mixed non-milk nutrition. • No history of allergy, regularly vaccinated Family history • Older brother – convulsions trated with AET; • Father – epilepsy; • Mother – chronic enteropathy in childhood suggested gluten free diet, but she refused; • Grandfather – COPD; Clinical finding • Weight 7 kg • Agitated, crying, groaning, dehydrated, afebrile (36,7⁰C), hemodynamically stable; • Vital sings: RR 36/min, CF 136/min, spO2 93%; • Skin: pale, marble, with limbs cyanosis. • Left torticollis, slight axial hypotonia. • Normal auscultatory findings of lungs and heart . • Abdominal examination: abdominal distension ,soft and nontender, without tumefacts and organomegaly. Laboratory findings Acido Base Balance Full Blood Count Coagulation status PT 16,7 s 10,1 INR 1,31 6,21 5,20 aPTT 21,2 s HGB 125 108 D – dimer 0,64 mg/l - 14,2 MCV 64 65 Fibrinogen 2,2 g/l 92,9% MCH 20 20,7 HCT 40% 34,2% PLT 835 376 pH 7,240 ESR 3 pCO2 3,65 kPa WBC 31,4 pO2 8,51 kPa RBC HCO3 11,5 mmol/l BE sO2 Biochemistry CRP 0,2 Glucose 3,0 Total protein 52 Albumin 30 Blood urea nitrogen 1,7 Creatinine 24 Sodium 135 Potassium 3,5 Calcium 2,13 AST 42 ALT 32 ALP 326 CK 82 LDH 327 AFP 1,5 Normal urin dipstick and sediment findings • Tissue transglutaminase antibody: – IgG 269; – IgA > 300; • Anti – gliadin antibodies: – IgG 6 ; – IgA > 300; Microbiology • Stool culture, ova and parasite testing, Rotavirus and Adenovirus: NEGATIVE. • Stool: positive for Candida sp. • Urin culture: negative. Radiology findings • X-ray plain film air-fluid levels Radiology findings • Ultrasound revealed mass suspected to intussusception in right hemiabdomen: Target sign (also known as the doughnut sign) Pseudokidney sign Radiology findings • Abdominal CT scan reveals dilated and fluidfilled loops of small bowel with air-fluid levels the classic ying-yang sign of an intussusceptum inside an intussuscipiens in right hemiabdomen. • Rectoscopy was performed: reveal normal. – The lining of the colon appears smooth and pink, with numerous folds. – No abnormal growths, pouches, bleeding, or inflammation is present. COURSE • Treated with antibiotics: – metronidazole – gentamicin • Corticosteroids: – methylprednisolone • H2 blockers: – ranitidine • Transfusion of fresh frozen plasma, 3 times • After exclusion of acute abdomen, cow protein free diet was introduced, but without any improvement. • Spontaneus desinvagination. • After obtainig coeliac serology, gluten free diet has started, occurs clinical improvement with metabolic stabilisation. Conclusion • Case of rare but serious clinical presentation of celiac crisis. • It is important to recognize that CD may present in “crisis.” • The possible precipitating factors in present patient are unrecognized coeliac disease, hypokalemia and previous infection. Discussion • Incidence of celiac disease is on rise in Montenegro. • Prevalence of CD is found to be........ dopuniti ukoliko postoje podaci..... • Celiac crisis is a life-threatening complication of CD. • Clinically, it is characterized by severe diarrhea, dehydration and metabolic disturbances like hypokalemia, hypomagnesemia, hypocalcemia, hypoproteinemia and metabolic acidosis. Definition of celiac crisis • Acute onset or rapid progression of gastrointestinal symptoms attributable to celiac disease requiring hospitalization and/or parenteral nutrition along with at least 2 of the following: Signs of severe dehydration including: hemodynamic instability and/or orthostatic changes Neurologic dysfunction Renal dysfunction: creatinine >2.0 g/dL Metabolic acidosis: pH <7.35 Hypoproteinemia (Albumin < 3.0 g/dL) Abnormal electrolytes including: hyper/hyponatremia, hypocalcemia, hypokalemia or hypomagnesemia Weight loss > 10 lbs Metabolic pathophysiology in celiac crisis • Celiac crisis may not respond to a gluten-free diet alone. In severely ill children with celiac crisis, the use of corticosteroids may cause dramatic improvement. * • Lloyd-Still described 3 cases of celiac crisis successfully treated with corticosteroids. ** • The role of steroids now is controversial as gluten free and good nutritional diet are considered good enough to tide over the crisis *** * Mihailidi E, Paspalaki P, Katakis E, Evangeliou A. Celiac Disease: A Pediatric Perspective. International Pediatrics 2003;18:141-8. ** Lloyd-Still JD, Grand RJ, Khaw KT, Shwachman H. The use of corticosteroids in celiac crisis. J Pediatr. 1972; 81: 1074-1081. *** Walia A, Thapa BR. Celiac crisis. Indian Pediatr. 2005; 42: 1169 Grazie per l'attenzione Saluti da Montenegro